Introduction
The May Thurner Syndrome (MTS) is a clinical condition as a result of an anatomical compression of the left common iliac vein (LCIV) by the fifth lumbar vertebra posteriorly and by the right common iliac artery (RCIA) anteriorly associated with symptomatology. This phenomenon can cause venous stasis in the pelvis and left lower limb and can be precursor of a deep venous thrombosis. The association of other venous compression like Nutt- Cracker syndrome can enhance this venous stasis1.
From an historical perspective this syndrome was first described by Virchow, in 1851, who noticed that there was a predominance of iliofemoral deep vein thrombosis (DVT) on the left lower limb, reaching a frequency 5 times higher, in relation to the right lower limb. He defined the syndrome as a repetitive and chronic compression of LCIV by the RCIA, with the consequent development of synechiae inside the LCIV. In 1908, Mc Murrich, (in a cadaveric study, observed internal adhesions in the common iliac veins and postulated that these were congenital and responsible for the highest incidence of DVT2. In 1943, Ehrich and Krumbhaar observed that 23.8% of adults had intravenous lesions in the LCIV and the histological analysis showed that they consisted of elastin and collagen, showing that the lesions were acquired and not congenital3.
In 1957, May and Thurner examined 457 cadavers and observed lesions in the LCIV in 22% of the cases, classifying them as spurs, dividing them into 3 types(4, 5). In 1965, Cockett and Thomas described the first clinical series of 57 patients with acute ilio-femoral DVT, secondary to LCIV compression by the RCIA6.
Precise diagnosis and quantification of the compression are key elements to a successful treatment in this young population. The diagnosis is based on the association of symptoms and the interpretation of imaging tests such as CT or MR. However, sometimes there are disagreements in the interpretation of these exams and this must be solved.
Clinical case
A 43 old man with a past history of a deep venous thrombose of the left lower limb 13 years ago following an inguinal hernioplasty, presented with a long history of left limb edema and inability to stand up for long periods of time. These symptoms deteriorated in the previous five months disabling him from working.
The physical examination showed global edema of the left lower limb associated with venous dermatitis in the medial malleolar area.
A venous ultrasound was performed which revealed reflux of the left popliteal vein, the great saphenous vein and the small saphenous vein.
A venous-CT scan was done but lead to a disagreement between the radiologist report, stating no relevant compression of the left common iliac vein by the right common iliac artery and the vascular surgeon's assesment. (Image 1 )
A phlebography and an endovascular ultrasound (IVUS) was then performed which confirmed the compression (Image 1).
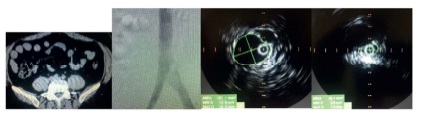
Image 1 Venous-CT, phlebography and IVUS that shows severe compression of the left common iliac vein by the right common iliac artery side.
The patient was anticoagulated. An Abre 16/80 stent (medtronic) was implanted with posterior dilation with a 16/4 balloon (Boston Scientific). The phlebography and endovascular ultrasound control showed complete resolution of the compression. (Image 2)
In the postoperative period, the patient maintained anticoagulation with LMWH and intermittent pneumatic compression of the lower limbs, being discharged at 24h with oral anticoagulation (DOAC- rivoroxaban) and elastic stockings.
At 3 months follow-up, the patient was asymptomatic and had resumed his work.
Discussion
The diagnosis of MTS demands a high degree of clinical suspicion, as the symptoms can be associated with such clinical as superficial venous reflux, post-thrombotic syndrome and primary lymphedema6.
The lower limb venous doppler ultrasonography is the first line exam because it is non-invasive and simple to perform. However the visualization of common iliac veins is technically difficult, deeming the exam not sensitive enough to detect LCIV compression or their intraluminal defects. At least 20% of the iliac vein ultrasound studies performed are not diagnostic7. The Doppler ultrasound is of great value in the evaluation of infra-inguinal venous disease, a very prevalent disease.
If no anomaly is found at this level or the anomaly does not justify the clinical picture, the ilio-cava sector should be studied with CT or MRI. CT and MR are the exams of choice for the study of SMT8. In addition to allowing the demonstration of direct compression of LCIV by the RCIA and the compensatory collateral circulation, they can also exclude extrinsic compressions, such as tumors, hematomas or retroperitoneal fibrosis. CT scan is the most used exam in this diagnosis due to its availability and lesser time consumption. MRI is less available and therefore less routinely used. However, it easily demonstrates the area of compression or obstruction and the existence of collateral circulation9-11.
Phlebography by puncture of a vein in the foot is insufficient to obtain a good visualization of the femoral-ilio-cava venous sector. Phlebography by femoral puncture is usually performed. In addition to demonstrating LCIV compression, demonstrates collateral venous circulation and allows measuring the pressure gradient induced by the obstruction. This gradient must be greater than 2mmHg, at rest, and 3mmHg, after exercise12,13. However, there is currently no hemodynamically credible test to target the degree of venous obstruction and the hemodynamic improvement after stenting.
Intravascular ultrasound (IVUS) is a more recent exam that can measure the size of the vessels, the internal morphology of the vessel and the degree of stenosis, as well as facilitating the accuracy of stent implantation8,14. Forauer et al stated that its use interfered with the endovascular treatment of SMT in 50% of the cases15. Montminy M. et al stated that phlebography when compared with IVUS fails to identify a lesion in 19 % of the cases and misses the location of maximal stenosis in more than two-thirds of the limbs16. As observed in our clinical case, the IVUS allowed us to increase the accuracy of the diagnosis and to improve the adequacy the ilio-cava stenting. So IVUS has revealed an increasing utility in confirming the diagnosis and helping to improve the therapeutic quality in the endovascular treatment of SMT17. However, the acquisition cost has limited the availability of de IVUS.
Endovascular surgery revolutionized the treatment of obstructive venous disease, due to its low physiological aggressiveness, high safety, good efficacy and a complication rate lower than 2%18-21. Osman Ahmed et al in a recent review of his experience in the endovascular treatment of SMT, reported a a technical success of 100%, with no major complications and a complication rate of less than 5%22. Wan-Yin Shi et al23 published their experience with the endovascular treatment of SMT, in 233 patients, referring a technical success in its uncomplicated form of 98.5%. Machado M. et al24 reports in the endovascular treatment of MTS a technical success of 100%, a primary patency of 85.7% and an assisted primary patency of 100%.
The ilio-caval stenting became the gold standard for the treatment of MTS.