Introduction
The thoracic aorta is the most commonly involved aortic section when acute aortic dissection (AD) occurs. It may also extend to the abdominal aorta1. However, acute isolated abdominal aortic dissection (IAAD) is a relatively rare event, representing only 1% to 4% of the AD cases, with only 18 cases reported in the International Registry of Acute Aortic Dissection (IRAD) between 1996 and 20032,3. It can occur spontaneously or in association with trauma and surgical procedures (especially endovascular)4-6. The association with atherosclerosis or an iatrogenic etiology is stronger for acute IAAD than for classical Stanford type B AD. Acute IAAD most commonly presents with abdominal pain, visceral ischemia (including acute renal failure) and limb ischemia. Mean reported age of presentation is 67.7 ± 13.3 years2, similar to that of classical type B aortic dissection. Medically treated chronic dissection tends to progress with aneurysmal degeneration. Due to wall weakening induced by chronic dissection, with higher rupture risk, many surgeons advise earlier intervention in dissecting aneurysms, usually when they reach a diameter of 3 cm1,6,7. In result of the scarcity of reported cases, management of IAAD is still a matter of controversy. We describe a series of eight cases of IAAD who underwent surgical treatment. These cases occurred during a time frame of 13 years and no other cases of IAAD were described in our institution during this period.
Methods
This is a single center, retrospective, observational, study of patients with IAAD who were treated with open or endovascular surgery. All patients diagnosed with IAAD and treated during the period comprised between 2008 and 2021 were included. The deJned primary outcome was early mortality (<30 days). Secondary outcomes analyzed were complication and reintervention rates. Statistical analyses were performed using SSPS software (Statistical Package for the Social Sciences, version 20.0, SSPS Inc, Chicago, IL, USA). Results were expressed as mean ± standard deviation (SD), or median ± interquartile range (IQR).
Results
A total of eight patients (four males and four females) were diagnosed and treated for IAAD between 2008 and 2021 in our Institution. Median follow-up was 6,2 years (2 months-13 years). Median age at presentation was 78 (IQR= 58.2 - 84.5) years and all patients were asymptomatic. Hypertension had a prevalence of 50% and half of the patients were current or former smokers. Median aortic diameter at presentation was 30mm (14-85mm).
All but one patient underwent endovascular treatment, this patient was a young (68 years) good risk patient who underwent open surgery (aortobiiliac bypass). Three patients were treated with bifurcated aortic endografts, three patients had a single stent-graft (iliac limbs of aortic endografts) implanted and one patient underwent a CERAB procedure for coexistent stenotic disease of the aortic bifurcation.
Of the patients treated withonly one iliac limb (Fig 1) one had IAAD of a short infrarenal aortic segment with enough proximal (infrarenal) and distal (above the aortic bifurcation) neck lengths (Fig 2 and 3) and the other two had small aortic dissecting aneurism with similar, favorable, anatomic conditions.
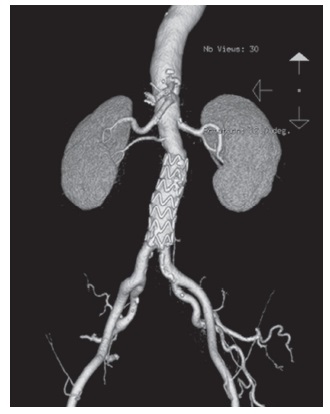
Figure 1 Saccular dissecting aortic aneurysm treated with an Endurant II (Medtronic Vascular, USA) iliac limb 20×80mm trimmed down to 70mm length.

Figures 2 and 3 Isolated abdominal aortic dissection with aneurysmal degeneration with saccular morphology.
There were no perioperative deaths or early postoperative complications. Late reintervention was needed in one patient. During the 8th year post-EVAR this
patient had a routine follow-up CTA which revealed an endoleak (suggestive of type III EL) and growth of aneurysm diameter. Repeated EVAR was chosen to treat this late complication, intraoperative angiography revealed a type Ia endoleak which was treated with an aorto-uni-iliac stent graft (to ensure that a possible associated type III EL would be treated as well) and cross-over femoro-femoral bypass. Two early surgical reinterventions were performed to drain groin hematomas after this surgery. At the 12th year of follow-up (four years after reintervention), the patient was asymptomatic and angioCT showed aneurysm diameter stabilization without endoleaks.
Discussion
Treatment strategies for acute IAAD include open surgery, endovascular intervention or medical treatment. The results from a meta-analysis published by Jonker et al8 suggest that an early aggressive (open or endovascular surgery) may be associated with improved survival. However, this is a retrospective study with only 19 patients treated with endografts, therefore, in our institution, we still manage the AIAAD with medical treatment and treat these patients in case of ischemic complications.
Despite the good historical results described for open surgery,1,2,6) especially in good risk patients, the evolution of endovascular therapies has allowed the effective treatment of high operative risk patients with good long-term results9,10). In fact, the excellent results obtained by some centers supports endovascular techniques as the Jrst-line treatment in all patients given the presence of adequate anatomy10. Our series includes one patient that was preemptively treated (asymptomatic and without aneurysm degeneration), and this is somewhat controversial, however, it was decided to perform the surgery considering the patient's reduced risk and the low risk and complexity of the procedure itself. In fact, a recent large meta-analysis11 of 482 patients confirmed a low long-term mortality with a surveillance strategy offering surgery for patients who develop symptoms or an aneurysm, however, this same publication underlines the signiJcant rate of late intervention (18%) and also the low mortality rate of patients who underwent endovascular treatment (2%). Moreover, a retrospective study of more than 200 patients treated conservately and followed with routine angioCT showed that only 1.4% of the patients had positive aortic remodeling with medical therapy alone12.
In our opinion, this may justify a low threshold for intervention in patients with IAAD as long as they are good candidates for endovascular treatment.
We describe the treatment of three patients with a single stentgraft (all of them with iliac limbs from conventional aortic endografts), this is closely related to the fact that early intervention in infrarenal IAAD (but after the acute phase) is facilitated by the presence of a normal size aorta at the infrarenal neck and above the aortic bifurcation. This surgical strategy has the advantage of a single, lower proJle, vascular access a shorter procedure duration and preserves the native aortic bifurcation allowing easier future endovascular or open reinterventions.
This is a retrospective study with a small number of patientswhich limits the external validity of its Jndings.
Conclusion
Infrarenal IAAD is a rare pathology and precise clinical indications for treatment in asymptomatic patients are, therefore, unknown. In patients with adequate anatomy endovascular treatment is safe and effective as our case series, and other published works, shows. In some patients with short segment dissections tailored treatment with short stent-grafts may allow a simple, low risk, approach. Early, post-acute, intervention may be warranted in all cases (even asymptomatic) considering the low risk of complications in this group of patients.














