Introduction
Renal cell cancer (RCC) is relatively rare and represents only 3.1% of all adult cancers.1 Extension to the venous system is a feature of cancer progression; however, at diagnosis, venous tumour thrombi are present in only 4-10% of cases.2 The surgical management of renal cancer with tumour thrombi has evolved substantially since it was first documented in 1913, with the first excision of an intracardiac neoplastic thrombus performed under cardiac bypass in 1970.3 Radical nephrectomy alone, the only option previously available, has a poor prognosis with the majority of patients dying within a year. The addition of inferior vena cava (IVC) tumor thrombectomy improves quality of life, prevents symptoms of venous congestion, decreases oncologic-associated morbidities, and can often achieve complete cure and extend survival. The surgical strategy for IVC tumor thrombectomy depends on the limit of thrombus extension, tumor size, hemodynamic risk factors, as well as infiltration into the IVC wall.4 The authors evaluated the institutional experience of a tertiary center in the surgical management of RCC patients with tumour thrombi invading the IVC.
Methods
Retrospective analysis of a single-center consecutive series of patients with RCC and IVC tumour thrombi treated with surgery in our department between 2012 and 2021 was carried out. Demographic data, diagnostic and procedural characteristics, clinical outcomes and survival analysis were examined.
Patient characteristics: We selected patients who received surgeries for RCC with caval thrombi in our center between 2012 and 2021. The following data were examined retrospectively: sex, date of birth, data of surgery, comorbidities such as smoking status, arterial hypertension, diabetes mellitus, dyslipidemia, acute coronary syndrome or previous stroke, the ASA physical status classification system, tumour size, thrombus localisation and extension in the IVC, the TNM stage, histopathological classification, tumor size, surgical approach, peri-operative blood loss, operative time, pre- and post-operative kidney function, duration of hospitalisation in the intensive care and in the hospital, number of red blood cells units and number of fresh-frozen plasma units received by the patients, post-operative complications, reinterventions, recurrence, adjuvant treatment, 30-day mortality, time of follow-up and patient survival.
Thrombus extension was determined using computed tomography (CT) and was classified on the basis of the classification system of Neves as follows: level I - tumor thrombus in the renal vein or ≤2 cm from the confluence of the IVC and renal vein, level II - thrombus within the IVC >2 cm from the confluence of the IVC and renal vein and below the hepatic veins, level III - thrombus involving the intrahepatic IVC, and level IV - thrombus above the diaphragm.5
Workup: The pre-operative evaluation for all patients involved a clinical exam and laboratory tests as well as thoracic, abdominal and pelvic imaging studies through a CT-scan.
Operative details: The surgical approach was determined by the superior limit of the venous thrombus. For stage I and II extent, an abdominal approach with a subcostal incision allowed for resection of the thrombus in the retro- and suprahepatic vena cava. For stage III and IV diseases, access to the supradiaphragmatic vena cava was necessary. For stage III disease, this access was achieved either through an abdominal approach, a thoraco-diaphragmatic laparotomy or medial abdominal or subcostal incisions with sternotomy; For stage IV disease, access to the right atrium required a systematic sternotomy and systematic intervention in the Cardiac Surgery Department.
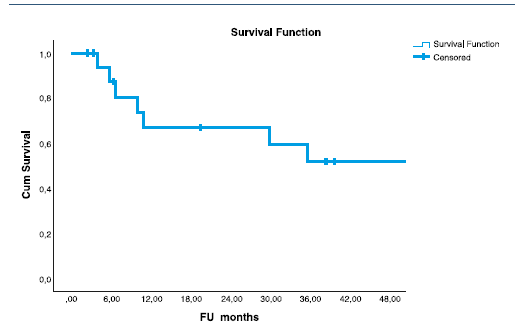
Statistical analysis: All patients were followed from diagnosis until death or until data were censored (and the patient was considered to be alive). Descriptive statistics was used for patients caracheristics. Overall survival was evaluated from the date of surgery to the last follow-up visit or death. Kaplan-Meier survival curves were calculated using censured data and compared by the log-rank test. A p-value of less than 0.05 was considered significant. All tests were carried out with the program SPSS® v22.0.
Results
Patient characteristics: A total of 18 patients underwent primary IVC repair for RCC tumor thrombus between 2012 and 2021. Among the patients, 16 were men and 2 were women. Of these 33% (n=6) had smoking history, 78% (n=14) hypertension, 33% (n=6) diabetes and dyslipidaemia. Mean tumour size was 8.78 ± 2.47cm (3-12cm), and 67% (n=12) of the cases were renal clear cell adenocarcinoma. On the basis of the Neves classification for IVC thrombus extension, 39% (n=7) of the patients had level I; 28% (n=5) level II; 17% (n=3) level III and 17% (n=3) level IV. Clinical and histopathological characteristics are presented in the Table 1.
Table 1 Clinical and histopathological characteristics of patients and tumours
| N | |
| Sex Male Female | 16 (89) 2 (11) |
| Smoking History | 6 (33) |
| Arterial Hypertension | 14 (78) |
| Diabetes Mellitus | 6 (33) |
| Dyslipidaemia | 6 (33) |
| Histology - Clear Cell carcinoma | 12 (67) |
| Stage of thrombus according to Neves Classification I II III IV | 7 (39) 5 (28) 3 (17) 3 (17) |
Intraoperative variables: The majority of the patients underwent en bloc radical nephrectomy, with cavotomy and vena cava thrombus removal followed by lateral venorrhaphy of the vena cava (88.9%, n=16). In one patient, infra-renal IVC ligation was performed, and in another IVC interposition with PTFE and a prosthetic-renal bypass. In level IV, combined open sternotomy and cardiac bypass was necessary for RA thrombus control. Mean total operative time was 3h4min ± 1h19min and median intraoperative blood loss was 600ml requiring a median blood cells transfusion of 3.5units (min = 0, max = 16) during the hospital stay. There were no intraoperative deaths.
Post-operative and long-term follow-up: 16 of the 18 patients were transferred to the intensive care unit (ICU), with a median ICU stay of 2 days (min = 0, max = 14) and subsequently transferred to the vascular surgery department for a median total hospital stay of 8 days (min = 4, max = 61). The mean preoperative serum creatinine was 1.23+0.38 mg/dL. After surgery, there was observed a mean decrease of serum creatinine of 0.001 mg/dL (p=.991) (paired T test), confirming the absence of renal impairment. Only one patient required reintervention in the post-operative course for splenectomy. Post-operative complications included one case of pulmonary embolism, pneumonia, acute coronary syndrome and two cases of temporary acute renal lesion, but none required renal replacement therapy. There was no 30-day mortality. Five patients underwent adjuvant chemotherapy. Median follow-up time was 19.5 months (6-46.2 months). The four-year overall survival rate was of 52% (Figure 1).
Global survival curve for 18 patients after surgical treatment for renal cell carcinoma extending into the vena cava.
Discussion
Radical nephrectomy and tumor thrombectomy are known to be the most effective treatment methods in patients with RCC and tumor thrombus extending into IVC.6 The survival of RCC patients who had involvement of the vena cava by tumor thrombi over the last twenty years has already been described. The rate of overall survival in our study, 52% at four years, was similar to rates that have been documented in previous studies.7,8,9,10,11,12 All previous studies are retrospective, are based on long periods (10-30 years) and have small sample sizes. Despite the weak evidence in these studies, they enable us to better comprehend these rare cases in terms of morbidity and mortality and give us an idea of the prognostic validity of venous involvement. The published studies are heterogeneous and, in some cases, cover periods in excess of 20 years, but the true survival rate for all stages is on the order of 45% after five years.
Management of renal cell carcinoma with caval thrombus should be a multidisciplinary approach. Management of these patients should be a team approach. Moreover, adequate preoperative workup is the key to a safe and successful surgical outcome. At our center, medical, cardiac, and anesthetic preoperative consultations are mandatory. The presence of thrombus in cava, in patients with renal tumor, poses very varied problems of surgical strategy. Fundamental factors to choose the surgical approach are 1) the extension of the thrombus in the vena cava; and 2) potential adhesions or infiltration of the vessel wall by the tumor. For example, renal cell carcinoma with a tumor thrombus extending into the supradiaphragmatic inferior vena cava and right atrium represents a challenge to the surgical team with the need of cardiopulmonary bypass (CBP). After nephrectomy we used CPB to cool the patients to 20 degrees celsius and decreased the flow to 500 ml/min/m2. The heart went into spontaneous ventricular fibrillation without using cross clamping and cardioplegia. Then we did atrial and inferior vena caval thrombectomy in a bloodless and visible operation field within a safe time interval. The aim of using this technique is to prevent myocardial injury and to protect the brain from hypoxia by using this low flow technique. This method can be used safely for the management of renal cell carcinomas and for some retroperitoneal malignancies associated with vena caval and atrial involvement.13 Given this multidisciplinary approach, we feel the best option for patients with renal cell carcinoma with tumor thrombus of the vena cava is referral to a high-volume center where all specialties involved have some degree of experience in dealing with these patients. We believe that this multidisciplinary approach is critical for minimizing complications related to radical nephrectomy with vena cava thrombectomy.13