Introduction
Venous iliofemoral obstructions can cause debilitating symptoms interfering with daily activities and decreasing patients’ quality of life. In the recent past, the most promising treatment consisted of pain medication, compression stockings and anticoagulation.1
Endovascular recanalization of venous obstructions emerged as a revolutionary procedure with good results having been reported. Initially, treatment was performed with stents developed for the arterial system.2 However, these stents show specific characteristics to overcome the negative effects of atherothrombotic plaques. In the venous system, the main pathophysiologic issue consists of intraluminal vein scarring and is not related to atherothrombotic plaques. Subsequently, dedicated venous stents were developed with favorable features for the venous system, which main goal is to counter extraluminal compression.3,4
Venous obstructions occur as a result of deep venous thrombosis, post-thrombotic syndrome or non-thrombotic iliac vein lesions, all eligible for endovascular treatment. However, the type of original venous obstruction seems to influence the stent-related outcomes.
The aim of this review is to report on the impact of venous stent patency loss, as well on risk factors and management.
Methods
A systematic review was conducted according to the recommendations of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement. The literature search was last updated in April 2021.5
Search strategy: Using the Medline and Cochrane databases, the following query (((("Endovascular Procedures" [MeSH Terms]) OR ("Endovascular Procedure*"[Title/Abstract])) OR ("Intravascular Procedure*" [Title/Abstract])) OR ("Intravascular Technique*" [Title/Abstract])) OR ("Endovascular Technique*" [Title/Abstract]) AND (((("May-Thurner Syndrome" [MeSH Terms]) OR ("May-Thurner Syndrome" [Title/Abstract])) OR ("Iliocaval Compression" [Title/Abstract])) OR ("Cockett Syndrome" [Title/Abstract])) OR ("Iliac Vein Compression" [Title/Abstract]) AND ((("Postthrombotic Syndrome" [MeSH Terms]) OR ("Postthrombotic Syndrome" [Title/Abstract])) OR ("Venous Stasis Syndrome" [Title/Abstract])) OR ("PTS" [Title/Abstract]) AND ((((((((("Venous Thrombosis" [MeSH Terms]) OR ("Venous Thrombosis" [Title/Abstract])) OR ("Phlebothrombos*" [Title/Abstract])) OR ("Venous thrombos*" [Title/Abstract])) OR ("Deep Vein Thrombos*" [Title/Abstract])) OR ("Deep-Venous Thrombos*" [Title/Abstract])) OR ("Deep-Vein Thromboses" [Title/Abstract])) OR ("Deep Venous Thrombos*" [Title/Abstract])) OR ("DVT" [Title/Abstract]) was used for online search.
Eligibility criteria included any publication reporting on iliofemoral venous stenting patency. Exclusion criteria were 1) articles published before 2000, 2) language other than Portuguese or English, 3) studies in paediatric age and cancer, and 4) not human research.
Data extraction and assessment of study quality: Two reviewers (A.S., C.N.) were responsible for study selection, data extraction, and study quality assessment. Data collected and analyzed included year of publication, type of study (classified as case control, observational retrospective, observational prospective, and randomized control trial [RCT]), type of stent, number of patients in the cohort, rate of stenosis/occlusion, follow up (in months), clinical presentation, identified risk factors, treatment, and outcome.
Results
Initially a total of 952 potentially relevant articles were selected. After reviewing the records at title or abstract level, 71 articles were read in full and 12 were judged eligible for inclusion, discussing 1981 patients (Figure). These included one prospective single center study, one prospective multicenter study and 10 retrospective single center studies. Studies characteristics, population, stents used, and antiplatelet regimen are available in the Table.
Indication for stenting included DVT (4%), PTS (18.8%) and NIVLs (77.2%). A total of 1807 patients were initially submitted to angioplasty and stenting, and in 174 adjuvant thrombolysis was performed.
A total of 10 studies presented an estimated incidence of stent occlusion, ranging from 0% to 19.9%, affecting 81 patients. A total of 5 studies presented an estimated incidence of in-stent stenosis, ranging from 0% to 32.2%. Follow-up strategies included clinical and imaging control with a mean follow-up of 19.7 months.
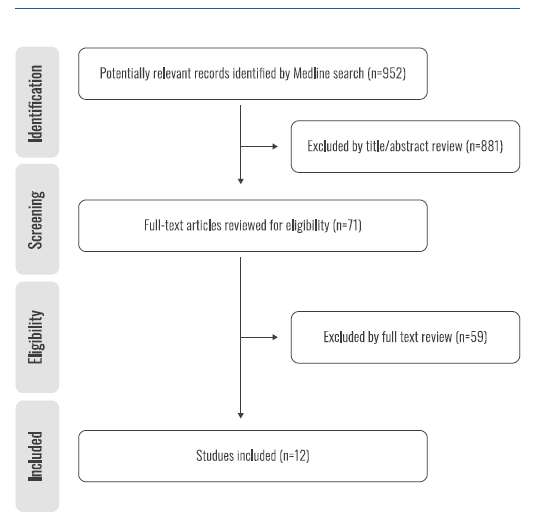
Figure. Preferred reporting items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram summarizing the literature screening process for studies referring to venous stent patency.
Post-thrombotic femoral leg inflow veins was associated most frequently with stent failure. Other risk factors included incomplete thrombolysis, male gender and age younger than 40 years. Stent placement below the inguinal ligament, type of stent and anticoagulation regimen do not seem to affect stent patency.
Post-procedural stent re-stenosis was reported in 121 limbs (5.1%) and stent occlusion in 81 limbs (3.4%); the latter was distributed as follows: 11.1% after DVT, 77.8% PTS and 11.1% NIVLs. Considering stent failure treatment, several treatment alternatives were considered. Conservative management was an option in 25 patients (12.4%), who were all clinically asymptomatic. A total of 186 re-interventions were performed in symptomatic patients which included angioplasty, thrombolysis, re-stenting, thrombectomy and arteriovenous fistula construction.
Table. Analysis of study characteristics, population, type of stent and antiplatelet regimen
| Article (Year) | Study design | Population | Age | Female/male ratio | Sample size | Stent type | Antiplatelet regimen |
| Knipp 2007(6) | Retrosp; Single centre | NIVL | Median 39 (range 17-71) | 6.25 | 58 | not mentioned | Warfarin or Clopidogrel ± Aspirin ("variable period", 6 wk) |
| Husmann 2007(7) | Retrosp; Single centre | NIVL | Median 34 (16-64) | 4.5 | 11 | Wallstent (Boston Sientific) | Initially LMWH and swith to VKA (6 mon) |
| Srinivas 2015(8) | Prosp; Single center | Acute iliofemoral DVT | Mean 42,1 ± 10,8 | 1.7 | 8 | Wallstent (Boston Sientific); SMART Stent (Cordis) | Warfarin (12 mo) |
| Langwieser 2015(9) | Retrosp; Single centre | PTS | Mean 32 ± 11 | 3.5 | 9 | Nitinol self-expandable stent | Rivaroxaban 20mg + Clopidogrel 75mg (6 mon) then Rivaroxaban 20mg or Aspirin only (after 6 mon) |
| Vuuren 2017(2) | Retrosp; Single centre | PTS and NIVL | Mean 43,2 ± 14,5 (RANGE 17-81) | 1.9 | 200 | Sinus Venous (OptiMed) | not mentioned |
| Haqq 2017(10) | Retrosp; Single centre | NIVL, acute DVT and PTS | Mean 42,4 ± 18,1 | 2.0 | 70 | PTS patients received anticoagulation ("long period"), most NIVLs patients received anticoagulation (3 mo), switch to MAPT/DAPT (6 wk) | |
| Jayaraj 2018(11) | Retrosp; Single centre | PTS and NIVL | not mentioned | not mentioned | not mentioned | Wallstent (Boston Sientific); Z-stent (Cook) | DOAC + Aspirin + Cilostazol (≥3 mon) |
| Menez 2019(12) | Retrosp; Single centre | PTS | Median 41 (17-86) | 0.6 | 95 | Cook Zilver (Cook); Sinus XL Flex (OptiMed); Wallstent (Boston Sientific) | Aspirin (75-100mg) + Warfarin or DOAC (1 mo), Warfarin or DOAC (3-6 mo) |
| Sebastian 2019(13) | Prosp; Multi center | NIVL, acute DVT and PTS | Median 43 (31; 56) | 0.9 | 136 | Sinus XL Stent (optimed), Venovo (bard); Sinus Obliquos (optimed), VICI Venous (Boston Scientific); Sinus XL Flex (OptiMed), Zilver Vena Stent (Cook), BlueFlow (admedica); Sinus Superflex stent (optimed), BlueFlow (abdmedica) | Vitamin K antagonist or DOAC |
| Chait 2019(1) | Retrosp; Single centre | NIVL | Median 66 (21-99) | 1.9 | 1061 | Wallstent (Boston Sientific) | Clopidogrel 75mg or previous anticoagulation (3 mo) |
| Avgerinos 2019(14) | Retrosp; Single centre | Acute iliofemoral DVT | Mean 45,8 ± 17,2 | 1.7 | 73 | Wallstent (Boston Sientific); Protégé stent (ev3 Endovascular Inc.) | VKA/DOAC/LMWH + Aspirin/Clopidogrel (≥3 mo) |
| Bondarev 2019(15) | Retrosp; Single centre | NIVL | Mean 47 ± 15 | 13.8 | 59 | Wallstent (Boston Sientific); SMART Stent (Cordis) | not mentioned |
PTS - Post Thrombotic Syndrome; NIVL - non-thrombotic iliac vein lesions; DVT - Deep Venous Thrombosis; LMWH - Low Molecular Weight Heparin; VKA - Vitamin K Antagonists; DOAC - Direct Oral Anti-Coagulant; MAPT - Mono Anti Platelet Therapy; DAPT - Double Anti Platelet Therapy.
Primary, primary assisted and secondary patency rates at one year ranged from 68-100%, 79-90% and 85.8-100%, respectively. Anticoagulation duration after stenting ranged from 1-12 months with no difference between direct oral anticoagulants and vitamin K antagonists, supplemented with antithrombotic therapy.
In one study involving only patients treated for NIVLs, no anticoagulation was prescribed and antiplatelets therapy was continued for three months. The Villalta score was reported in six studies, with a score improvement in all cases.
Discussion
Venous stent failure is still a poorly understood phenomenon. Endovenous recanalization is a relatively recent treatment alternative for venous outflow obstructions and only in the last few years have venous stents been developed. The most widely accepted definition of venous in-stent stenosis is diameter stenosis ≥50% in the stented vessel segment. Stent occlusion is defined as a complete absence of blood flow in the stented vessel segment.
The most common risk factor for stent failure was the presence of thrombotic inflow veins. The majority of stent occlusions were observed in PTS limbs and this can be explained by the fact that venous inflow in PTS patients is more compromised because of intraluminal scarring below the femoral vein.2
The different types of stents used did not seem to influence patency rates, even though in the literature patency varies according to different stents. Because dedicated venous stents have been available for only the past few years, there is currently lack for large comparative studies.16,17
All patients were kept under anticoagulation, with the exception of one study that involved patients treated for NIVLs without venous thrombosis, that were kept exclusively under antiplatelet therapy. In these patients, all stent failures occurred within 6 months. Iliac veins stents placed for venous thrombosis, however, had continued stent failure after 6 months, supporting the role for extended surveillance in this group of patients.10 Antiplatelet regimens are still not uniform among different studies. Anticoagulation seems preferable to antiplatelet therapy for the first months. Regarding duration of anticoagulation, discontinuing anticoagulation in patients with NIVLs after 6-12 months seems consensual if the stent appears patent on ultrasound. The role of antiplatelet agents following venous stenting appears to be unclear.18 Eijgenraam et al. reported antiplatelet use in venous stenting procedures; although antiplatelets have been shown to be beneficial in preventing restenosis of arterial stents, these effects cannot necessarily be extrapolated to venous stents. One might hypothesize extending antithrombotic treatment for an indefinite period, following venous stenting in PTS patients, especially if multiple DVTs have occurred or if thrombophilia testing is positive.
Conclusion
Stents placed for venous thrombosis are associated with higher disease burdens and intuitively have poorer outcomes compared with stents placed for venous compression. It is noteworthy that most stent occlusions occur in post-thrombotic limbs.
For that reason, a selective approach and planning should focus on identification of risk factors for stent failure. Stent failure continued even after 6 months, emphasizing the importance of an extended surveillance.















