Introduction
The kidney is a metabolically active organ with a terminal arterial supply, so quickly established parenchyma infarction is expected after acute renal artery occlusion (ARAO). These patients usually present with nonspecific symptoms making timely diagnosis difficult.1 Percutaneous revascularization is recommended if the occlusion is less than 6 hours.2 However, significant controversy remains regarding the benefits of late revascularization in ARAO. Reversal of renal dysfunction and hypertension has been reported after delayed revascularization, even in patients requiring dialysis. However, there are no recommendations on who, when, and how to revascularize in case of a late diagnosis. We present a patient with acute occlusion of both renal arteries requiring dialysis, revascularized after 21 days with renal function recovery. The patient provided written informed consent to publish clinical data and images.
Case report
A 64-year-old male with a clinical background of smoking and high blood pressure (HBP) leading to heart failure with reduced ejection fraction and intermittent claudication was admitted to the emergency department for an oliguric acute kidney injury (AKI) conditioning a decompensated heart failure. The patient previously had uncharacterized chronic kidney disease with a basal serum creatinine of 1.26mg/dL, estimating a glomerular filtration rate of 47ml/min. At the emergency department, serum creatinine and urea were 6.56mg/dL and 233mg/dL. The ion measurement revealed potassium of 5.1mEq/L and normal levels of remaining ions. The renal ultrasound showed kidneys with normal morphology and dimensions, preserved parenchymal echostructure, and no hydronephrosis or ureterovesical obstruction.
The patient was hospitalized and started intravenous diuretic and antihypertensive therapy. He responded well to furosemide, isosorbide dinitrate, and morphine, improving diuresis, dyspnea, and oxygen saturation. An extensive study was carried out to investigate the etiology of renal dysfunction without identifying the causal factor. Renal scintigraphy revealed viable kidneys with a markedly decreased global function, worse in the left kidney, apparently related to an acute and potentially reversible process. On the sixth day of hospitalization, the patient developed anuria unresponsive to furosemide, hypervolemia, resistant HBP, and worsening metabolic acidosis and hyperkalemia, which demanded the initiation of hemodialysis by a femoral central venous catheter (CVC).
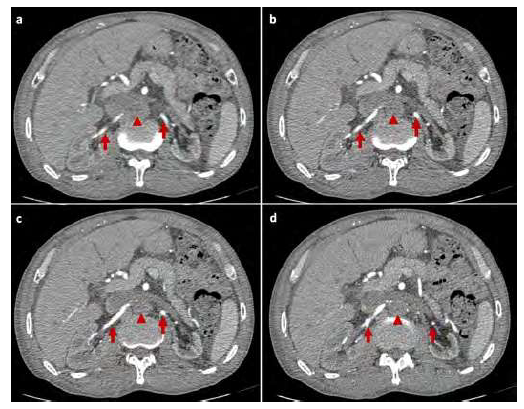
Two days later, an ultrasound study of the renal arteries revealed poor kidney perfusion with a “parvus et tardus” flow on both renal arteries; the renal veins were patent without flow disturbances. To adequately characterize arterial obstruction, he underwent a computed tomography angiography (CTA) that shows aortoiliac thrombosis starting below the superior mesenteric artery, conditioning the occlusion of the proximal segment of both renal arteries (Fig 1). Since admission, the patient did not refer to worsening of intermittent claudication but was confined to bed.
Abdominal computed tomography angiography showing pararenal aortic thrombosis and bilateral proximal renal artery occlusion (arrowhead). Reconstitution of the middle and distal segments of the renal arteries could be observed (arrows).
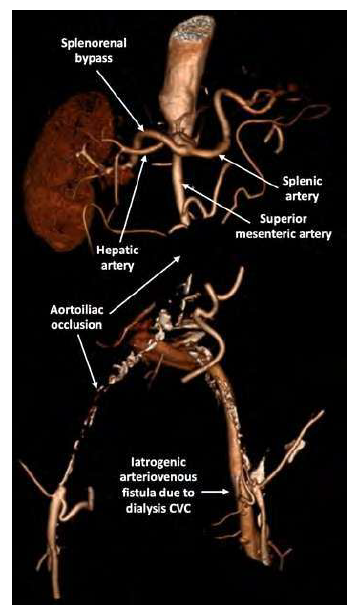
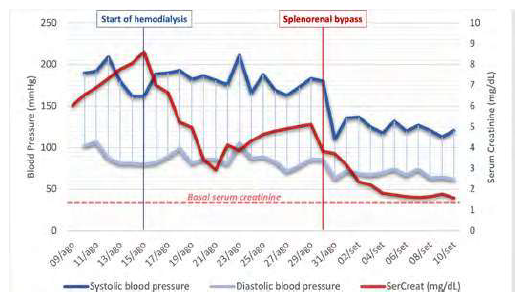
The case was discussed multidisciplinarily, and right renal artery open surgical revascularization was decided. Due to the patient's high surgical risk, we chose only to revascularize the right kidney, which was shown to be undoubtedly viable in renal scintigraphy. Likewise, it was decided to anchor the inflow in the splenic artery in favor of the aorta to avoid thrombus mobilization or supra celiac clamping, risking deleterious hemodynamic effects associated with ischemia/reperfusion of the mesenteric territories. A splenorenal retrocaval bypass was done uneventfully through a midline incision using a 6mm ringed ePTFE graft 21 days after the initial presentation (Fig 2). Immediately after surgery, the patient showed marked improvement of diuresis with decreased nitrogen retention parameters (Fig 3), allowing definitive suspension of the dialysis in the first three days and better blood pressure control. Serum creatinine dropped to baseline and remained stable at one year of follow-up. Chronic limb-threatening ischemia developed later with ulceration of the left foot due to aortoiliac thrombosis, aggravated by a left femoral arteriovenous fistula (AVF), a complication of the previous femoral CVC. The patient underwent an axillobifemoral bypass and AVF correction. The postoperative bilateral ankle-brachial index was > 0.9 with foot ulcer healing and resolution of claudication.
Discussion
In the setting of ARAO causing renal ischemia, salvage of a functioning kidney depends on timely revascularization requiring a high index of suspicion for a rapid diagnosis. Nonspecific symptoms and laboratory findings contribute to delayed diagnosis,1 so imaging confirmation is critical. Our case underlines the importance of these factors. The patient was admitted to the emergency department with an oliguric AKI, having carried out an extensive investigation; however, the etiology of AKI was only diagnosed by CTA on the 8th day of hospitalization. Although CTA requires nephrotoxic iodinate contrast, it is more sensitive than ultrasound.3
The evidence to support treatment strategies for patients with ARAO is poor, primarily due to the rarity of this situation, with only a few clinical cases and small series reported. Endovascular revascularization is usually used as first-line therapy.2 Techniques may include a combination of thrombolysis, thromboaspiration, mechanical catheter thrombectomy with angioplasty, and stenting if necessary. Surgical revascularization with open thrombectomy or bypass could be an option in patients with extensive thrombus burden, thrombolysis contraindication, and endovascular treatment failure.1,4 Although the ischemic window of kidney viability is narrow, some reports in the literature demonstrate benefits in late renal artery revascularization (>24h) in patients with acute presentations, so there is still doubt regarding managing these patients.2
The associated etiology (embolism, thrombosis, or dissection) influences the clinical picture and prognosis. In a small series of 16 patients surgical revascularized for ARAO, Ouriel et al. showed that only patients with thrombotic occlusion recover renal function after revascularization, not seen in patients with embolic or traumatic occlusion. Kidney function retrieval depended on a reconstituted distal renal artery, irrespective of the delay of revascularization.5 Usually, thrombotic occlusions are associated with atherosclerosis, so they are possibly well tolerated due to the development of significant collateralization. These data support that warm ischemia time is not the only factor weighing on kidney viability.5 Glomerular collapse and tubular necrosis occur when renal perfusion is abruptly reduced, but when enough flow remains, the tubular function is preserved despite the decrease of the glomerular filtration rate.6 Although not sufficient for normal organ function, the collateral branches can guarantee the viability of the kidney.5 In the reported case, atherosclerotic lesions in the ostium of both renal arteries existed, favoring the development of extensive collateralization. Scintigraphy and CTA showed viable kidneys without evidence of parenchymal necrosis. Likewise, the presence of venous flow even with evidence of renal artery occlusion indicated a good collateral network.7 This allowed the preservation of kidney viability despite the absence of normal perfusion after ARAO.
Our case corroborates some predictors of recovery of kidney function previously reported as thrombotic occlusion, distal renal artery reconstitution suggesting good collateralization, and persistent HBP suggesting remaining tubular function.8,9 Renal function rescue has been reported with renal artery occlusions for up to three months.2 However, these patients should be revascularized as soon as possible. Better outcomes have been observed in patients revascularized with catheter-directed thrombolysis for ARAO in the first 48 hours.1
We used a splenorenal bypass to revascularize the right kidney due to the estimated preoperative risk and aortic thrombus burden. Using splenic artery as inflow to the kidneys may be advantageous in non-candidates for an aortorenal bypass, such as cardiac dysfunction cases that preclude aortic clamping, previous aortic graft, and severe calcification.10 93% patency rates have been reported at approximately five years of follow-up.10
Our case highlights the benefit of late renal artery revascularization in cases of ARAO to avoid renal replacement therapy. Aggressive late renal revascularization may benefit selected patients independent of the time from the presentation. More extensive studies would be essential to provide adequate patient selection and management recommendations.