Introduction
Proximal juxtarenal involvement in aortic abdominal aneurysm (JAAA) may preclude the traditional endovascular aortic repair (EVAR). Recent endovascular techniques have been employed for those with neck lengths inferior to 10mm, such as fenestrated/branched EVAR (f/bEVAR) and parallel graft such as chimney EVAR (ChEVAR).1 These techniques aim to achieve a durable proximal aortic neck while maintaining patency of visceral branches.
Parallel stentgraft techniques such as ChEVAR were initially used for "bail-out" in patients with inadequate landing zones and accidental visceral coverage.l2l Their current application for complex AAAs has been relegated for when there is unavailability off/bEVAR endografts, especially due to durability concerns.2 However, the off-the-shelf nature of the ChEVAR technique makes it a good alternative for urgent/emergent AAA repair. We report our institutional experience in ChEVAR in urgent setting.
Methods
Cohort selection
This is a single-centre retrospective study of consecutive ChEVAR procedures collected from January 2019 to March 2023 in a tertiary hospital. Inclusion criteria were procedures for aneurysm repair (JAAA or TAAA) performed in urgent/ emergent setting in which chimney technique was employed. ChEVAR performed in elective setting were excluded.
Definitions
The Crawford classification was used for the extent of thoracoabdominal aneurysms. Sac regression was the reduction in maximum diameter of the aneurysm sac by::: 5 mm.
Outcomes
Primary outcomes were technical success, 30-day mortality and 1-year mortality rates. Secondary outcomes were target vessel patency. Surveillance strategy consisted of Computed Tomography Angiography (CTA) performed during admission, 30 days, six months and yearly. Imaging collection and analysis was performed using the centre's workstation Sectra 1DS7 (Sectra AB, Linkoping, Sweden).
Results
Demographics
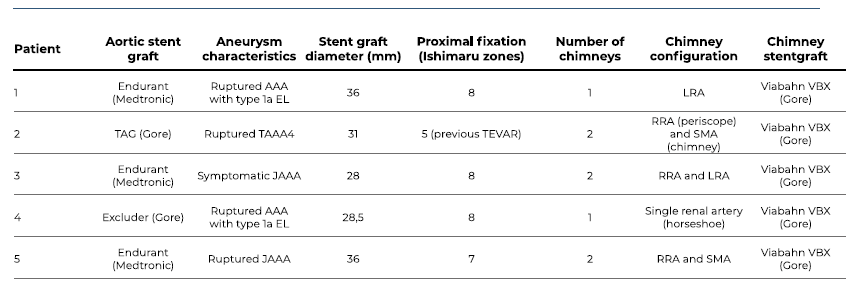
We report a series of 5 patients (Figure) submitted to emergent/urgent aneurysm repair using ChEVAR technique. Average age was 73,4 years (45-89) and all patients were male. Arterial hypertension was present in 100% patients; 80% were former smokers and all patients were ASA 4 (American Society of Anesthesiologists). Indications for surgery were: post EVAR type la endoleak with associated rupture or symptomatic in two patients; symptomatic/contained rupture of JAAA in two patients; and contained rupture of a thoracoabdominal aneurysm (TAAA) in one patient. The latter, a 45-year-old male with a type 4 TAAA, was submitted to ChEVAR technique based on previous laparotomies and associated intraabdominal infection.
Table 1 Pre-operative characteristics of patients treated with ChEVAR for emergent aneurysms.
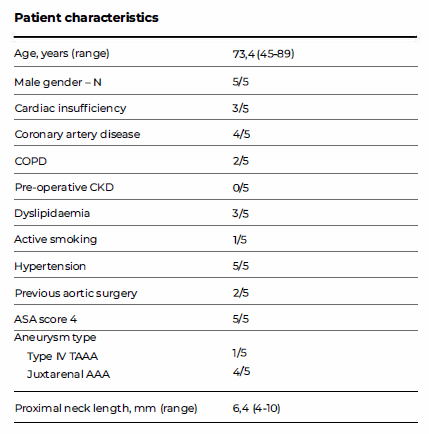
AAA abdominal aortic a neurysm;ASA American 5ociety of Anesthesiologists; CKD chronic kidney disease; COPD chronic obstructive pulmonary disease; TAAA thoracoabdominal aortic aneurysm.
Technical details
Femoral and brachial/axillar cutdowns were used in all patients. A total of 8 target vessels were catheterized: two patients required single-vessel chimney and the remainder two-vessel chimney. Target vessels were two superior mesenteric artery and six renal arteries. Technical success rate was 100%. There were no major complications and average admission period was 15 days (range 6-24).
Short and mid-term outcomes
The 30-day mortality was 0% without any major complications. Follow-up CTA at 30 days excluded any procedure-related complications or endoleaks, including gutter-related endoleaks. Sac regression was observed in all patients.
Follow-up time was 20.2 months (range 4.7-38) and 3/5 of patients have expired due to non-aortic related pathologies, on average 18 months after surgery (range 4.7-38), with a 1-yearsurvival of 80%. Target vessel patency during the followup period is 87.5% (l renal artery occluded at 23 months). The three deaths were attributed to complications related to medical comorbidities: pneumonia, COPD exacerbation and acute heart failure.
DISCUSSION
Our "real-world" institutional experience with ChEVAR revealed favorable short-term mortality and mid-term target vessel patency during the 20-month follow-up period. The significant medium and long-term mortality, despite non-aortic related, is explained by the baseline characteristics of these patients, with severe comorbidities and high ASA score.
Since the first use of ChEVAR, case reports and short series have been published. However, in 2015, the multicentric PERICLES registry revealed results comparable to other endovascular options. This supported the use of ChEVAR as an off-the-shelf alternative.3 The favorable short and medium-term outcomes of the PERICLES registry were further analyzed in a long-term analysis which revealed a 5-year 66% survival and 92% chimney graft branch vessel patency.4
A 2022 systematic review included 1019 patients assessed mid-term outcomes of ChEVAR for JAAA.5 The study found survival and target vessel patency at 3 years of 81.4% and 95.1%, respectively. It should be noted that a large proportion of these studies were performed in high-volume referral centers and may not reflect real-world results.
Recently evidence, has emerged to better clarify how this technique compares to open repair and f/bEVAR in JAAA. Zlatanovic et al6 found that ChEVAR and f/bEVAR had higher rates of aortic-related reintervention and side branch occlusion/stenosis when compared to open repair. The direct comparison between f/bEVAR and ChEVAR did not found significant differences in outcomes. It is noteworthy that this network meta-analysis was based in poor-quality and heterogenous studies (observational and registries). Open repair was not considered in our cohort due to severe prohibitive medical comorbidities in four patients and previous abdominal surgery and infection in one patient.
The applicability for ChEVAR may pose a problem when planning the procedure in some patients7, for which f/ bEVAR may be better suited. In the emergent setting, offthe-shelf f/bEVAR can be a solution for a significant portion of these patients. The required upper limb access for ChEVAR is an additional disadvantage opposed to f/bEVAR which can currently be performed with femoral access only. Type l endoleak related to gutters remain a major concern for ChEVAR - despite an acceptable low rate.8 However, complete and adequate sealing is mandatory in ruptured JAAA.
In our cohort off-the-shelf f/bEVAR was not considered due to the unavailability of these devices in our center. Physician modified endografts (PMEG) techniques were excluded due to inexperience with such procedures. It should also be considered that f/bEVAR and PMEG require higher levels of expertise than ChEVAR. Compared to PMEG and ChEVAR, the off-the-shelf f/bEVAR leads to more extensive aortic coverage and sacrifice of segmental arteries, especially for JAAA.l8l
As opposed to custom-made f/bEVAR, ChEVAR offers immediately available with standard off-the-shelf devices, lower cost and access profile. Furthermore, ChEVAR may surpass certain anatomical contraindications for f/ bEVAR, especially in the emergent setting. These complex endovascular procedures require continued surveillance to detect failure requiring interventions.
The main limitations of this study concern its small sampie, single-centre and retrospective nature. Although major technical details overlap, the procedures were not standardised, and variations occurred.
Conclusion
Our experience shows high technical success and low short-term morbidity and mortality with the use ofChEVAR for acute aortic aneuryms. High mid-term mortality was observed due to non-aortic causes. Sac regression, low rates of target vessel occlusion and type la endoleaks reveal a favourable profile for AAA exclusion. The ChEVAR technique is a viable option in the emergent setting for patients unfit for open repair.