Introduction
Peripheral Arterial Disease (PAD) affects more than 200 million individuals worldwide, representing an increase in its prevalence of 29% in low-income countries and 13% in high-income countries (throughout the decade of 2000-2010).1
This pathology is a common manifestation of systemic atherosclerosis and indicates coronary and cerebrovascular atherosclerosis. PAD is also associated with a five times higher risk of acute myocardial infarction (AMI) or stroke and a three times higher risk of death.2,3 At six months, of the patients with CLTI who were not revascularized, 40% will have suffered an amputation, and 20% will have died.4
PAD risk factors remain similar between males and females, including smoking behaviour, age, diabetes mellitus (DM), hypertension, and dyslipidaemia.5
According to the literature, PAD prevalence in women has varied between 3% and 29%.6 Generally, asymptomatic PAD is more common in females than in males (13% versus 9%).7 However, when symptomatic, the female gender presents a more complex disease (in several arterial sectors), with a more severe clinical presentation (CLTI), and worse outcomes.7-10 Compared to men, women with PAD usually present symptoms only 10 to 20 years later.8
Few studies on PAD characteristics in the Portuguese female population were published. Only three studies, published in 2020, 2021, and 2023, approached PAD gender differences, two referring to Lisbon's population and the most recent to Coimbra’s. The first one is an international research study, and it concluded that Portugal is the country holding the highest disparity between genders, where only 23% of patients submitted to revascularization by PAD were women.11
Given PAD’s high burden of disease and the low representation of women in PAD studies and clinical trials,12 this paper aims to characterize women with PAD hospitalized in a Vascular Surgery Department. The specific aims are to compare gender differences in: clinical presentation at admission, age, comorbidities, usual medical treatment, hospitalization characteristics, revascularized sectors, therapeutic strategy during hospitalization and CLTI clinical outcomes.
Methods
An observational, analytical, retrospective, longitudinal study was conducted. Patients hospitalized in the Vascular Surgery Department from January 2018 to December 2019, with symptomatic PAD (intermittent claudication or CLTI), suggested by the clinical history and objective examination and confirmed with ABI, were consecutively included in the study. On the other hand, patients admitted for complementary diagnostic exams or patients with non-atherosclerotic PAD were excluded from the study. The clinical information was obtained by consulting the medical records. The following data was collected:
- Sociodemographic data: age, sex;
- Clinical presentation at admission: intermittent claudication or CLTI;
- Comorbidities: chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), stroke, transient ischemic attack (TIA); DM, arterial hypertension, heart failure, coronary heart disease (CHD), smoking habits, dyslipidaemia, and depression;
- Chronic medication: antihypertensive drugs, statins, fibrates, ezetimibe, oral antidiabetic drugs (OAD), insulin, antiplatelet therapy, anticoagulant, phosphodiesterase 3 inhibitor (PD3-i);
- Hospitalization data: length of stay; provenance (emergency room or outpatient clinic); decreased functional status on admission (dependent); hospital discharge (home versus long-term care national network);
- Revascularized sectors (aortoiliac; femoropopliteal; distal);
- Treatment during hospitalization: medical treatment (only); revascularization: endovascular or surgical; amputation surgery (includes both primary and secondary): major or minor;
- Clinical outcomes evaluated: 30-day mortality, successful revascularization, and amputation-free survival.
Revascularization success was defined as the absence of major amputation, 30 days after revascularization (regardless of the need for reintervention during this period or not).
The outcome amputation-free survival evaluates the elapsed time between a revascularization surgery and death or major amputation.
Hospitalization data, treatment during hospitalization, and clinical outcomes evaluated are exclusively CLTI sub-analysis.
The statistical analysis was conducted through the 27th version of the Statistical Package for the Social Science (SPSS®) program. In the qualitative variables, both absolute (n) and relative (%) frequency were characterised. Regarding the categorical variables’ comparison, a chi-square test (χ2) or Fisher exact test (in the cases where over 20% of cells had an expected count inferior to 5) were applied. Concerning the quantitative variables, the asymmetry and kurtosis values were used to assess the sample’s distribution. Additionally, a visual analysis of the histogram and the Kolmogorov-Smirnov test were performed. When a normal distribution was verified, a presentation of the mean and standard deviation, along with a comparison of the mean among groups, was conducted, through the t-test for independent samples. For the variables where the normality was not verified, a presentation of the median and interquartile range, along with a comparison among groups was undertaken through the Mann-Whitney U test.
An evaluation was made considering the gender relation with the probability of major amputation through binary logistic regression, initially univariate, and subsequently, a multivariate analysis was executed. Variables holding p<0.25 in the univariate analysis were included in the initial multivariate model. In the amputation-free survival outcome, a Kaplan-Meier survival analysis was developed and a Log-Rank test was also conducted in order to evaluate the differences among genders. For all tests, p<0.05 was considered a statistically significant value, with a confidence interval (CI) of 95%.
The present research was approved by the Ethics Committee for Health of the respective institution.
Results
The selection process of the sample is presented as a flowchart in Figure 1.
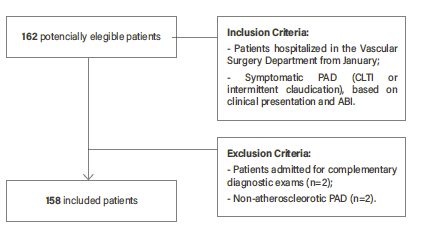
Figure 1 Patient selection flowchart. PAD: peripheral arterial disease; CLTI: Chronic limb threatening disease; ABI: Ankle-brachial index
Characterization of the Sample
One-hundred and fifty-eight hospitalized patients with a PAD diagnosis were included, 107 of male gender (67.7%). Females were older than men (76.5 ± 10.4 years old vs. 69.5 ± 10.6 years old, p<0.001, Table 1. In younger age groups, PAD is more prevalent among men. On the contrary, in the age group ≥ 80 years, the prevalence was higher among women (Figure 2).

Figure 2 Comparison of PAD prevalence, according to the age group, between male and female patients (n = 158).
Considering the risk factors and comorbidities, women presented a lower proportion of smoking habits compared to men (smokers/ex-smokers), 4.0% versus 58.9%, p<0.001. However, women presented a higher prevalence of hypertension (90.2% versus 73.8%, p=0.021), DM (74.5% versus 57.0%, p=0.036) and depression (7.0% versus 0.9%, p=0.002), Table 1.
Table 1 Comparison of male vs. female PAD patients concerning the demographic features and comorbidities, through the absolute and relative frequency and Chi-square test
| Female (n=51) | Male (n=107) | χ2 | df | p | Phi | |
|---|---|---|---|---|---|---|
| Age - mean (SD) | 76,5 (10,4) | 69,5 (10,6) | 2,64 | - | <0,001 | -0,663 |
| Smoker - n (%) | 1 (2,0) | 35 (32,7) | 43,1 | 2 | <0,001 | 0,522 |
| Ex-smoker - n (%) | 1 (2,0) | 28 (26,2) | ||||
| Non-smoker - n (%) | 49 (96,1) | 44 (41,1) | ||||
| Hypertension - n (%) | 46 (90,2) | 79 (73,8) | 5,597 | 1 | 0,021 | 0,188 |
| Dyslipidemia - n (%) | 30 (58,8) | 54 (50,5) | 0,969 | 1 | 0,394 | 0,078 |
| Diabetes - n (%) | 38 (74,5) | 61 (57,0) | 4,521 | 1 | 0,036 | 0,169 |
| Stroke - n (%) | 14 (27,5) | 17 (15,9) | 2,928 | 1 | 0,132 | 0,136 |
| TIA - n (%) | 0 (0) | 2 (1,9) | - | - | >0,99 | -0,078 |
| CAD - n (%) | 6 (11,8) | 22 (20,6) | 1,833 | 1 | 0,191 | -0,108 |
| Heart failure - n (%) | 13 (25,5) | 17 (15,9) | 2,070 | 1 | 0,193 | 0,114 |
| COPD - n (%) | 3 (5,9) | 15 (14,0) | 2,265 | 1 | 0,182 | -0,120 |
| CKD - n (%) | 9 (17,6) | 19 (17,8) | 0,000 | 1 | >0,99 | -0,001 |
| Depression - n (%) | 7 (13,7) | 1 (0,9) | - | - | 0,002 | 0,273 |
TIA: transient ischemic attack; CAD: coronary artery disease; COPD: chronic obstructive pulmonary disease; CKD: chronic kidney disease.
A higher number of women were on insulin (42.0% versus 24.3%, p=0.027) and antihypertensive therapy (88.0% versus 71.0%, p=0.026), Table 2. No relevant differences were found between men and women in the remaining medical history and usual medication.
Regarding the clinical presentation at admission, 50 females (98.0%) were admitted for CLTI and only one (2.0%) for intermittent claudication, while 94 males (87.9%) were hospitalized for CLTI and 13 (12.1%) for intermittent claudication.
Females were more frequently admitted by CLTI and, particularly, for stage IV in Fontaine’s classification, Table 3.
The hospitalization median length of stay was 7 days in the female group and 9 days in the male. No relevant differences were registered in this parameter (p=0.490).
Considering the revascularized sectors, women were significantly less frequently revascularized in the aortoiliac sector (18.0% versus 50.0%, p=0.012). In the remaining sectors, there were no significant variations between groups (Table 4).
Table 2 Comparison of male vs. female PAD patients concerning medication at admission
| Female (n=50) | Male (n=107) | χ2 | df | p | Phi | |
|---|---|---|---|---|---|---|
| Antihypertensives - n (%) | 44 (88,0) | 76 (71) | 5,449 | 1 | 0,026 | 0,186 |
| ACEIs/ARBs - n (%) | 34 (68,0) | 64 (59,8) | 0,974 | 1 | 0,378 | 0,079 |
| Antiplatelets - n (%) | 32 (64,0) | 77 (72,0) | 1,018 | 1 | 0,354 | -0,081 |
| Anticoagulants - n (%) | 14 (28,0) | 18 (16,8) | 2,624 | 1 | 0,136 | 0,129 |
| Statins - n (%) | 35 (70,0) | 77 (72,0) | 0,064 | 1 | 0,851 | -0,020 |
| Fibrates - n (%) | 3 (6,0) | 7 (6,5) | - | - | >0,99 | -0,010 |
| Ezetimibe - n (%) | 0 (0) | 2 (1,9) | - | - | >0,99 | -0,078 |
| OAD - n (%) | 24 (48,0) | 53 (49,5) | 0,032 | 1 | 0,858 | -0,014 |
| Insulin - n (%) | 21 (42,0) | 26 (24,3) | 5,090 | 1 | 0,027 | 0,180 |
| PDE3-i - n (%) | 3 (6,0) | 7 (6,5) | - | - | >0,99 | -0,010 |
ACEI: Angiotensin-converting enzyme inhibitors; ARB: Angiotensin II receptor blockers; OAD: oral antidiabetic drugs; PDE3-i: phosphodiesterase 3 inhibitor
Table 3 Comparison of male vs. female PAD patients concerning the clinical presentation at admission
| Female (n=51) | Male (n=107) | χ2 | df | p | Phi | |
|---|---|---|---|---|---|---|
| IC - n (%) | 1 (2,0) | 13 (12,1) | - | - | 0,038 | -0,168 |
| CLTI - n (%) | 50 (98,0) | 94 (87,9) | - | - | 0,038 | 0,168 |
| LF Grade IV - n (%) | 46 (90,2) | 79 (73,8) | 5,597 | 1 | 0,021 | 0,188 |
IC: Intermittent claudication; CLTI: Chronic limb threatening ischaemia; LF: Leriche-Fontaine
Table 4 Comparison of male vs. female PAD patients concerning the revascularized sectors.
| Revascularized sector | Female (n=22) | Male (n=68) | χ2 | df | p | Phi |
|---|---|---|---|---|---|---|
| Aortoiliac - n (%) | 4 (18,0) | 34 (50,0) | 6,898 | 1 | 0,012 | -0,277 |
| Femoropopliteal - n (%) | 16 (72,7) | 43 (63,2) | 0,663 | 1 | 0,453 | 0,086 |
| Distal - n (%) | 8 (36,4) | 22 (32,4) | 0,120 | 1 | 0,797 | 0,037 |
Therapeutic strategies for CLTI patients
Significant variations were observed in revascularization by conventional surgery (18.0% of women versus 41.5% of men, p=0.005) and in the major amputation rate (40.0% of women versus 21.3% of men, p=0.020), in particular above the knee amputation (p<0.024). Hybrid (conventional and endovascular) procedures were performed in 7.5% of men, while none were performed in females (Table 5).
Through univariable binary logistic regression, it was noted that women diagnosed with CLTI have a 2.47 times greater risk of major amputation when compared to men with CLTI (p=0.018). However, when adjusted through multivariable analysis, for the predictor variables with p<0.25 in univariable analysis, the gender effect was no longer relevant (OR=1.41; p=0.428), where the age was the main independent predictor in the major amputation (OR=1.08; p=0.001, Table 6).
Table 5 Comparison of revascularization strategies for male vs. female CLTI patients
| Female (n=50) | Male (n=94) | χ2 | df | p | Phi | |
|---|---|---|---|---|---|---|
| Revascularization - n (%) | 21 (42,0) | 55 (58,5) | 3,570 | 1 | 0,079 | -0,157 |
| Open - n (%) | 9 (18,0) | 39 (41,5) | 8,104 | 1 | 0,005 | -0,237 |
| Endovascular - n (%) | 12 (24,0) | 23 (24,5) | 0,004 | 1 | >0,99 | -0,005 |
| Major Amputation - n (%) | 20 (40,0) | 20 (21,3) | 5,703 | 1 | 0,020 | 0,199 |
| Above-knee - n (%) | 18 (36,0) | 17 (18,1) | 5,694 | 1 | 0,024 | 0,199 |
| Below-knee - n (%) | 2 (4,0) | 4 (4,3) | - | - | >0,99 | -0,006 |
| Minor Amputation - n (%) | 11 (22,0) | 32 (34,0) | 2,260 | 1 | 0,180 | -0,125 |
| Medical Treatment only - n (%) | 4 (8,0) | 6 (6,4) | - | - | 0,739 | 0,030 |
Table 6 Odds of major amputation of patients with CLTI
| Univariable | Multivariable | |||||
|---|---|---|---|---|---|---|
| p | OR | CI-95% | p | OR | CI-95% | |
| Female sex | 0,018 | 2,467 | 1,164-5,228 | 0,428 | 1,410 | 0,603-3,294 |
| Age | <0,001 | 1,084 | 1,041-1,130 | 0,001 | 1,080 | 1,034-1,129 |
| Stroke | 0,071 | 2,193 | 0,935-5,146 | 0,359 | 1,550 | 0,608-3,949 |
| Depression | 0,164 | 2,778 | 0,660-11,693 | 0,274 | 2,434 | 0,494-11,991 |
OR: Odds Ratio; CI: Confidence Interval
The type of admission was similar between groups: 44.0% of women and 48.9% of men were admitted through the emergency room, p=0.603. Of the 18 patients who were dependent on admission, 17 were amputated. For this reason, a decreased functional status is strongly associated with the risk of major amputation (p<0.001; Phi=0.56). Female patients had a significantly decreased functional status on admission (28.0% of women were bedbound versus only 4.3% of men, p<0.001; Phi=0.34). Concerning the type of hospital discharge, 86.0% of women were discharged home versus 88.3% of men (p=0.792).
Regarding CLTI patients submitted to revascularization (21 female and 55 male), the successful revascularization rate was similar between genders, with a 90.5% success rate for women and 90.7% for men (p>0.99).
Mortality rate at 30-days was 12.0% for women (6 deaths) and 5.3% for men (5 deaths). Although a tendency is suggested, no relevant statistical variations were registered between groups (p=0.191). Given that only 11 deaths occurred and considering a cut-off of 10 events by predictor to carry out multivariable analysis, the adjusted evaluation of this outcome was not conducted.
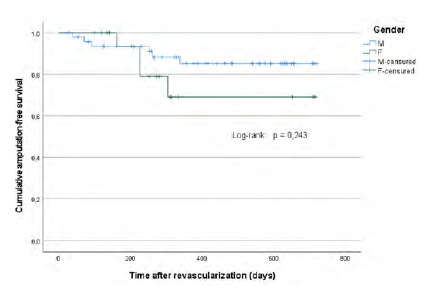
Amputation-free survival
Until December 2019, 10 events (deaths/major amputations) were registered (14.7% of the total number of cases, n=68), four in female patients and six in male patients. The percentage of censored patients was similar in women (78.9%) and men (87.8%), Figure 3.
The amputation-free survival mean was inferior in the female, comparatively to the male group, respectively 568±62 days and 642±30 days. However, in the Kaplan-Meier survival analysis, the Log-Rank Test indicated the absence of relevant differences between groups, p=0.243.
Discussion
Women admitted with PAD, compared to men, had higher rates of major amputation and were less likely to be revascularized by conventional surgery. Females were older, had a higher prevalence of DM, had more severe disease, and were more dependent upon admission. Nevertheless, the prognostic was similar between sexes (no significant differences concerning successful revascularization, 30-day mortality, and amputation-free survival).
Historically, PAD was more prevalent in males.13 However, recently, different studies recognised a similar or even higher prevalence in women.14 Most of these studies were demographic and based on ABI measurements, showing a superior prevalence of asymptomatic PAD (ABI<0.9) in females.7,15 A study of hospitalized patients confirmed that men were more frequently symptomatic and were more likely to have surgical indication. The higher number of men in our sample is consistent with the literature.11,16,17
In this research, females were more frequently admitted with CLTI. Several explanations can be advanced: 1) atypical symptoms in women, which can be mistaken for joint pain or intolerance to physical efforts,18 leading to a late diagnosis and more advanced stages of disease, 2) lower prevalence of intermittent claudication in women, due to inferior muscular mass and due to lower levels of activity in older ages.18,19
The female and male groups presented an average age of 76.5 and 69.5 years old, respectively, with women being about 7 years older, which is supported by the existing literature.15,20 Contrarily to younger age groups, in the age group ≥ 80 years old, PAD prevalence was superior in the female gender. These data can be explained by: 1) higher life expectancy in women; 2) loss of estrogen’s vascular protective effect in post-menopausal women.8,15
We also noted a higher level of smoking habits and a lower prevalence of DM in male patients. Females presented a higher prevalence of hypertension and depression, which is supported by the current evidence.14,21 Relatively to other comorbidities, no variations were noted. Other studies also did not register differences.22 Nevertheless, Lo et al. demonstrated that men have greater prevalence of CHD, DM, COPD and CKD, while women have a higher prevalence of cardiac insufficiency, hypertension and stroke.20
In terms of usual medication at admission, except for insulin and antihypertensive drugs, no differences were found between genders. A demographic study reports lower levels of statins, antiplatelet, and ACEIs in women with PAD.23 Since our study is focused on a hospitalized sample, a stronger medical follow-up along with a higher control of risk factors is more probable.
Smoking habits are described as a risk factor for PAD and particularly for aortoiliac atherosclerosis.13,24 In this study, we found that men were more likely to be intervened on the aortoiliac sector and that men displayed, as well, a higher prevalence of smoking habits. Conversely, advanced age and DM are related to femoropopliteal and distal PAD.13 In this research, female individuals registered a higher prevalence of this risk factors and a tendency for higher number of interventions in these sectors, yet this difference was not statistically significant.
No differences were noted concerning the hospitalization duration, admission provenance or post hospital discharge destination. However, studies indicate that women present longer periods of hospitalization, higher probability of emergency admission and discharge for the Long-term Care National Network.12,16
As just one woman had intermittent claudication, the statistical evaluation between genders, regarding therapeutical options and clinical outcomes was not possible. For this purpose, a larger sample group is required.
Considering hospitalized patients with CLTI, we verified that males had a significantly higher rate of revascularization by conventional surgery. This is supported by the literature: men with PAD have a better surgical risk than women and greater vessel diameter, which facilitates the intervention.12 Women were preferably revascularized by endovascular procedures given the advanced age and comorbidities.20,22,25,26 In this study, a higher number of revascularized female patients by endovascular procedure was found, in comparison to conventional surgery.
On the other hand, women were more frequently subjected to major amputation, in particular above the knee. Decreased functional status along with advanced age, were found as predictors of amputation. Various studies confirm a higher major amputation rate in female patients,27,28however other studies did not find divergences or reached a higher major amputation rate in males.25,29
Regarding the successful revascularization rate, no differences were noted between males and females, aligned with several other studies.22,30-32
On the topic of mortality, the literature presents conflicting results. Some studies demonstrate higher mortality among the female group for all procedures,16,28,33,34 while others did not report relevant variations.32,35
It is possible that sex could be a mortality risk factor per se. The association between mortality and sex can also be explained by advanced age, the higher number of comorbidities, and by the disease severity in women. It is therefore important to adjust for statistical confounding factors and consider the type of procedure. In this study, given the limited number of events (11 deaths in 158 patients), it was not possible to accurately evaluate the statistical impact of sex on mortality.
No significant differences were noted in the amputation-free survival (post-revascularization) analysis. However, women had a shorter amputation-free survival. The published papers have divergent results.12,36,37
Considering studies that focus on the Portuguese population: a) Correia et al, showed that outcomes in revascularized patients were similar between genders; women were older and more frequently submitted to endovascular revascularization;22 b) Baldaia et al found that women had higher major amputation rates, were treated at a more advanced stage of the disease, and showed greater mortality rates at 90-day follow up;38 c) In the VASCUNET study, which compared 11 countries, Portugal was the country with the highest gender disparity in most parameters: of the revascularized patients only 23% were female; hospitalization for intermittent claudication was 14.9% higher in men; the octogenarian’s group had a 21% higher number of females, and a 14.9% higher number of women submitted to endovascular revascularization.11 The results obtained by these studies are mostly aligned with ours.
This study has some limitations. It is a retrospective analysis conducted in one institution. The sample size is small, which limits the precise evaluation of specific outcomes. For future research, we consider increasing the sample size, analyse in detail the clinical outcomes, particularly the impact of gender on mortality, when adjusted to other predictors. Most studies focused their analysis on CLTI, limiting the available information on intermittent claudication patients. Hence, it is important to include them in future research.
Conclusion
There are notable differences in the prevalence of risk factors for PAD in women vs. men. Women have a higher prevalence of DM and advanced age, while males have superior smoking habits, which could explain the higher involvement and revascularization of the aortoiliac sector.
Male patients were more frequently submitted to revascularization and females to major amputation. Successful revascularization, 30-day mortality, and amputation-free survival were not different for males vs. females. Females were more dependent, had more advanced age, and had higher disease severity. This can explain a higher rate of major amputation in women.