Introduction
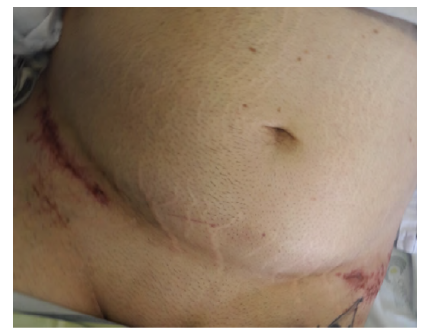
Seat Belt Aorta is a rare but potentially life-threatening injury that can occur in high-speed motor vehicle collisions. It refers to blunt trauma of the abdominal aorta, as a result of sudden deceleration caused by the seat belt during a collision, which compresses this large vessel against vertebrae. One of the key features of significant seat belt injuries is the presence of “Seat Belt Signs”, which are visible signs of the injury. These marks appear as abrasions or bruises across the chest and abdomen and are caused by the force of the seat belt restraining the body during the collision, being indicative of internal lesions in up to 30% of cases (Figure 1).1
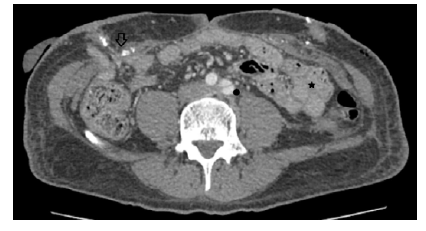
Seat Belt Aorta is often associated with two other injuries collectively referred to as the "Seat Belt Triad", which are abdominal wall disruption and hollow viscus injury (Figure 2). A fourth component, more common in children, is sometimes present, which is a horizontal fracture of the vertebral body, due to flexion-distraction forces acting on the spine, called Chance fracture.2
We aimed to review the published literature regarding aortic seat belt injuries.
Methods
Using Pubmed database we performed a non-systematic literature review on this subject including all the published cases reporting seat belt trauma to the abdominal aorta. We used different combinations of the search terms “seat belt aorta”, “seat belt triad” and (“seat belt” AND “aorta”). All articles reporting blunt injury to the abdominal aorta due to seat belt trauma were included. We further analysed presentation at admission, concomitant lesions, including presence of seat belt triad and “Chance fracture”, treatment and outcomes. Exclusion criteria were: articles not available in English or Portuguese; duplicated articles; reports on seat belt trauma to the thoracic aorta, the aortic arch or supra-aortic trunks; reports on paediatric population; blunt trauma to the aorta not resulting from seat belt use.
Results
A total of 30 articles, published between 1968 and 2019 were included, of which only 12 (40%) were published after 2000. Fifty-two cases of seat belt injury to the abdominal aorta were reported, all of which were either case reports or case series.1-30 Twenty-nine males (56%) and 23 females (44%), with a mean age at presentation of 43 (SD ± 19) years, ranged 18 to 82.
Presentation at Admission and Clinical Features
All patients except one (n=51) presented at the emergency department in the acute phase, with the following symptoms: 29 (55.8%) with abdominal pain, 26 (50%) with acute lower limb ischemia and 9 (17.3%) with hypotension/hypovolemic shock. Two patients developed late-onset lower limb claudication (5 to 48 months after the accident).
The presence of concomitant abdominal wall and hollow viscus injury (seat belt triad) was reported in 38 patients (73.1%) and the presence of seat belt sign was identified in 40 patients (76.2%) at admission. Among these, only 7 patients with seat belt sign did not have seat belt triad (p<0.01). Lumbar and Chance fractures were reported in 22 patients (42.3%), only 2 of which were not associated with the presence of seat belt triad (p<0.001).
Twenty-four studies reported on 35 patients,1-12 14 hemodynamic and conscience status at admission18-22,25-30 with 26 of these (74.3%) being hemodynamically stable when first entering the emergency department, while the remaining 9 (25.7%) were unstable. All patients were conscient at admission, except for one of the unstable patients, that was intubated and ventilated prior to arrival at the hospital.3
The most frequent vascular lesion reported was intimal dissection of the infrarrenal aorta and iliac arteries, present in 47 patients (90.4%), of which only 14 (29.8%) were uncomplicated dissections and the remaining 33 (70.2%) were complicated with either aorto-iliac thrombosis, false aneurysm formation, contained aortic rupture (peri-aortic hematoma), uncontained rupture or lower limb atheroembolism (Table 1).
Table 1 Reported vascular lesions caused by seat belt aortic injury, in 52 cases included in this review
| Reported Vascular Lesions | Patients N=52 |
| Aortic Dissection (All) - N (%) | 47 (90.4) |
| Complicated Aortic Dissection - N (%) Aortic Occlusion/Thrombosis False Aneurysm Contained Aortic Rupture (Periaortic hematoma) Lower Limb Atheroembolism Uncontained Aortic Rupture | 33 (63.5) 17 (32.7) 6 (11.5) 4 (7.7) 4 (7.7) 2 (3.8) |
| Uncomplicated Aortic Dissection - N (%) | 14 (26.9) |
| Isolated Lower Limb Atheroembolism - N (%) | 3 (5.8) |
| Acute Iliac Thrombosis - N (%) | 2 (3.8) |
| Other Reported Vascular Lesions - N (%) Inferior Vena Cava Laceration Superior Mesenteric Vein Tear Iliac Vein Thrombosis Inferior Mesenteric Artery Avulsion | 6 (11.5) 2 (3.8) 2 (3.8) 1 (1.9) 1 (1.9) |
Treatment and Outcomes
All patients presenting at the emergency department in the acute setting required immediate surgical intervention of some sort, with 40 (76.9%) requiring urgent vascular surgery and the remainder requiring either gastrointestinal, orthopaedic, abdominal wall repair or a combination of these. Eleven (21.2%) vascular lesions were initially managed conservatively,2,4,5,8,9,13,21,23,26 yet 3 required urgent surgery (1 to 3 days after admission), due to a rapidly expanding false aneurysm (n=2)8,21 or acute iliac thrombosis with limb ischemia (n=1)5 and 5 required later vascular repair (4 months to 2 years after admission) due to late-onset claudication (n=2),13,23 false aneurysm expansion (n=2)4,9 or acute iliac thrombosis with limb ischemia (n=1).26 One patient (1.9%) was too unstable and was considered for palliation only.17
A total of 48 patients (92.3%) underwent vascular procedures, of which 39 (81.3%) open surgery and 9 (18.8%) endovascular repair (Table 2). The most common procedure was aortic graft interposition (n=12; 25%), followed by aortoiliac thromboendarterectomy (n=10; 20.8%), endovascular aortic repair (EVAR) (n=7; 14.6%) and aorto-femoral or aorto-iliac bypass (n=6; 12.5%). Forty-one patients (85.4%) required aortoiliac repair (32 open and 9 endovascular) and the remaining 7 (14.6%) underwent either extra-anatomical revascularization or lower limb procedures.
Table 2 Reported vascular operations performed in patients with seat belt aortic injury, of 48 cases included in this review
| Procedure | Patients N=48 |
| Aortic Graft Interposition - N (%) | 12 (25) |
| Aortoiliac Thromboendarterectomy - N (%) | 10 (20.8) |
| Endovascular Aortic Repair (EVAR) - N (%) | 7 (14.6) |
| Aorto-femoral and Aorto-iliac Bypass - N (%) | 6 (12.5) |
| Lower Limb Thromboembolectomy - N (%) | 4 (8.3)* |
| Axillofemoral Bypass - N (%) | 3 (6.25) |
| Palmaz Aortic Stenting - N (%) | 2 (4.2) |
| Direct Aortic Suture - N (%) | 1 (2.8) |
| Not Indicated - N (%) | 3 (6.25) |
* Five additional lower limb thromboembolectomy were performed during other procedures.
Most patients with seat belt triad required multiple interventions for gastrointestinal and abdominal wall reconstruction, yet only 1 patient required vascular reintervention, due to a late-onset claudication 3 years after the initial surgery due to stent stenosis, which was treated by stent removal and interposition graft repair.13 Three patients required lower limb amputation, two of which were bilateral amputations.5
Ten patients (19.2%) passed, on average 7.6 days after initial surgery (1 to 31 days), with a mean age of 61 years (36 to 78) and the majority (70%) being female (7:3). Out of these patients, 7 presented with seat belt triad at admission. Associated vascular lesions were: dissection complicated with acute aortic thrombosis (n=6); dissection complicated with uncontained aortic rupture (n=1) and uncomplicated aortic dissection (n=3). One patient died during surgery.
Discussion
The increased use of computed tomography in adult trauma patients has led to a rise in the identification of blunt traumatic abdominal wall injuries. However, the incidence of blunt abdominal aortic injury is much lower, occurring in only 0.03% to 0.07% of blunt traumas due to the abdominal aorta's greater protection. Conversely, blunt aortic injury is more common, affecting around 0.58% of blunt trauma cases, with the majority of these injuries occurring in the thoracic aorta (>95%) and resulting in aortic rupture and death on site. Notably, seat belt use accounts for only a third of all cases of blunt abdominal aortic injury.5,13
As it would be expected the most common injury to the aorta after blunt trauma was intimal dissection, which was the precursor in most cases of more severe complications such as false aneurysm formation, acute aortic thrombosis, and aortic rupture. This phenomenon, often results from sudden deceleration of the body during a high-speed accident causing the aorta to twist or stretch leading to mechanical stress on the aortic wall. Additionally, the seat belt can cause a sudden increase in intra-abdominal pressure, which can cause the aorta to expand and contribute to its dissection and rupture.4,13
Despite most patients arriving at the emergency department hemodynamically stable and conscient, the majority required some sort of urgent or emergent surgical intervention. The presence of hemodynamically instability at admission was related to more severe vascular lesions, with 5 out of the 9 patients that presented with hypovolemic shock, having complicated aortic dissections (3 with a ruptured aorta and another 2 with pseudoaneurysm formation).
At the opposite end of the spectrum, clinically stable and asymptomatic aortic lesions might be tempting to manage conservatively, yet it should be taken into consideration possible complications arising from blunt aortic trauma, namely intimal dissection and false aneurysm formation. In fact, among the 11 patients managed conservatively only 3 did not need any kind of vascular surgical intervention, 2 of which had a small intimal flap aortic dissection and 1 had a partial iliac thrombosis.
Regarding the treatment, despite a clear preference towards open surgery, one should take into consideration that most of the presented cases were reported in the last century, with only 11 reported cases in the last 10 years, which is likely a reflection of progressive improvements made in automotive safety and legislation on road and traffic security, although one cannot exclude that this may also be due to publication bias. Interestingly, if we analyse the procedures by year, only 2 aortoiliac thromboendarterectomies and 4 aortic graft interpositions were performed after 2000 versus 6 EVAR. Independently of the procedure, almost all patients had good results regarding their initial vascular lesions, with only 1 patient requiring reintervention.
Lastly, one should take into account the high morbidity and mortality associated with seat belt aortic injuries and especially seat belt triad, with almost 20% of 30-day mortality reported in our study. These patients were generally older (mean age 61 versus 43 years) and female, yet male death was associated with younger patients (54 years, male mean age versus 64 years, female mean age), which might be due to men being more frequently involved in more violent and higher-speed vehicle accidents.
Conclusion
Abdominal aortic injuries resulting from seat belt trauma, including the seat belt aorta and the seat belt triad, are serious medical conditions that can have life-threatening consequences, being associated with a high morbidity and mortality. Despite patients often presenting stable at admission, these injuries should not be disregarded. They require prompt recognition and management, often including multiple surgical interventions. As such, healthcare professionals should maintain a high degree of suspicion for these injuries and thoroughly evaluate patients who have been involved in high-speed motor vehicle accidents.