Background
Calciphylaxis or calcific uremic arteriopathy is a rare disease that occurs mainly in obese, female patients with end stage renal disease (ESRD). Clinical presentation usually starts with livedo-like skin lesions that become plaque-like or nodular, and then progress to severe painful and necrotic ulcers.1 It is associated with a high mortality rate (one-year mortality rate of 50-80% in ESRD patients) mainly due to infection of the ulcerated wounds leading to sepsis.2 Being a pathology that may be overlooked and vascular surgeons often being the first to investigate the cause of limb ulcers, this case report aims to alert to this differential diagnosis of leg ulcers.3
Case report
A 40-year-old woman with ESRD on haemodialysis, morbid obesity, severe arterial hypertension, atrial fibrillation (anticoagulated with apixaban) and secondary hyperparathyroidism was admitted to the vascular surgery department due to intolerable pain in her leg and foot ulcers. The patient suffered from cat scratches two months earlier at the site of the ulcers and developed a progressive worsening in extent and depth of the ulcers.
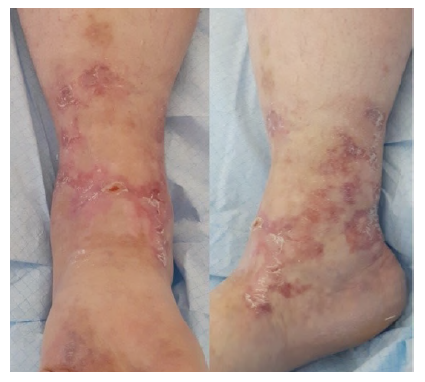
At admission, the patient had several lower limbs ulcers, including a deep ulcer with tendinous exposure of the extensor hallucis longus, measuring 4x4cm in its deepest area, with circumferential superficial involvement of the right limb (Figure 1). Despite atherosclerotic involvement of the tibioperoneal arteries, duplex ultrasound revealed biphasic curves in the tibial arteries in the right foot. The ankle-brachial index was carried out with a result of 1.1, obtaining a WIFi stage of 3 (2/0/2). Venous insufficiency and venous obstructive disease were excluded. Laboratory tests showed parathyroid hormone of 1104 pg/ml (11-79.5pg/ml), total corrected calcium of 9mg/dl (8.5-10.1mg/dl) and inorganic phosphate of 7.1mg/dl (2.5-4.9mg/dl).
A subcutaneous tissue biopsy was sent for microbiology, revealing infection with Serratia marcescens and Candida albicans. The patient was then initiated on intravenous antibiotic therapy with piperacillin/tazobactam and antifungal therapy with fluconazole. During hospitalization, glycaemic values remained normal, allowing a diabetic ulcer to be excluded. The patient had not travelled recently and had no history of immunosuppressive diseases.
Surgical debridement was then proposed, and a deep tissue biopsy was sent for histological analysis. This revealed "small thick-walled vessels with dystrophic calcification of the intima and media compatible with calciphylaxis” (Figure 2).
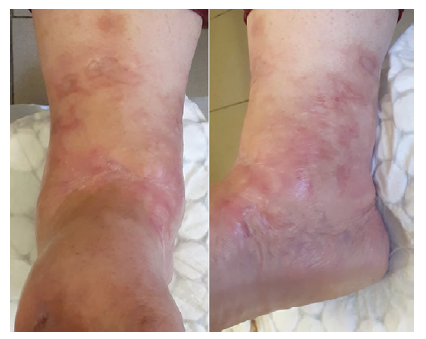
Wound care was continued after discharge with chemical debridement. Opioids were needed to control pain. The dialysis plan was readjusted with a reduction in dialysate calcium and introduction of sodium thiosulphate. Given the histological diagnosis obtained and the good healing progress with treatment aimed at calciphylaxis, other differential diagnoses were not investigated. The ulcers healed after 8 weeks (Figure 3) without recurrence in the 6 months follow-up (Figure 4).
Extensive leg ulcers including tendinous exposure (left) and several areas of necrotic tissue.

Figure 2 Histological analysis of deep tissue biopsy of the ulcer bed. A: Histologic findings of calciphylaxis in an abnormal vessel (arrow); B: Calciphylaxis in a small artery. The calcification affects the media and the intima is thickened by fibroplasia compromising the lumen (The intimal fibrosis has retracted from the stiffened calcified wall due to fixation artifact).
Discussion
Calciphylaxis has an estimated prevalence of 4,1-4,4% among haemodialysis patients in the western world. 1 Only 20% of the patients may not have ESRD. The average age of these patients is 60 years, and the majority are women and morbidly obese.4
The common clinical presentation usually starts with spontaneous livedo-like skin lesions that progress to severe painful and necrotic ulcer. Involvement of the lower extremities is the most common, however, the ulcers may also appear in the trunk and the upper limbs.1 The lesions, despite appearing spontaneously, can be triggered by skin trauma.
Although the pathogenesis of the disease remains unclear, a dysfunctional calcium-phosphate axis (secondary hyperparathyroidism) predisposing to diffuse calcification of the media of arterioles, micro-thrombosis and intimal hyperplasia is commonly accepted as pathogenic hallmarks.
A deep skin biopsy with subcutaneous adipose tissue is necessary to confirm the diagnosis. It should be considered for atypical ulcers that produce intolerable pain in dialysis patients. The most common finding is a septal calcifying panniculitis.1 The differential diagnosis should include peripheral arterial disease, venous hypertension, pyoderma gangrenosum, Martorell's ulcer and vasculitis, including systemic lupus erythematosus, antiphospholipid syndrome and cryoglobulinemia. Because of the high incidence rate of atherosclerotic vascular disease in patients with ESRD, it is essential to exclude underlying or concomitant vascular disease.3 Calciphylaxis has no clear guidelines regarding treatment. It relies on medical treatment to correct calcium/phosphate dysregulation, reduce pain and wound care. There may be an indication for parathyroidectomy in refractory cases to medical therapy. Regarding the regulation of calcium, vitamin D analogues and calcium supplements should be avoided, while calcium-reduced dialysate solutions (2.5-3mg/dl) and calcimimetics such as cinacalcet (that increase the sensitivity of the parathyroid cells calcium receptor decreasing PTH concentration) should be used.1 Additionally, the regulation of phosphate should be targeted with a phosphorus-reduced diet and phosphate-lowering drugs such as sevelamer. More recently, sodium thiosulphate administration either intravenously or by focal injection into ulcers has shown improvement in healing rates, due to its calcium chelating, anti-oxidative and vasodilator effects.5 The main side effects are nausea, vomiting, metabolic acidosis, volume overload, hypocalcaemia, and prolonged QT interval.5
Pain management is also important and may be challenging. Pain is considered to be triggered by skin ischemia but may also have a neuropathic component. Therefore, agents such gabapentin, ketamine and benzodiazepine can be useful.2 Opioids tend to accumulate in renal failure patients warranting cautious use. Lumbar sympathetic block may also be considered in refractory cases. 2
There are no specific recommendations in wound care, but some studies refer that hyperbaric oxygen therapy and bisphosphonates may be useful along with conservative debridement (surgically managed only if infected) and dressings.6 Complete wound healing is expected a few months after starting treatment.
It seems reasonable that surgical correction of underlying obstructive arterial disease, if present, may have an appropriate role, but such treatment should be individualized regarding the evolution of the ulcer with medical therapy3
The proposed diagnostic and therapeutic algorithms are shown in Figures 5 and 6 respectively.

Figure 5 Proposed diagnostic algorithm for end-stage renal disease patients on dialysis presenting with atypical leg ulcers

Figure 6 Proposed therapeutic algorithm for end-stage renal disease patients on dialysis presenting with atypical leg ulcers
To conclude, a high clinical suspicion is required to consider calciphylaxis in the differential diagnosis of patients with ESRD presenting with atypically painful limb ulcers. An expedite management is required as infectious complications may yield a poor prognosis. Vascular surgeons play an important role in this early diagnosis and exclusion of other causes of limb ulcers.