Introduction
Laparoscopic partial nephrectomy is increasingly practiced by urologists for localized renal lesions. Partial nephrectomy (PN), being a renal parenchyma-sparing technique, carries a lower risk of postoperative chronic kidney disease than total nephrectomy.1
Renal artery pseudoaneurysm and arteriovenous fistulas are rare, but potentially life-threatening complications after PN.2 Incidences of renal artery pseudoaneurysm following a laparoscopic PN of 1% to 2% have been reported, while this rate is less than 0.5% for open partial nephrectomy.3 Renal pseudoaneurysms can lead to severe hematuria, blood loss, and hemorrhagic shock.4
The authors present a case of a patient who developed a pseudoaneurysm after PN treated with embolization.
Case report
A 67-year-old female with a prior history of stroke and acute glaucoma underwent a laparoscopic partial left nephrectomy (ischemic time: 30 minutes) due to an early-stage renal adenocarcinoma. The initial procedure was uneventful. However, gross macroscopic haematuria appeared suddenly one month after, associated with lipotimia. At admittance, the patient had hemodynamic repercussion (hypotension, tachycardia) and acute anemia with a serum hemoglobin level of 6.9g/dl. Computerized tomography angiography (CTA) detected a 20x10x10mm pseudoaneurysm in the surgical site (Figure 1). Intervention to stop the bleeding was considered emergent and an endovascular solution was proposed.
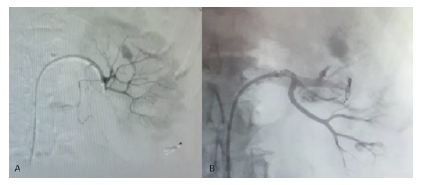
Through a 5F femoral access, the patient underwent a renal angiogram using a cobra catheter (Terumo®) which confirmed the large pseudoaneurysm in a segmental artery close to the renal hilum. After super-selective catheterization, embolization of the culprit segmental artery with coils (ConcertoTM Helix Detachable) and plug (Micro Vascular Plug - Medtronic®) was performed (Figure 2). The final angiography showed effective exclusion of the pseudo-aneurysm and good perfusion of the remaining renal parenchyma. Discharge was on the 5th postoperative day, after full recovery of kidney function, with a serum creatinine of 0,73mg/dl.

Figure 1 Pre-operative computed tomography angiography (coronal view) revealing a pseudo-aneurysm on the left kidney.
Discussion
Pseudoaneurysms and arteriovenous fistulas are rare post-operative complications of PN. Risk factors related to the development of pseudoaneurysms after PN are large tumors, high nephrometry score, and tumors that required exposure of the renal sinus or in which the collecting system was opened.5
Gross haematuria and flank pain are the most common symptoms that raise the suspicion of vascular lesion occurring most frequently within the 3 weeks after the surgery.3
For the diagnosis of renal pseudoaneurysms, CTA is the most frequently used exam. Alternatively, contrast-enhanced ultrasound or magnetic resonance imaging could be performed.5 Attention should be given to the fact that these patients have chronic kidney disease and in whom the use of contrast is not innocuous. Ultrasound can show the degree of clotting, the culprit vessels feeding the pseudoaneurysm and typical “to-and-fro” waveform.5
Management of renal pseudoaneurysm may vary from conservative therapy, to minimally invasive angiographic embolization or be treated with total nephrectomy. Selective embolization is usually the choice because not only it is a safe procedure with technical and clinical success rates of 95-100%, but also allows renal parenchyma sparing when compared to nephrectomy. Although some renal parenchyma is lost due to embolization, this did not result in a decrease in renal function in our patient.4
To conclude, while close follow-up of the patients after PN should be done to timely diagnose life-threatening vascular complications, pseudoaneurysm embolization was shown to be effective in the management of secondary haematuria to a renal pseudoaneurysm.