Introduction
Trauma is the most common cause of death in young adults, with blunt thoracic aortic injuries (BTAI) being described as the second most prevalent cause in high-energy accidents after head injury.1,2
BTAI is characterized by an aorta tear resulting from a high-energy blunt trauma with sudden deceleration and increased intravascular pressure,3 typically in motor vehicle accidents or falls from a considerable height.4 The injury mainly occurs at the aortic isthmus, the portion of the thoracic aorta most susceptible to excessive stretching.
This is a rare type of lesion that accounts for 1-2% of all thoracic traumas, but it is potentially lethal, with up to 80% mortality before hospitalization and 46% in-hospital mortality.1,3,5
The initial diagnosis is challenging because these polytrauma patients often have other life-threatening injuries,2 and presentation can vary from an asymptomatic intimal tear to significant hemodynamic instability or hemorrhagic shock from an aortic rupture.6
The severity classification system for BTAI evaluates these lesions in 4 grades based on computed tomography angiography (CTA) imaging: type I (intimal tear), type II (intramural hematoma), type III (pseudoaneurysm), and type IV (rupture).7,8
In recent decades, thoracic endovascular aortic repair (TEVAR) has become the standard of care for BTAI.9-11 It is the primary treatment recommended by the Society for Vascular Surgery (SVS) and the European Society for Vascular Surgery (ESVS) guidelines for the management of BTAI, if the patient has suitable anatomy.7,12 TEVAR has better short-term outcomes compared to open surgery repair (OSR), with higher survival rates and decreased risk of spinal cord injury and paraplegia.8,13,14 However, there are still some concerns about the long-term results and durability of TEVAR. Although OSR is associated with increased perioperative morbidity and mortality rates,13,15,16 it could be a good option for patients whose anatomy and injury location are not suitable for endovascular treatment.
Other aspects, such as managing minimal aortic injuries (grade I), graft selection and oversizing, optimal timing of aortic repair, and coverage of the left subclavian artery (LSA), have been subject to controversy.
The purpose of this study was to analyze and report our last 4-year center’s experience in the treatment of blunt traumatic injuries of thoracic aorta and supra-aortic trunks.
Methods
We retrospectively reviewed our institutional database to identify all patients treated for blunt traumatic injuries of the thoracic aorta and supra-aortic trunks in our level-one trauma center from January 2018 to December 2021, and the follow-up period ranged from three to 24 months. ICD-9 codes (9010; 9011; 38.44; 39.31; 39.73; 39.90) were used to ensure no missing subjects. Data were extracted from patients’ medical records. Patients’ demographics, injury mechanism, grade of aortic injury, treatment details, time to intervention, length of hospital stay, and postoperative morbidity and mortality rates were extracted. A descriptive analysis of all the data was performed.
Advanced trauma life support (ATLS) guidelines were followed at the initial evaluation by an emergency team. Chest radiography and CTA were performed in all patients. Traumatic aortic injuries were categorized using the SVS classification: type I (intimal tear), type II (intramural hematoma), type III (pseudoaneurysm), and type IV (rupture).7,8
The vascular surgery team made decisions based on clinical and radiological factors on management modality (non-operative, endovascular intervention, or open surgery) and timing for intervention.
Results
A total of six patients with blunt traumatic injuries of the thoracic aorta presented to our level-one trauma center in the 4-year period of this retrospective report.
The mean age was 29 years (range 19-34 years), and 83.3% of patients were male. The demographic characteristics and comorbidities of the selected patients are described in Table 1. The mechanism of injury was a high-energy motor vehicle accident for all cases. The most common injury grade was type III (pseudoaneurysm) in five patients (83.3%), and one patient presented with a type IV aortic injury with rupture. No type I or II lesions were observed in this group of patients. All the traumatic injuries were in the aortic isthmus at the descending thoracic aorta, and all BTAI diagnoses were made on CTA imaging, Figure 1.
In our cohort, all six patients were suitable for TEVAR procedure. None were managed nonoperatively. Mean time to intervention was seventeen days (range 1-81 days). The patient with higher grade of injury (grade IV) was submitted to emergent TEVAR at admission. Grafts used in each procedure and its measures are presented on Table 2. Mean oversizing percentage was 11%, varying between 5% and 24%. Cerebrospinal fluid drainage was not performed in any patient and there were no neurological symptoms detected postoperatively related to TEVAR or OSR.
Two patients had coverage of their LSA, one complete and the other partial coverage. The patient with complete LSA coverage had recurrent episodes of dizziness postoperatively due to subclavian steal syndrome (reversion of vertebral artery flow seen on Doppler ultrasound), with resolution of symptoms before discharge. The other patient with partial LSA coverage had no clinical consequences. No other complications related to vascular intervention were observed. One patient in our cohort (patient number 2) also presented with acute limb ischemia due to an embolus from a mural thrombus in the descending aorta. Therefore, an emergent femoral embolectomy was done before the TEVAR procedure.
The mean length of hospital stay was 54 days (range 21-133 days). No deaths occurred in the hospital or during the follow-up period, and there were no registered vascular procedure-related morbidities, such as endoleaks, endograft migration or collapse, upper extremity limb ischemia, spinal cord ischemia, or post-implantation syndrome.
Table 1 Patients’ demographic, presentation details, and diagnosis method.
| ID | Age (years) | Sex | Year | Comorbidities | Mechanism of injury | Location of injury | Grade of injury | Diagnosis method |
| 1 | 34 | Male | 2018 | - | Motor vehicle accident | DAo (aortic isthmus) | III (pseudoaneurysm) | CTA |
| 2 | 27 | Female | 2019 | Hypertension Obesity | Motor vehicle accident | DAo (aortic isthmus) | III (pseudoaneurysm) | CTA |
| 3 | 19 | Male | 2020 | - | Motor vehicle accident | DAo (aortic isthmus) | III (pseudoaneurysm) | CTA |
| 4 | 27 | Male | 2020 | - | Motor vehicle accident | DAo (aortic isthmus) | IV (rupture) | CTA |
| 5 | 32 | Male | 2021 | Psoriasis | Motor vehicle accident | DAo (aortic isthmus) | III (pseudoaneurysm) | CTA |
| 6 | 32 | Male | 2021 | - | Motor vehicle accident | DAo (aortic isthmus) | III (pseudoaneurysm) | CTA |
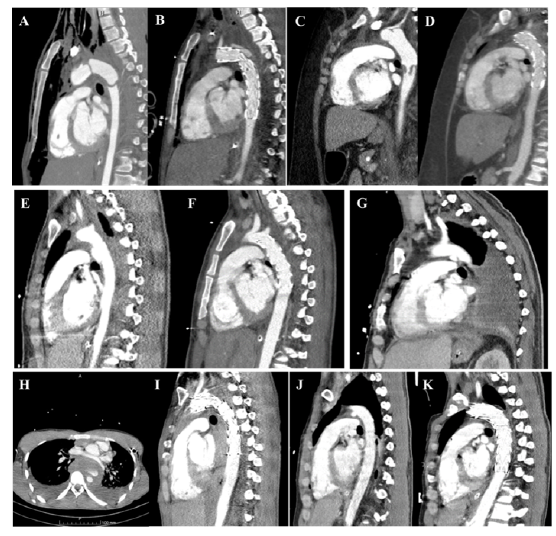
Figure 1 Pre- and post-operative contrast-enhanced computed tomography images of traumatic thoracic injuries. A & B - patient number 1; C & D - patient number 2; E & F - patient number 3; G - patient number 6; H & I - patient number 4; J & K patient number 5
Table 2 Treatment details and outcomes.
| ID | Treatment | Timing for treatment | Graft | Oversizing | Cerebrospinal fluid drainage | LSA coverage | Length of hospital stay (days) | Follow-up (months) | Postoperative complications |
| 1 | TEVAR | Day 6 | Medtronic Valiant Captivia® 26x150mm | 13% | No | No | 45 | 7 | - |
| 2 | TEVAR | Day 4 | Medtronic Valiant Captivia® 22x150mm | 5% | No | No | 31 | 24 | - |
| 3 | TEVAR | Day 3 | Medtronic Valiant Navion® 20x94mm | 5% | No | No | 44 | 12 | - |
| 4 | TEVAR | Day 1 | Medtronic Valiant Captivia® 26x150mm | 24% | No | Yes (complete) | 21 | 18 | Subclavian steal syndrome with dizziness |
| 5 | TEVAR | Day 6 | Medtronic Valiant Captivia® 26x150mm | 8% | No | No | 52 | 12 | - |
| 6 | TEVAR | Day 81 | GORE TAG® 24x100mm | 9% | No | Yes (partial) | 133 | 3 | - |
TEVAR - thoracic endovascular aortic repair; RSA - right subclavian artery
Discussion
Although there are some studies with acceptable outcomes with OSR,18 other reports showed considerable mortality rates and risk of paraplegia.19 Conversely, TEVAR has become the first-line treatment for BTAI when suitable anatomy is present, with good short- and mid-term outcomes.8,19-21 In fact, TEVAR has been shown to reduce mortality rates and decrease the incidence of paraplegia in various reports.22,23 However, the potential long-term durability and efficiency of TEVAR remain uncertain. In a recently published cohort study of 287 patients in Taiwan, Cheng et al. found that TEVAR was associated with better long-term outcomes, mainly due to lower mortality rates in the perioperative period, compared with OSR. In addition, TEVAR was associated with similar survival and reintervention rates after hospital discharge.15
The appropriate timing for the intervention in patients presenting with BTAI is still an aspect of controversy. A study from 1997 showed that in most patients with BTAI who progressed to rupture (grade IV), it happened in the first 24 hours.24 For many years, immediate intervention was considered the best therapeutic option for all these patients. However, more recent studies found better outcomes for delayed intervention (after 24 hours), with decreased mortality and paralysis rates, compared to early treatment (within 24 hours).19,25 Demetriades et al. reported benefits from delayed intervention in patients with BTAI and concomitant major injuries requiring stabilization.20 ESVS guidelines recommend emergent repair in patients with BTAI and free rupture (grade IV) or peri-aortic hematoma ≥15mm. If this is not the case, delayed intervention should be considered to allow treatment of other life-threatening injuries.12 Delayed repair also has the benefit of providing more accurate stent graft measurements on CT imaging after complete resuscitation of the patients. In our cohort, we followed the current guidelines, and delayed intervention was performed in five of the seven patients to allow for the stabilization of other associated serious injuries. Emergent intervention was performed in a patient with free aortic rupture and concomitant massive bilateral hemothorax with over 3000cc of drained blood through the bilateral thoracic drains.
There are also controversies around ideal stent graft oversizing. Oversizing around 10% is recommended for most patients with BTAI. More aggressive oversizing between 10-20% should be considered for patients with considerable hypotension to avoid inadequate undersizing, with risk of endoleak and graft migration, once full resuscitation is achieved.26 Oversizing of >20% can be an option in patients with severe hypotensive hemorrhagic shock, but it entails a risk of device collapse if the oversizing proves to be excessive.27 Accordingly, in our center's experience, we chose a stent graft oversizing around 10% in most patients (5-13%). In the patient presenting with grade IV BTAI and hemorrhagic shock, an oversizing of 24% was chosen.
Recent articles report the necessity of LSA coverage in 30% of TEVAR for urgent treatment of BTAI.23 A 20mm proximal seal zone is recommended, which can result in the need for LSA coverage. In a recent retrospective study published in 2021 with 61 patients who underwent TEVAR for BTAI treatment, LSA coverage, when needed, was well tolerated. However, the long-term outcomes of LSA coverage are still unknown.28 For patients submitted to urgent or emergent TEVAR needing LSA coverage, the decision of revascularization should be individualized.29 In this cohort, LSA coverage was performed in two patients, and no sequelae were reported in the post-discharge follow-up.
Contrastingly, BTAI grade I lesions presenting with intimal tear can be managed expectantly with serial surveillance CT imaging.17
This retrospective study has some limitations. First, we only collected data about patients who underwent intervention. For this reason, we could have missed some BTAI grade I cases treated conservatively. Second, patient number seven, who was treated more recently, has a shorter follow-up period and still has no follow-up CT imaging.
Conclusions
This study reports our level one trauma center experience in the management of BTAI, which is in accordance with current international guidelines. All patients underwent CTA for diagnosis and grading of aortic injury and all patients who needed intervention underwent TEVAR, if anatomically suitable.
TEVAR proved to be effective in the treatment of BTAI, with few complications and good outcomes at short and mid-term follow-up, and it should be the first-line treatment for these patients. OSR should be an option when a patient’s injury has anatomical features that are not suitable for endovascular approach. More large-scale studies are warranted to clarify some controversies surrounding graft selection and oversizing, optimal timing of aortic repair and management of the LSA.















