Introduction
Premature peripheral artery disease (PAD) is a poorly studied disease with a rising global prevalence, defined as the onset of PAD occurring before or at the age of 50. Etiology is multifactorial and includes both genetics and environmental causes.1 The most common known risk factors are not different than PAD in general and include smoking, diabetes, hypertension, and chronic kidney disease.1-6) Atypical risk factors that might be at play are still relatively unknown.7 Premature PAD is associated with an aggressive form of atherosclerosis with poor outcomes - patients have a higher risk of progression to chronic limb-threatening ischemia (CLTI), undergo more reinterventions and have higher amputation and mortality rates than their older counterparts.4-10 The aim of this study was to investigate the demographics and outcomes of revascularization procedures for CLTI in patients with premature PAD.
Methods
A prospectively maintained single-center database from a tertiary academic institution was retrospectively enquired regarding a study period of 12 years, from May 2011 to November 2023.
Study population
Ninety-one patients 50 years old or under who underwent a primary revascularization procedure for CLTI from May 2011 to November 2023 were included. Both open surgery and endovascular procedures were included. Patients who had previously been submitted to a revascularization procedure outside the considered time frame or those who underwent primary amputation were excluded.
Data collection
An institutional medical record review was performed, and baseline characteristics, clinical presentation, and procedural and follow-up data were obtained. Reintervention was defined as a subsequent vascular revascularization procedure performed on the same limb due to clinical-driven restenosis/occlusion associated with recurrence/maintenance of symptoms of CLTI. Major amputation was defined as either transfemoral or transtibial amputation.
Endpoints
The primary endpoint was a composite outcome of reintervention, amputation and/or mortality. The secondary endpoints were reintervention, amputation and mortality rates, and amputation-free survival. Two subgroup analyses were performed, comparing diabetic and non-diabetic patients, and endovascular and open revascularization procedures.
Statistical analysis
Descriptive statistics were used to report data. Continuous data were presented as mean ± standard deviation or median (interquartile range). Kolgomorov-Smirnov and Shapiro-Wilk tests were used to assess data distribution normality, and the Student t-test or Mann-Whitney U statistics were used, respectively, to compare continuous Gaussian and non-Gaussian data. Dichotomous variables are expressed as counts (percentages) and compared between groups using Pearson’s chi-square test. Survival curves for endpoints were estimated by Kaplan-Meier plots, and equality between groups was evaluated with the Mantel-Cox log-rank test. All statistical tests were two-sided and considered statistically significant when the p value was <.05. All analyses were performed using IBM SPSS Statistics version 29.0 software.
Results
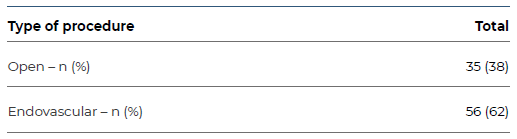
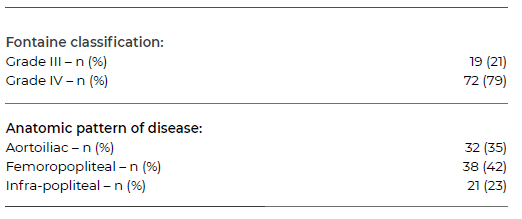
Between May 2011 and November 2023, ninety-one patients (74% male, 26% female) with a median age of 48 (44-49) years were submitted to a primary revascularization procedure at our institution. Baseline characteristics are depicted in Table 1. The most commonly associated comorbidities were smoking (n=63, 69%), diabetes mellitus (n=41, 45%) and hypertension (n=40, 44%). Seventy-two patients (79%) presented with either ulceration or gangrene - Fontaine grade IV - while 19 (21%) patients presented with rest pain - Fontaine grade III, Table 2. Most patients underwent an endovascular procedure (n=56, 62%), Table 3.
Table 1 Baseline characteristics of patients 50 years old or under submitted to a primary revascularization procedure for CLTI.
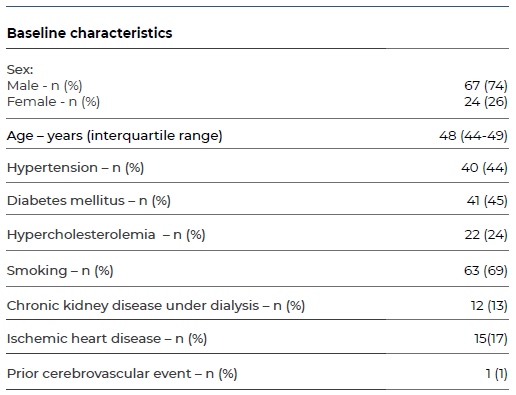
Table 2 Clinical grading and anatomic pattern of disease of patients 50 years old or under submitted to a primary revascularization procedure for CLTI.
The median follow-up period was 7.4 (4.3-10.3) years. The composite endpoint of reintervention, amputation and/or mortality occurred in 57 (63%) patients. Individually, 36 (40%) patients underwent a reintervention procedure, 23 (25%) were submitted to major amputation, and 26 (29%) patients died. Median time for freedom from amputation was 4.7 (0.8-7.8) years, Table 4.
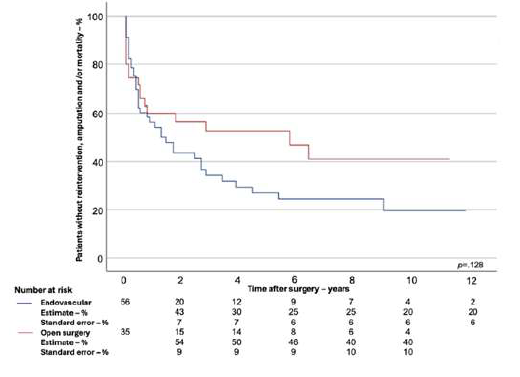
The two-year estimates for freedom from reintervention, amputation and/or mortality were 47%, while the six and ten-year estimates were 33% and 28%, respectively (Figure 1).
Two subgroup analyses were performed. Firstly, diabetic (n=41, 45%) and non-diabetic (n=50, 55%) patients were compared. Diabetic patients had higher rates of hypertension (59% vs. 32%, p=.011) and chronic kidney disease under dialysis (22% vs. 6%, p=.025) but lower rates of smoking (49% vs. 86%, p<.001), Table 5. Patients presenting with ulceration or gangrene - Fontaine grade IV - and those who underwent an endovascular procedure were more frequently diabetic (68% vs. 93%, p=.004; 52% vs. 74%, p=.039; respectively). On the contrary, patients presenting with rest pain - Fontaine grade III - and those who were submitted to an open revascularization surgery were more frequently non-diabetic (32% vs. 7% - p=.004; 48% vs. 27%, p=.039; respectively), Tables 6 and 7.
At 30 days, diabetic patients had a non-statistically significant higher rate of reintervention, amputation and/or mortality (8% vs. 20%, p=.106). There were also no statistically significant differences in reintervention and mortality rates individually, except for the 30-day amputation rate, which was higher in diabetic patients (12% vs. 2%, p=.05), Table 8.
Freedom from reintervention, amputation and/or mortality estimates in the second year was 42% vs. 52%, in the sixth year 28% vs. 36%, and in the tenth year 22% vs. 32%, in the diabetic vs. non-diabetic groups, respectively (Figure 2). Visual analysis of Kaplan-Meier curves suggested higher freedom from reintervention, amputation and/or mortality in non-diabetic patients. However, this difference was not statistically significant (p=.210).
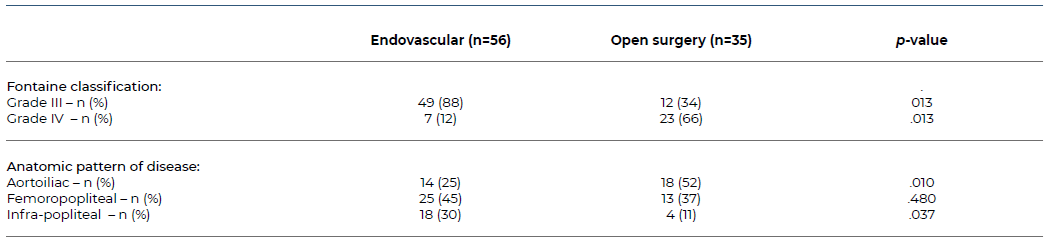
Lastly, a subgroup analysis was performed comparing endovascular procedures (n=56, 62%) and open revascularization surgery (n=35, 39%). Patients submitted to an endovascular procedure had higher rates of hypertension (54% vs. 29%, p=.019), diabetes (54% vs. 31%, p=.039), and chronic kidney disease under dialysis (21% vs. 0%, p=.003) - Table 9. Patients presenting with rest pain - Fontaine grade III - or an infra-popliteal anatomical disease pattern more frequently underwent an endovascular procedure (88% vs. 34%, p=.013; 30% vs. 11%, p=.037; respectively). Conversely, patients presenting with ulceration/gangrene - Fontaine grade IV - or an aortoiliac anatomical pattern of disease were more frequently submitted to an open revascularization procedure (13% vs. 66%, p=.013; 25% vs. 51%, p=.10; respectively), Table 10.
Table 4 Outcomes for patients 50 years old or under submitted to a primary revascularization procedure for CLTI.
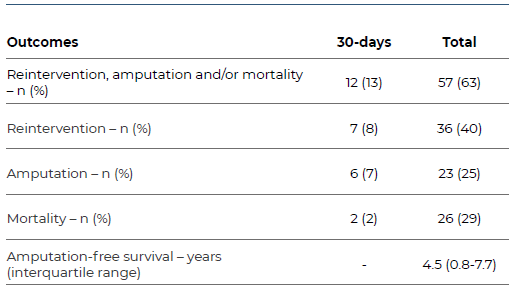
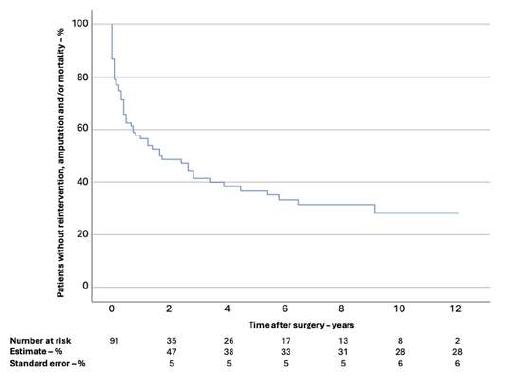
Figure 1 Kaplan-Meier estimate of freedom from reintervention, amputation and/or mortality in patients 50 years old or under submitted to a primary revascularization procedure for CLTI.
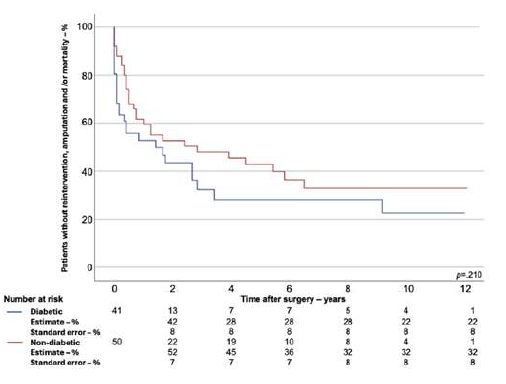
Figure 2 Kaplan-Meier estimate of freedom from reintervention, amputation and/or mortality in diabetic and non-diabetic patients 50 years old or under submitted to a primary revascularization procedure for CLTI.
Table 5 Baseline characteristics of diabetic and non-diabetic patients 50 years old or under submitted to a primary revascularization procedure for CLTI.
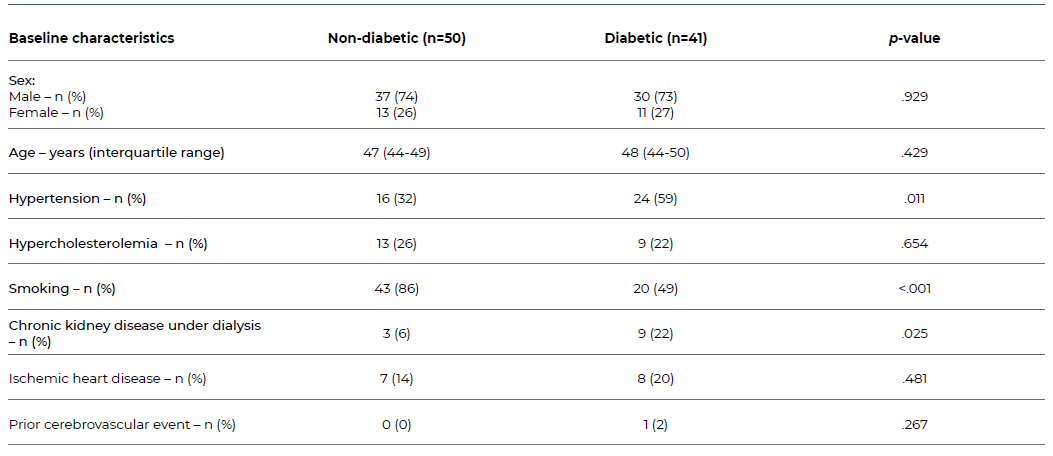
Table 6 Clinical grading and anatomic disease pattern of diabetic and non-diabetic patients 50 years old or under submitted to a primary revascularization procedure for CLTI.
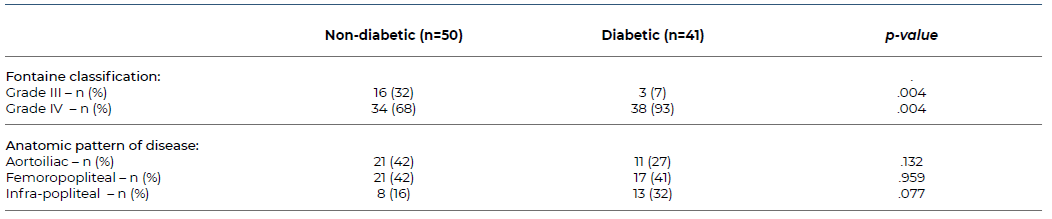
Table 7 Type of revascularization procedure performed in patients 50 years old or under, stratified by the presence of diabetes.
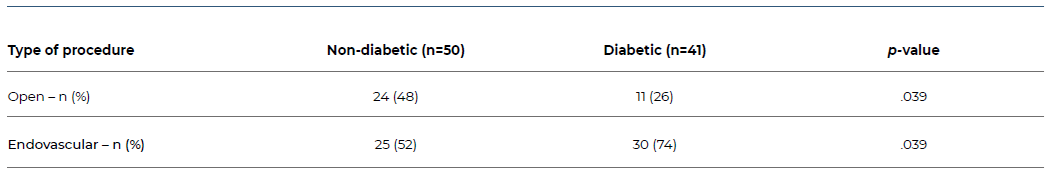
Table 8 Outcomes for diabetic and non-diabetic patients 50 years old or under submitted to a primary revascularization procedure for CLTI.
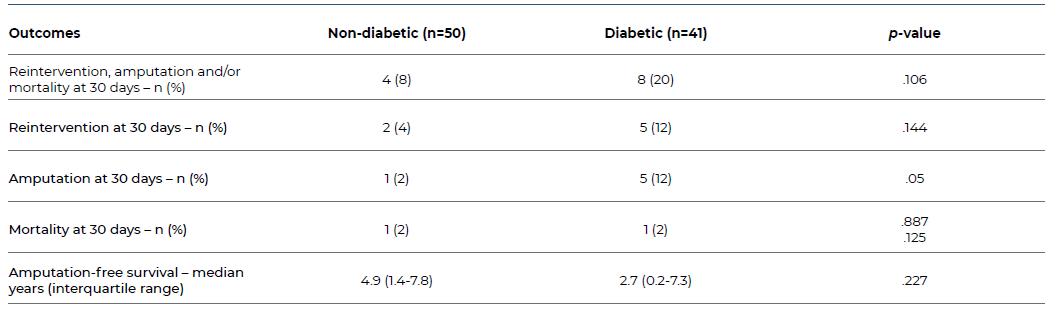
Table 9 Baseline characteristics of patients 50 years old or under submitted to a primary revascularization procedure (endovascular vs. open surgery) for CLTI.
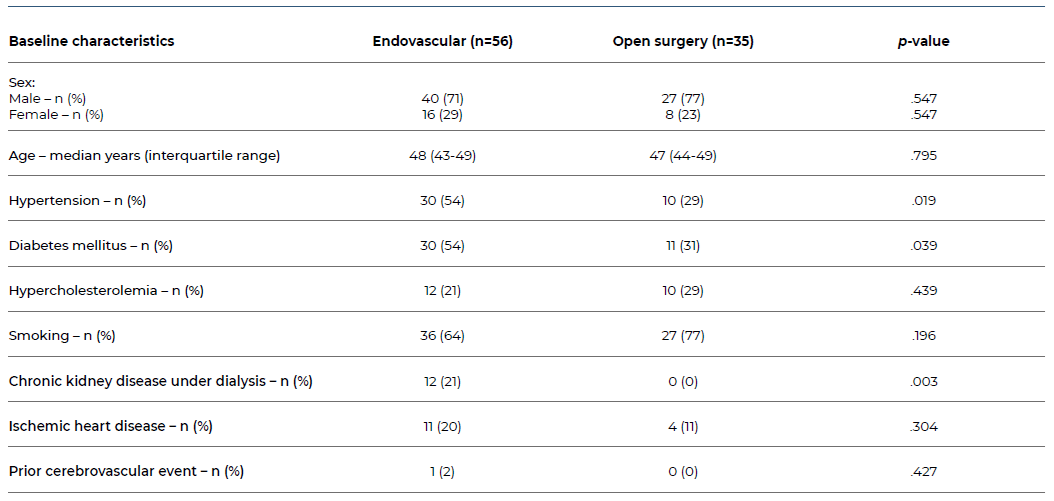
Table 10 Clinical grading and anatomic disease pattern of patients 50 years old or under submitted to a primary revascularization procedure (endovascular vs. open surgery) for CLTI.
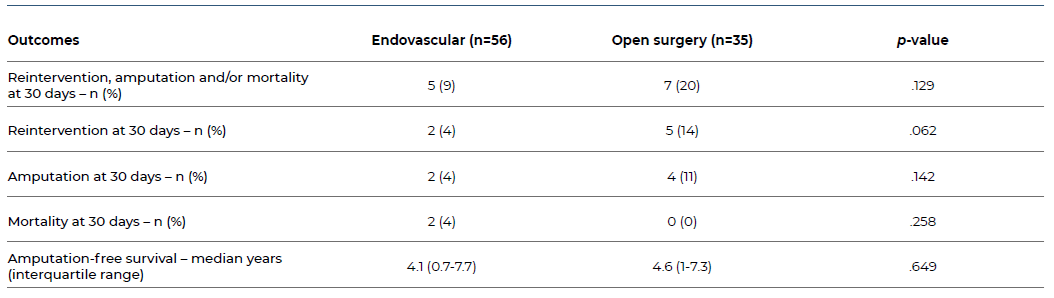
Patients submitted to an open revascularization surgery had a non-statistically significant higher 30-day rate of reintervention, amputation and/or mortality (20% vs. 8.9%, p=.129). There were also no statistically significant differences in reintervention, amputation, or mortality rates individually (Table 11). Freedom from reintervention, amputation and/or mortality estimates in the second year was 43% vs. 54%, in the sixth year 25% vs. 46%, and in the tenth year 20% vs. 40%, in the endovascular vs. open surgery groups, respectively (Figure 3). Visual analysis of Kaplan-Meier curves suggested an overall higher freedom from reintervention, amputation and/or mortality from the second year onwards in open surgery patients. However, in global, differences between the curves were not statistically significant.
Table 11 Outcomes for patients 50 years old or under submitted to a primary revascularization procedure (endovascular vs. open surgery) for CLTI.
Discussion
As the global prevalence of premature peripheral artery disease is on the rise, its recognition, early diagnosis, and effective treatment are of great importance, especially considering the particularities of this young, active population.
In this study, the most common risk factors for CLTI in patients 50 years old or under were smoking, diabetes, and hypertension. This aligns with previous studies, which also pointed out these as the most frequently found comorbidities in this population.1-6 While reported smoking rates range from 54% to 61%, our population was found to have a higher prevalence of smokers (69%).4-5 As for hypertension and diabetes, our findings were similar to results from the literature, which report a 42-79% rate of hypertension and 25-59% of diabetic patients.3-4),(6-7 Interestingly, previous studies report female sex as a risk factor for premature PAD, with a 41-50% rate of female patients throughout studies.2),(5 This is considerably higher than in our population and may be explained by a demographic bias due to differences in populations and respective associated habits and comorbidities. Ischemic heart disease was also reported as frequent in premature PAD patients and associated with long-term mortality. That, along with chronic kidney disease, has been proposed as effective in identifying patients at risk for premature PAD in the general population.2),(6),(10 Other described risk factors in literature that were not evaluated in our study due to its retrospective design were race, lipoprotein(a) and hypercoagulability, and systemic inflammatory markers.5),(7
A composite primary endpoint of reintervention, amputation, and/or mortality was selected in this study, given that any of these outcomes is highly deleterious in the life of a young patient. Previous studies report a higher rate of worse limb-related outcomes in young patients submitted to revascularization procedures for premature PAD, such as higher major amputation rates and lower amputation-free survival.4-6),(8-9 A study by Kim et al. reported a 3% 30 day amputation rate in CLTI patients under 50 compared to 1% in patients over 80 years old, which is lower than the rate we reported.4 However, amputation-free survival appears to be lower in older patients.4 This may be due to a lower threshold for opting for amputation in more elderly patients.
Regarding reintervention, patients with premature PAD are also at higher risk for reintervention. Indeed, a different study by Kim et al. reports lower freedom from reintervention at 1 year (87% ± 0.5) in this subset of patients compared to older counterparts (90.3% ± 0.2).5 While this may be explained by a longer life expectancy, allowing time to develop the need for reintervention compared to older patients, studies also indicate that this may be due to a more aggressive atherosclerosis pattern in younger patients.
As for mortality, studies overall confirm a high mortality rate in these patients due to an increase in all-cause mortality.4,6 A large study on this topic reports a 19% mortality rate in a mean follow-up period of 5.6 years.6In our study, the mortality rate was 29% in a mean follow-up period of 7.4 years. Contrastingly, one of the previously mentioned studies by Kim et al. indicates a lower mortality rate in premature PAD patients when compared to an older population but suggests this may be a biased result as older patients are more likely to die from other causes not directly related to PAD.5 Nonetheless, the persistently elevated rates throughout years are suggestive of a need for improvement in long-term mortality.
In our study, a subgroup analysis between diabetic and non-diabetic patients was performed. Higher rates of hypertension and chronic kidney disease under dialysis were found in diabetic patients. There is a recognized association between diabetes and higher major adverse limb events and mortality in previous studies.3-5 Despite finding no statistically significant differences between the primary endpoint, reintervention or mortality in our population, a significantly higher 30 day amputation rate was found in the diabetic subgroup.
A different subgroup analysis was also performed, comparing patients who underwent endovascular and open surgery revascularization procedures. Patients who were submitted to an endovascular procedure had higher rates of several comorbidities, such as hypertension, diabetes, and chronic kidney disease under dialysis. This may be due to the more commonly distal anatomical disease pattern found in diabetic patients, which is more frequently treated by endovascular means in our context. Another reason may be the preference for a lower-risk procedure in patients who are considered to be at a higher surgical risk due to their previous medical history. Previous studies report conflicting outcomes between these subgroups, with a general tendency for worse outcomes after endovascular procedures. A study by Madigan et al. regarding outcomes after revascularization procedures for aortoiliac disease showed lower one-year reintervention, amputation, and major adverse limb events rates in patients submitted to open surgery after propensity score matching.8 Other studies report higher amputation rates in patients submitted to endovascular procedures when compared to open or hybrid procedures, despite no differences in reintervention or mortality rates.4),(11 In our study, there were no statistically significant differences in reintervention, amputation and mortality, both individually and jointly, but results were tendentially worse in the endovascular group.
This study has certain limitations. Firstly, it was a single-center retrospective study with unavoidable associated biases. Secondly, the small sample size likely limited the ability to demonstrate statistically significant differences in outcomes in the subgroup analysis. Lastly, a comparison between patients with premature CLTI and older patients was not performed due to data collection constraints, which limited outcome analysis and underpowered this study.
Conclusion
Premature CLTI is associated with high amputation, reintervention and mortality rates. This appears to be even more significant in patients with concomitant diabetes or submitted to an endovascular procedure, despite no statistically significant difference in outcomes having been noted in our population. The most common risk factors include smoking, diabetes and hypertension, which is similar to PAD in general. Further research is needed to identify non-traditional target risk factors, such as genetics or environmental factors, to more easily identify and improve outcomes in this young population.