Introduction
Splenic artery aneurysms (SAA) are the most frequent (50 to 75%) abdominal visceral arterial aneurysms. In autopsy studies, the overall incidence is 0.01%, increasing to 10.4% with age. Although incidence rises markedly in the elderly, they occur at a younger age than other splanchnic aneurysms.1
Unlike other arterial aneurysms, SAAs exhibit a notable gender disproportion, affecting females at a ratio of 4:1 compared to males.2,3 The etiology of true splanchnic aneurysms includes various factors such as atherosclerosis, medial degeneration, collagen vascular diseases, and fibromuscular dysplasia. Additionally, risk factors such as multiparity, portal hypertension, and post-transplant status contribute to their development.4 Most SAAs are saccular in shape and are typically found more frequently in the mid- or distal splenic artery and its bifurcations.5
Abdominal radiography, Doppler ultrasound (DUS), computed tomography angiography (CTA), magnetic resonance angiography (MRA), and arteriography can detect SAA. Still, according to the SVS guidelines,6 CTA remains the preferred initial diagnostic and evaluative tool. Pilleul et al.'s comparison of MRA and CTA for analyzing splanchnic aneurysms revealed that MRA's sensitivity was suboptimal, particularly for small aneurysms.7
SAAs can manifest as multiple lesions and may coexist with other visceral and non-visceral aneurysms. In a review of 212 SAA cases, 3.3% of patients presented with concurrent visceral aneurysms, with the most common locations being extrahepatic, including aneurysms in the celiac, superior mesenteric, gastric, and pancreaticoduodenal territories. Additionally, 14.3% of patients had concurrent non-visceral aneurysms, with the most frequent locations being renal and the abdominal aorta.8
Reports indicate that symptomatic SAAs or those associated with rupture tend to present at an average maximum diameter of around 3 cm.9,10 In up to 25% of cases where SAAs rupture, the initial rupture may be confined within the lesser sac. This phenomenon, known as "double rupture," occurs when splenic artery hemorrhage is initially contained within the lesser sac before subsequent free rupture into the retroperitoneum, sometimes up to four days later.11 Rupture commonly occurs in pregnant women, particularly in the third trimester, with only three reported cases of first-trimester rupture documented in the literature.12
For patients undergoing urgent ligation of SAA or splenectomy, vaccination should be administered on or after postoperative day 14 to mitigate the risk of overwhelming post-splenectomy sepsis caused by pathogens such as Streptococcus pneumoniae, Haemophilus influenzae type B, and Neisseria meningitidis. Additionally, patients undergoing elective repair of SAA who face the possibility of splenic loss should be considered for vaccination at least 14 days before the intervention.4
For the management of SAAs, both proximal and distal ligation of the aneurysm segment is considered a feasible open surgical (OS) approach, thanks to visceral collateralization. Endovascular techniques (ET) offer another option that can be achieved by implanting a stent graft or coil embolization. Endovascular intervention can utilize various methods, often in combination, such as coil and glue deployment, particle or absorbable hemostatic gelatin injection, placement of covered or flow-diverting stents, and injection of thrombin or ethyl alcohol.13
As there is a lack of data due to rarity, our aim was to perform a systematic review of available data on SAAs.
Methods
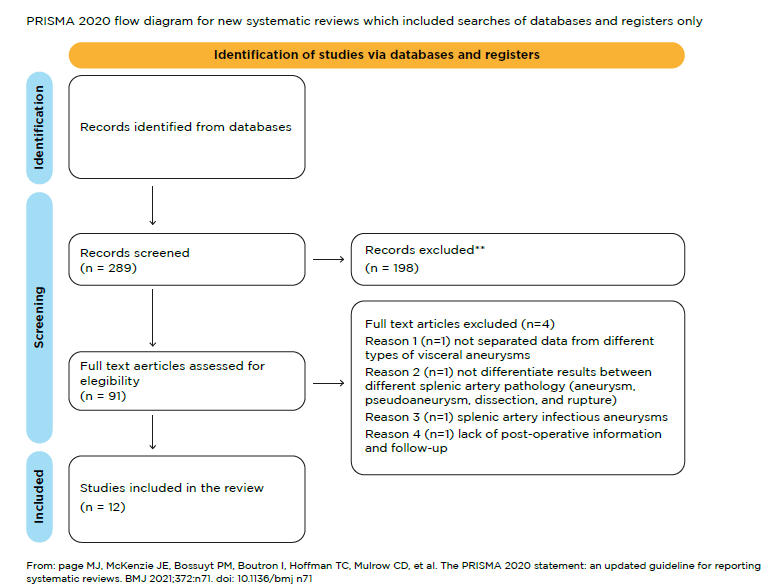
A systematic review was performed according to the PRISMA statement.14 A literature search was performed in the Medline database in the last five years, from January 2019 to January 2024, using the following “keywords” (visceral OR splanchnic OR splenic) AND (aneurysm).
We searched for manuscripts reporting treatment outcomes for patients with SAA published in the last 5 years. Portuguese and English articles were included. Non-English articles were included when an English abstract with extractable data was provided.
Inclusion criteria were selected as follows:
(i) patients with true SAA;
(ii) treatment of SAA by endovascular and/or open surgical means;
(iii) at least intraoperative and/or early extractable results (at least one of the following outcomes: peri-operative complications, reinterventions, and 30-day mortality).
Exclusion criteria included:
(i) etiology other than atherosclerotic/degenerative, such as post-traumatic, post-dissection, infection, or connective tissue disease;
(ii) aneurysms only followed clinically, not treated with intervention;
The data extracted were study design (type of study, publication type, type of treatment), population characteristics (number of patients, number of aneurysms, follow-up length, symptoms, and timing of treatment), baseline demographics (age, gender), early and late-related complications, and reinterventions. Non-deducible data were labeled as “not reported” or “non extractable,” as appropriate.
The main outcomes were postoperative complications, reinterventions and mortality.
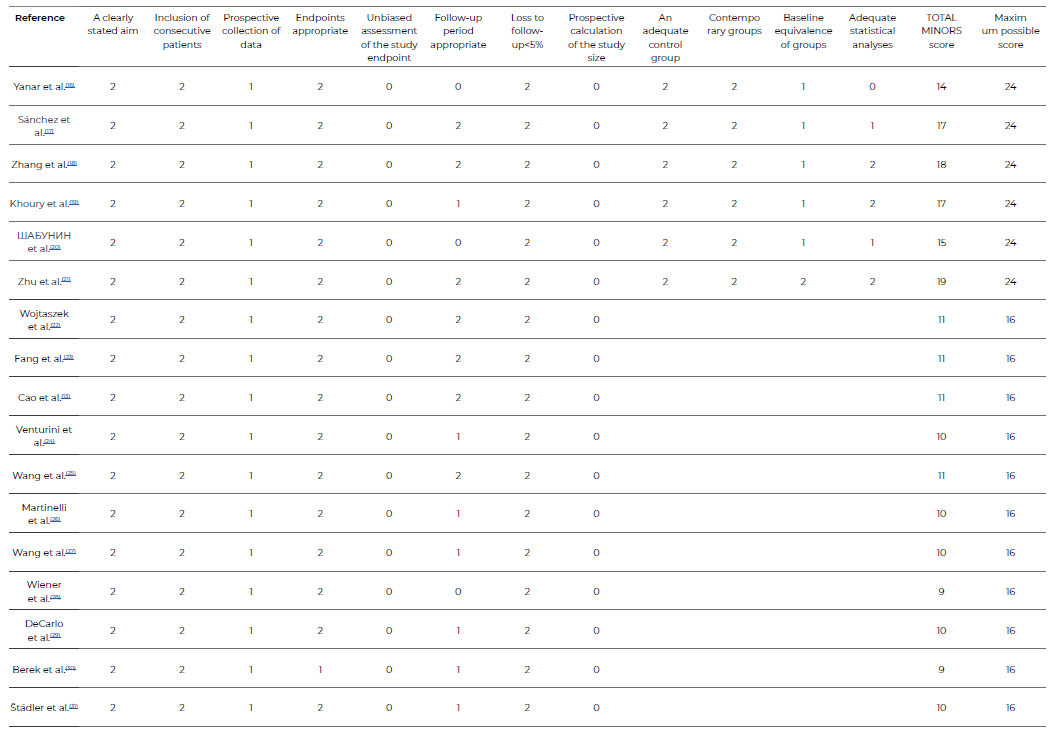
Quality assessment
The methodology of the studies and risk of bias were systematically assessed by two independent reviewers (AC and MM) using the Methodological Index for Non-Randomized Studies (MINORS) score,15 with a maximum score of 16 for non-comparative and 24 for comparative studies. A score ≤8 was considered poor quality, 9-14 moderate quality, and 15-16 good quality for non-comparative studies. For comparative studies, the cut-off points were ≤14, 15-22, and 23-24.
Authorship of the studies was unblinded during the review. Discrepancies between the reviewers during the search, selection, and quality assessment were resolved by discussion. In case of persisting disagreement, a third reviewer was consulted.
Statistical analysis
The case reports and small series with individual patient data were grouped and analysed with the Statistical Package for the Social Sciences (SPSS, version 25.0 for windows / MacOS) program. The software Medcalculate and Stats to do were used to perform pooled analysis. Continuous variables were expressed through the mean and standard deviation, and the categorical variables were described by percentage, with a 95 % confidence interval.
Most studies (58) were case reports or small case series with individual patient data (12), 14 were unicentric case series, one was multicentric and one was based on national data. Six were comparative studies; seven only included ET patients, and four only included OS patients, Table 1.
Regarding quality assessments, in comparative studies five were of moderate quality and one of poor quality, and all non-comparative were of moderate quality, Table 2.
Results
A total of 1061 patients were included, corresponding to 1085 reported SAAs. Of these, 317 (29.9%) were submitted to OS and 744 (70.1%) to ET, Table 1.
The mean age was 51.62 +- 14.57, with older patients in the OS group (54.49±15.95 vs 51.92±12.83) and 39.8% (29.5-50.0) were male (OS 34.5% [16.2-52.8] vs ET 41.7% [27.0-56.3]). A total of 12.6% (0.3-24.9) were detected during pregnancy, with a higher frequency of pregnancy also in the OS group (29.5% [0.0-9.3] vs 7.2% [0-14.6%]), Table 3.
The mean diameter was 3.18 +- 2.07 cm (OS 4.95±3.74 vs ET 3.10±1.92). Most SAA were located on the distal third of the splenic artery (165/376, 43.89%; ET 94/243, 38.68% vs OS 11/20, 55%), Table 3.
The frequency of rupture was 2.8% (0.0-8.9%) and much higher in the OS group (OS 37.5% [0-100%] vs ET 6.5% [0.0-23.4]), Table 3.
In the majority of the patients, the diagnosis was performed with CTA (206/328; 62.80%), followed by DUS combined with CTA (83/328, 25.30%). Less frequently, the diagnosis was performed with laparotomy combined with DUS (31/328, 9.45%), MRI combined with DUS (5/328, 1.52%), laparotomy combined with DUS (2/328, 0.61%) or only DUS (1/328, 0.30%).
Regarding treatment, the types of intervention reported were ET (744 patients) and OS (317 patients: 281 conventional open reconstructions, 25 laparoscopic, and 11 robotic).
Overall, 744 patients underwent endovascular repair. Most endovascular treatments were transarterial embolization (261/328), mainly with metallic coils or microcoils. Covered stents were used in 35/328 patients and embolization and stent in 29, Table 4.
The most performed conventional open reconstruction procedure was aneurismectomy (28/60). Overall, three patients received OS with ligation; eight aneurismectomy and reconstruction (seven end-to-end anastomosis and one bypass), and 11 primary splenectomies were performed. Also, 6/25 (24%) were submitted to laparoscopic splenectomy and aneurysmectomy, 18 (72%) laparoscopic clipping, and one (4%) to laparoscopic resection. Only one study included robotic surgery, in which 11 (100%) patients were submitted to aneurysm clipping and reconstruction, Table 4.
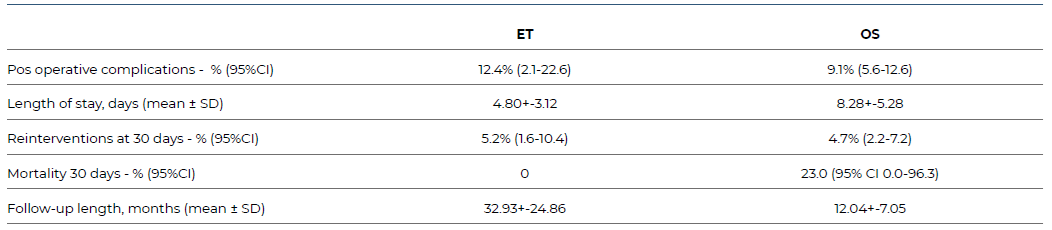
Post-operative complication rates were 12.4% (2.1-22.6) in the ER group and 9.1% (5.6-12.6) in the OS. In the ET group, the most frequent post-operative complications were postembolization syndrome and splenic infarction. In the OS group, the majority were systemic (sepsis and myocardial infarctions). In the robotic surgery group, there were two open conversions due to flat adhesions in the abdominal cavity, Table 5.
Splenectomy was performed in 3.52% in the ET and 8.61% in the OS group. The mean hospital stay was 4.80+-3.12 in ET and 8.28+-5.28 after OR.
The reintervention rate at 30 days was 5.2% (1.6-10.4) in the ET group. The main cause was SAA repermeabilization, which was treated with endovascular re-embolization. The leading cause for open conversion was failure to catheterize the splenic artery selectively. Reintervention after OS was 4.7% (2.2-7.2), Table 5.
Overall, there were three deaths, all in the OS group (mortality: 23.0 (95% CI 0.0-96.3).
The follow-up length in months was 32.93+-24.86 in ER and 12.04+-7.05 in OS group, Table 5.
Table 1 Characteristics of articles reporting on patients treated for splenic artery aneurysm, from January 2019 to January 2024, included in the systematic review
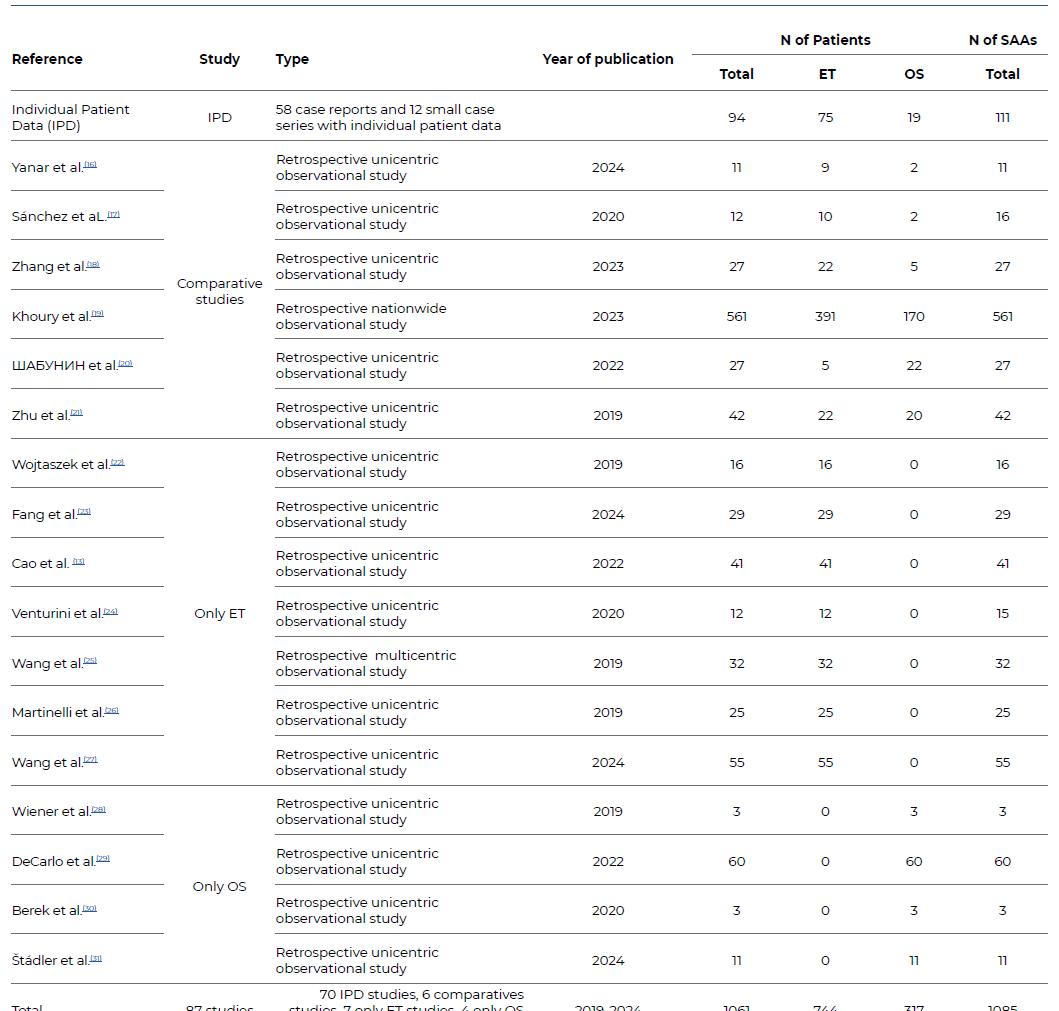
IPD - Individual Patient Data; ET - Endovascular Treatment; OS - Open Surgery; SAA - Splenic Artery Aneurysm
Table 3 Summary of the characteristics of patients and splenic artery aneurysms, included in the systematic review
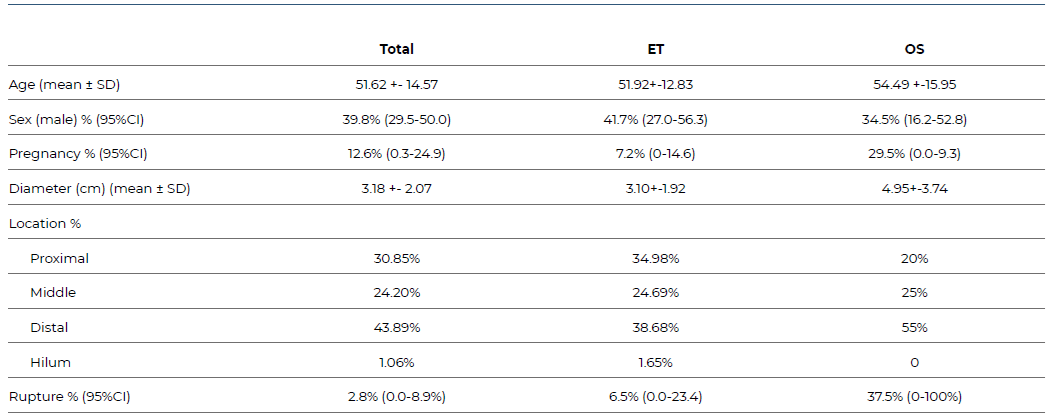
SD - Standard Deviation; CI - Confidence Interval; ET - Endovascular Treatment; OS - Open Surgery
Table 4 Summary of treatment techniques applied to patients with splenic artery aneurysm, included in the systematic review.
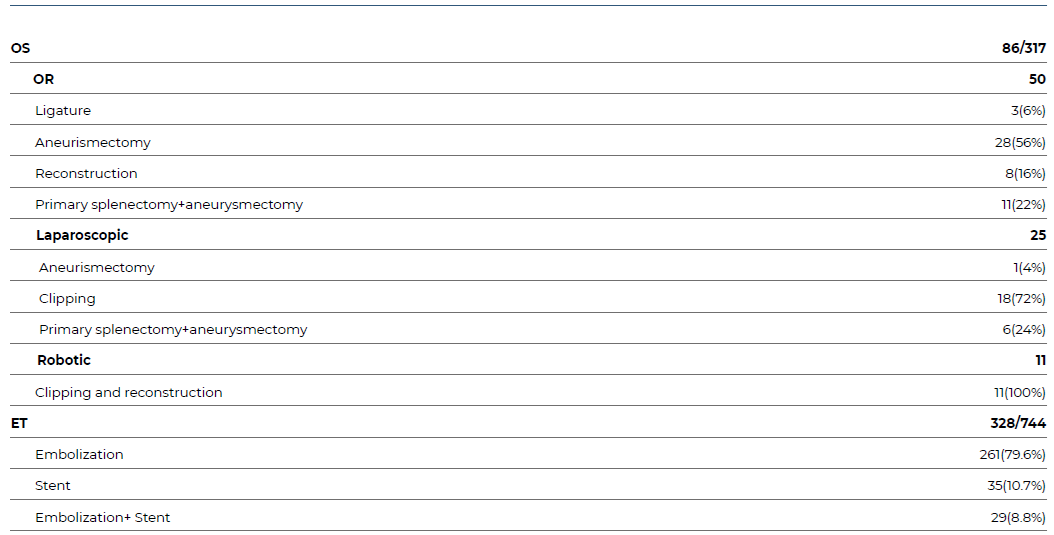
ET - Endovascular Treatment; OS - Open Surgery; OR - Open reconstruction
Post-operative complication rates were 12.4% (2.1-22.6) in the ER group and 9.1% (5.6-12.6) in the OS. In the ET group, the most frequent post-operative complications were postembolization syndrome and splenic infarction. In the OS group, the majority were systemic (sepsis and myocardial infarctions). In the robotic surgery group, there were two open conversions due to flat adhesions in the abdominal cavity, Table 5.
Splenectomy was performed in 3.52% in the ET and 8.61% in the OS group. The mean hospital stay was 4.80+-3.12 in ET and 8.28+-5.28 after OR.
The reintervention rate at 30 days was 5.2% (1.6-10.4) in the ET group. The main cause was SAA repermeabilization, which was treated with endovascular re-embolization. The leading cause for open conversion was failure to catheterize the splenic artery selectively. Reintervention after OS was 4.7% (2.2-7.2), Table 5.
Overall, there were three deaths, all in the OS group (mortality: 23.0 (95% CI 0.0-96.3).
The follow-up length in months was 32.93+-24.86 in ER and 12.04+-7.05 in OS group, Table 5.
Discussion
Regarding patients´ demographic characteristics, the results of our systematic review are in accordance with previously published literature, as SAAs appear more in medium age women (51.62 +- 14.57 years old, 60.2 % women).1,2,3 The gold standard for diagnosis is CTA (62.80% in our review).6
According to the SVS clinical practice guidelines on the management of visceral aneurysms, indications for SAA´s treatment are non-ruptured splenic artery pseudoaneurysms of any size in patients of acceptable risk because of the possibility of rupture (Grade 1, Quality of Evidence: B), non-ruptured splenic artery true aneurysms of any size in women of childbearing age (Grade 1, Quality of Evidence: B) and non-ruptured splenic artery true aneurysms >3 cm, with a demonstrable increase in size, or with associated symptoms in patients of acceptable risk because of the risk of rupture. (Grade 1, Quality of Evidence: C).6
The management of SAAs typically involves either open surgical or endovascular methods. However, the choice between the two approaches should be made meticulously, considering the specific anatomy of the aneurysm, any related patient clinical conditions, and the individual's overall health status.
Overall, according to our review, OS demonstrated lower morbidity and reintervention rates compared to ET, albeit with higher mortality rates. It's important to note that patients who underwent OS were notably older, more likely to be pregnant, and to have ruptured SAAs. These factors could contribute to the observed higher mortality in the OS group. In cases not involving pregnancy, SAAs have a relatively low rupture rate of less than 2%. However, the overall mortality rate of ruptured SAAs can be as high as 25%, which aligns with the 23% mortality rate found in our review.(16-32 SAAs in young women, particularly during the third trimester of pregnancy, are known to have a heightened risk of rupture.33 Pregnancy may be associated with 20% to 50% of all SAA ruptures, with devastating maternal and fetal mortality rates reaching 80% and 90%, respectively.34
According with SVS guidelines, the conventional surgical approach for managing SAAs involves proximal and distal ligation combined with aneurysmectomy, particularly for lesions located in the proximal or middle segments of the splenic artery. Typically, revascularization of the distal splenic artery isn't necessary due to maintained collateral flow through the short gastric arteries. ET offers immediate benefits such as local anesthesia, shorter hospital stays, and quicker recovery. However, drawbacks include the risk of end-organ embolization and a relatively higher failure rate than OS. Patients undergoing ET, particularly those with splenic artery occlusion for SAAs, may develop postembolization syndrome characterized by persistent pain, fevers, and systemic symptoms. Some experts argue that patients with aneurysmal disease at the splenic hilum might be better served by open repair and splenectomy.6
The main limitation of this systematic review is the quality of the original data, mostly small case series, and the heterogeneity of the reports.
Conclusion
SAAs rupture is associated with high mortality, so timely diagnosis and management are essential to attain a satisfactory outcome. A detailed and individualized analysis of each case and a sufficient understanding of the anatomy and hemodynamics of a particular aneurysm should guide the therapeutic decision.
OS has good results in the treatment of SAA with lower morbidity and reintervention than ET. However, ET should be a viable alternative in high-risk patients with favorable anatomy.
It would be important to create national registries with lifelong follow-up and randomized multicentric studies with a higher caseload to compare the outcomes of different treatments of SAA. Based on this, it would be easier to synthesize a guideline for managing SAA.