Background
Extremity-related vascular trauma is quite rare.1,2 A solitary femoral vascular injury is exceedingly uncommon when it does not coexist with significant musculoskeletal trauma, such as fractures, dislocations, contusions, crush injuries, or traction. However, superficial femoral artery (SFA) trauma is uncommon. It can lead to significant morbidity and mortality if not promptly diagnosed and managed, especially if associated with superficial femoral vein (SFV) injury. 1,2
Case report
A 60-year-old man with no known co-morbidities was transferred by air ambulance following a high-impact trauma with a freight elevator while working on his farm. The patient reported that he had been hit and pulled up by the machine, falling to the ground from a height.
At the emergency department, he was hemodynamically unstable, with a blood pressure of 77/30mmHg, and presented with a large wound of the proximal third of his right thigh, associated with active bleeding and swelling of the distal limb. His right foot was pale and cold compared with the left, and no tibial artery pulses were present. Motility and sensitivity could not be evaluated due to the patient’s hemorrhagic shock.
Laboratory tests revealed a low haemoglobin of 7.2 g/dL, platelets of 50,000/ μL, white blood cells of 14,9 × 106 / μL, and lactate of 3.6 mmol/L. The Mangled Extremity Severity Score (MESS) score was 7, establishing a poor prognosis for the affected limb.3 However, we decided collectively to proceed with autologous vein reconstruction.
Considering the emergency, the patient was immediately transferred to the operating room. Surgical exposure revealed an approximately 20-cm-wide total resection of muscle and subcutaneous tissue in the thigh area. The SFA was severed (Figure 1) and presented severe atheroma with multiple and irregular calcifications. Additionally, the SFV’s anterior wall was disrupted and associated with local thrombosis. The injured SFA segment (4-5 cm) was resected, the third proximal segment of the right great saphenous vein (GSV) was isolated and prepared, and a GSV to SFA interposition bypass was performed (Figure 2). The SFV was ligated.
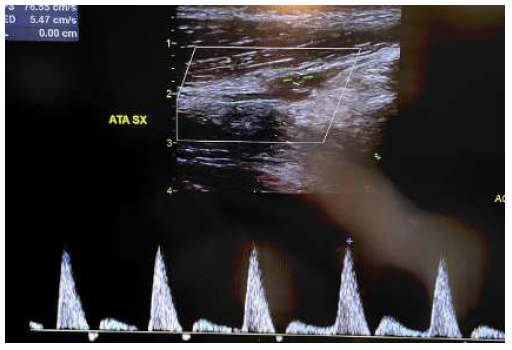
During the intervention, the patient experienced three cardiac arrests, and 15 bags of red blood cells were transfused. Immediately after the operation, the foot was warm, assuming normal colouration and pulsation at the ankle was detected. The presence of compartment syndrome was excluded. A duplex ultrasound performed shortly after the procedure showed direct blood flow to the tibial arteries, Figures 3 and 4.
The patient was maintained on systemic heparin infusion following surgery and spent five days in the intensive care unit. No further cardiac events occurred during this period. No neurological deficits or compartment syndrome were noted. A brain computed tomography was negative for acute or sub-acute haemorrhage or other sequelae from reanimation.
Ten days after the procedure, full-dose anticoagulation was suspended, and rivaroxaban (2.5 mg twice daily) and aspirin (100 mg) were started. Contributing to this antithrombotic regimen were the presence of peripheral artery disease along the ligation of the SFV, great saphenous vein bypass, and the lack of symptoms and indicators referred to as compartment syndrome, muscle haemorrhage, or surgical wound bleeding. Three weeks after admission, the patient was discharged with no complaints or complications. The dual pathway antithrombotic regimen was maintained for six months, after which the patient was given aspirin only.

Figure 1 Intraoperative image of the surgical exposure prior to revascularization. The superficial femoral artery and vein are visualised, exhibiting traumatic injuries.
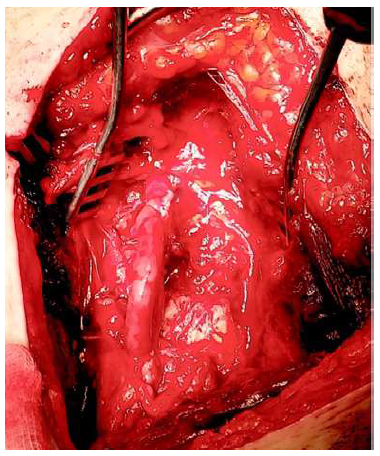
Figure 2 Intraoperative image after revascularization. An interposition graft using reversed great saphenous vein can be observed.
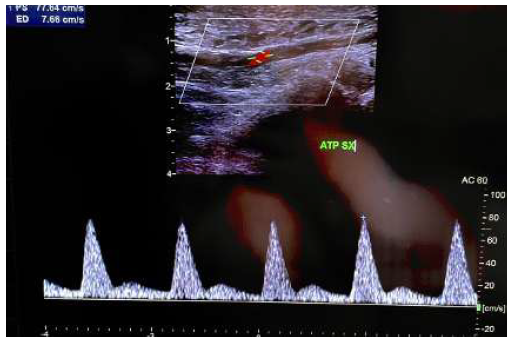
Figure 3 Post operative duplex ultrasound (1). Direct flow can be observed a the level of the distal posterior tibial artery.
Discussion
Penetration and blunt trauma account for 85% and 15% of femoral artery injuries, respectively.4,5 Up to 70% of peripheral vascular injuries in civilian trauma cases involve femoral vessels.5 The total incidence of injuries to the femoral artery is 18.8%,6 while the incidences of brachial, axillary, popliteal, and subclavian artery trauma are 48.2%, 15.3%, and 5.9%, respectively.7-10 The incidence of femoral artery injuries amongst all vascular trauma represents 26%.5 Major veins and nerves can also be damaged, and these conditions are typically associated with other lesions, such as organ lesions, fractures, and dislocations.11,12 In the absence of concurrent lesions, arterial injuries may be frequently misdiagnosed.2,4
Blunt trauma injuries are frequent among militaries due to high-velocity gunshot wounds. Among civilians, particularly in Western countries, deep wounds from high-energy blunts during work are not uncommon.6 According to some authors, blunt vascular trauma may result from the transfer of shearing forces that cause an intima flap and ultimately cause thrombosis,4,5 The possibility of vascular lesions should be evaluated for those who are injured by blunt trauma to the inferior limb area even though they do not show any specific symptoms associated with vascular injury and skin integrity is reported. Therefore, signs of arterial injury like pulse deficit, swelling, active bleeding, and poikilothermia, despite an externally intact vessel, might suggest an intima tear and arterial occlusion, which warrants appropriate management.13-15
The Mangled Extremity Severity Score (MESS) is recommended to guide limb salvage decision-making.3
Arteriography and duplex ultrasound may help evaluate a patient with suspected vascular damage to the limbs. Nowadays, the most accepted indications for arteriography in patients with lower extremity injuries are abnormal ankle-brachial indices (ABI), multiple injuries (gunshot wounds, comminuted fractures), blunt trauma with signs of vascular injury, extensive orthopaedic injuries or soft tissue defects, and in hemodynamically stable patients.16
The type and size of the injury will determine the vascular repair technique.17 If either the proximal or distal vascular segment can be mobilised and the traumatised segment involves up to 2 cm of length, resection with a primary anastomosis may be feasible. If too much tension is exerted on the anastomosis, an interposition graft becomes necessary.17 There is a discussion on the best arterial graft for revascularization. However, that discussion is outside the scope of this paper. Patients who are in shock, hypothermic, coagulopathic, or who have received significant volumes of blood are typically treated with PTFE grafts to expedite revascularization and reduce operative time.6 Nonetheless, research suggests no differences in results and complications between autogenous and synthetic grafts.17,18
According to a study by Cargile et al.12 including 321 patients with femoral vascular injuries, 36% experienced damage to both femoral artery and vein, 15% to isolated veins, and 48% to isolated arteries. Eighteen repaired veins thrombosed, eight of 61 simple (lateral venography), and ten of 50 complex repairs. Thirty-four per cent of patients with a venous injury repair had clinical evidence of postoperative deep vein thrombosis or oedema, and six patients (2.5%) had a documented pulmonary embolism. Cargile's review demonstrates that thrombotic and embolic problems may arise with vein reconstruction.
The four amputees in the series by Degiannis et al. all had an ischaemia period greater than five hours.13 Comparable to previous studies, the amputation rate was 4.9% for Hafez et al. and 3% for Asensio et al.6,14 However, amputations can be a reasonable option to save a patient's life over a limb in the following situations: a deeply ischemic limb at the time of presentation; a mangled limb with no reconstructive solutions, or a shocked patient with uncontrollable bleeding. In these studies, patients who presented hemodynamically unstable did not have an increased risk for limb loss. The risk of graft infection, especially with extensive tissue destruction, has guided the decision to use native vein graft.
Rayamajhi et al. reported in their experience of 158 patients with femoral artery injuries, in which half (51%) of the surgical repairs were done primarily, vein graft was utilised in 33%, and a prosthetic graft (PTFE) in 10%.15 Femoral vein injuries are managed primarily with ligation (85%). Of these, four had some residual minor limb oedema in the early period (6%), and 70% of the secondary amputations presented a concomitant ligation of the femoral vein. They performed 131 venous repairs; 50 were reconstructed by terminus-terminal bypass and 69 using terminus-lateral bypass. Thirteen vein repairs (14%) were thrombosed at presentation. Pulmonary embolism occurred in four of the patients. Thirty-four per cent experienced limb oedema or deep venous thrombosis. It is well known that femoral artery penetration and blunt trauma can be repaired with GSV grafts. Ipsilateral superficial and deep venous trauma is a risk factor for lower extremity vascular injury, which is why the contralateral GSV is typically used.
Shaik et al. reported their experience of 76 patients who underwent autologous GSV bypass for lower extremity vascular injuries.19 Of these, 15 patients (20%) underwent repair with ipsilateral-GSV bypass. Using a propensity-matched analysis, they found no significant difference in 1-year major amputation (8.3% vs. 4.8%, P = 0.99). Kaplan-Meier analysis of bypass grafts showed comparable primary patency rates for ipsilateral or contralateral GSV bypasses at one year (84% vs 91%) and three years post-intervention (83% vs 90%, p = 0.364) and concluded that in lower extremity artery trauma cases when contralateral GSV use is not practical, ipsilateral GSV may be utilised as a durable conduit for bypass. Reasonable criteria for the use of ipsilateral GSV use involved trauma to the contralateral leg (26.7%), relative accessibility (33.3%), and other reasons (40%).19
Ramdass et al. reported their experience of 14 patients with SFV trauma due to vascular trauma, of which 11 underwent SFV ligation and 3 surgical repairs with PTFE.20 They also observed limb salvage rate in the SFV ligation group was 73% (8/11) at 1 year with three significant amputations above the knee in the first week; no long-term prolonged swelling, pain, neurologic deficit, phlegmasia, or venous gangrene in the eight limb salvage patients were detected. In the study by Manley et al., including 84 patients with deep venous injuries, 48 underwent vein repair and 35 vein ligation.21 Those who underwent vein ligation had a greater degree of shock on presentation (red blood cell unit transfusions, 14 vs eight units; p = 0.03) and were more likely to receive prophylactic fasciotomies (60% vs 33%, p = 0.01); finally, patients with vein ligation had a lower rate of pulmonary embolism or deep venous thrombosis (9% vs 31%, p = 0.02) with no difference in symptomatic lower-extremity oedema (37% vs 39%, p = 0.88) or amputation rates (0% vs 2%, p = 0.99).
However, the nature and severity of the injury, accompanying lesion, and comorbidities substantially impact the postoperative outcome for patients with lower extremity injury.3 For high-risk patients (crush injury, concomitant venous injuries, prolonged ischemia, and extensive bone fractures), a prophylactic fasciotomy is justified. Karonen et al. reported their experience of 76 patients with acute limb ischemia treated with either prophylactic or therapeutic fasciotomy.16 There is no significant difference between the two groups regarding acute kidney insufficiency or neurological lesions. At the same time, wound complications were higher in the therapeutic fasciotomy group, suggesting, above all, that a more conservative approach could avoid unnecessary fasciotomies and reduce wound complications.
Conclusion
We have presented an unusual case of combined superficial femoral artery and vein injury as a result of forceful trauma, with a successfully preserved patient's lower limb, good neurological outcome, and no major complications. Vascular trauma should be thoroughly excluded and expeditiously managed if present, despite skin integrity.
A rapid clinical and surgical evaluation should be performed to prevent possible severe complications related to prolonged ischemia, not only for the vitality of the limb but also to preserve the patient’s life.