Introduction
Arterio-ureteral fistulas (AUFs) are a rare (incidence between 0.04-0.06%) but potentially life-threatening condition with reported mortality rates of 7-23%.1 They are classified as primary, secondary/iatrogenic or pregnancy related. While most fistulas are secondary to ureteral manipulation and cancer, primary AUFs occur due to erosion associated with aortoiliac aneurysmal disease or pseudoaneurysm. Historically, AUF were also associated with pregnancy, but the pathophysiology of these cases was related to chronic ureteropelvic obstruction secondary to severe pyelonephritis before the advent of antibiotics and have now become obsolete.2
Secondary AUF are more commonly associated with pelvic exenteration, radiation therapy, infection, vascular reconstructive surgery and indwelling ureteral catheters or stents.3 Diagnosis requires a high level of suspicion in the presence of the aforementined risk factors since symptoms like hematuria and back pain are nonspecific.
The authors present a case of a patient who developed an AUF 4 months after pelvic exenteration, lymphadenectomy and cutaneous ureteroileostomy.
Case report
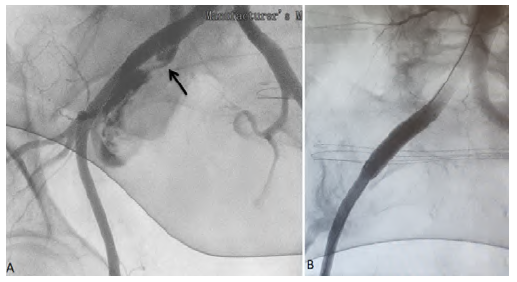
A 84-year-old female, with history of lupus, underwent pelvic exenteration, lymphadenectomy and cutaneous ureteroileostomy for high-grade urothelial carcinoma. In the postoperative period, an ileostomy with reconstruction of ureteroileal anastomoses and bilateral nephrostomies was required due to intestinal dehiscence with an abscess. She completed broad-spectrum antibiotics and antifungal therapy and was discharged with catheterized ureters. About 4 months later, the patient presented to the emergency department (ED) with gross hematuria. The blood work revealed 11g/dl of haemoglobin. Having been discharged, she returned to the ED the next day, hypotensive (94/61mmHg) with significant hematuria from ureteroileostomy, while haemoglobin had dropped to 8 g/dl, requiring aminergic support and the transfusion of two units of blood. Computed tomography (CT) angiography did not identify active bleeding and suggested integrity of the excretory system. She remained hospitalized under surveillance until she had another episode of hemorrhagic shock (blood pressure 49/23mmHg) with profuse bleeding through the ureteroileostomy, with a drop of hemoglobin to 5.5 g/dl. A new CT angiography was performed identified a fistula between the right common iliac artery and the ureteroileostomy (Figures 1 and 2). She underwent emergency angiography and fistula exclusion with a covered stent with intentional hypogastric coverage (the contralateral hypogastric was patent) given the short sealing length and the imminent risk of death (Figure 3). During the remaining hospital stay, there were no bleeding recurrences, and the patient was discharged on the 21st postoperative day after completing antibiotic therapy (meropenem and linezolid) and antifungal medication (micafungin) directed to urine cultures (isolated: multidrug resistant Staphylococcus aureus, Enterococcus faecium, Candida albicans). About one month later she was hospitalized again for acute kidney injury with ionic changes and complicated urinary tract infection, ending up dying from this complication.

Figure 1 Preoperative computed tomography angiography (cross sectional). Right common iliac artery-ureter fistula on cross sectional computed tomography angiography (black arrow)

Figure 2 Preoperative computed tomography angiography (sagittal). AUF on sagittal computed tomography angiography (black arrow). Red arrow points to the ureteroileostomy with contrast inside.
Discussion
The first case of an AUF was described in 1908, between external iliac artery and ureter after a bilateral ureterostomy.4 Since the development of ureteral stents in 1978, the number of reported AUFs has increased, which could be related to the increased frequency and duration of ureteral stent placement. In contrast, the mortality rate decreased from 69% in 1980 to 7-23%, probably due to the lower threshold of suspicion of the disease and the greater availability of less invasive solutions.5
Pathophysiologically, it is considered that previous radiation therapy and pelvic or vascular surgical procedures may affect the integrity of the vasa vasorum leading to a weakening of the adventitia and media of the arteries, increasing their susceptibility to rupture and necrosis. The ureter can also become fixed and obstructed by the surrounding inflammatory process leading to fibrosis and less compliant ureter.6 Then, the mechanical trauma produced by the repeated pulsation of either a native artery or graft over a weakened ureter with a rigid catheter/stent inside it, may trigger the fistula.2
Diagnosis can be difficult if this pathology is not suspected. Patients may present with significant hematuria and hemorrhagic shock, but more frequently report intermittent hematuria and back pain. This occurs due to blood clot formation within the urinary tract with consecutive obstruction and ureteral distention.1 Bleeding may be provoked on stent manipulation or stent exchanges. A systematic review described that the mean time for the first clinical manifestation - hematuria - in secondary fistulas was of 2 years for the patients with malignant disease and 10 years for the patient with previous vascular surgery.7
To aid in the diagnosis, CT angiography is usually performed, however the results are often negative and indirect findings such as hydronephrosis or blood clot formation within the urinary tract are the common form of diagnosis.1 Cystoscopy can identify pulsatile bleeding from the ureteral orifices so the placement of a balloon catheter in the ureter might temporarily stop the bleeding. Retrograde ureterography may demonstrate extravasation of contrast into the artery however is frequently limited or even impossible due to the massive bleeding.1 Angiography is useful to identify the ureteral bleeding and, if it is not identified, could be provoked through manipulation of the ureteral catheter.
AUF can be managed by conventional or endovascular surgery. Surgical intervention is challenging because of the presence of adhesions and often are not feasible, but may include nephroureterectomy, local reconstruction techniques, arterial ligation, bypass grafting or, less commonly, auto-transplantation.3 Iliac artery embolization may be an option however it requires additional extraanatomical bypass surgery to maintain lower limb perfusion.3 Percutaneous endovascular exclusion with stent graft appears to be an effective and safe therapeutic choice, although recurrence of hematuria, infection or stent thrombosis have been described.1 There is no consensus on whether or not the ureteral side needs to be treated after endovascular stent graft deployment. Treatment may include percutaneous transrenal ureteral embolisation.1
In the case described, although the patient did not undergo radiotherapy or chemotherapy, probably the corticosteroid therapy for lupus associated with the permanent catheterization of the ureters favored the development of an AUF. We opted not to treat the ureteral side due to continued urine diversion through nephrostomy catheters. No follow-up abdominal CT images were performed when the patient was hospitalized again 1 month later, therefore, infection of the stent graft cannot be excluded.
To conclude, AUF is a rare life-threatening condition that requires a high degree of suspicion for diagnosis. Percutaneous stent graft placement appears to be an effective and safe therapeutic choice.