Introduction
Endoleaks are among the primary complications following endovascular aneurysm repair (EVAR), which is present in up to one-third of cases. Among these, type 2 endoleaks (T2EL) account for the most common type of endoleak, comprising over half of all cases, with a prevalence of 20 to 40% in different series after EVAR.1-3
T2EL occur as a result of retrograde flow into the aneurysmatic sac through patent branch vessels, such as lumbar arteries (LA) and the inferior mesenteric artery (IMA), with less common sources being the median sacral artery and accessory renal arteries, thereby preventing complete exclusion of the aneurysm from systemic pressure, which can in turn lead to progressive sac growth and ultimately aneurysm rupture.2 Despite this, most T2EL are benign with an estimated rupture rate <1%.1
Multiple strategies with high technical success rate for treating T2EL have been described, yet robust data regarding the benefits of embolization are lacking, since continuous aneurysm growth, development of new T2EL and risk of rupture can persist after successful embolizations.1,4
While current guidelines advocate a strategy of vigilant surveillance and conservative management for most T2EL cases, recent attention has turned towards prophylactic measures aimed at preventing their occurrence.1 Due to lack of robust evidence, pre-emptive embolization of LA and IMA are not recommended, being reserved for selective cases.1
We aimed to investigate the impact of LA and IMA diameter and patency, as well as other associated risk factors on the development of T2EL after EVAR.
Methods
Study Population and Inclusion Criteria
We conducted a retrospective analysis of patients who underwent elective endovascular aneurysm repair for infrarenal aortic aneurysms at our institution between January 2020 and December 2022. Patients were included if they had undergone EVAR without embolization of LA or IMA, with both preoperative and postoperative imaging available for analysis. Exclusion criteria comprised patients who underwent EVAR for ruptured aortic aneurysms or other urgent/emergent indications, patients treated with complex endovascular procedures (e.g., f/bEVAR, chEVAR, iliac branch devices), and patients with incomplete or unavailable imaging data.
Data Collection
Patient demographics, including age and gender, were extracted from electronic medical records. Aneurysm characteristics, including diameter and morphology, were assessed based on preoperative computed tomography angiography (CTA) scans. All patients underwent preoperative CTA to evaluate the anatomy of the abdominal aorta and its branches. Postoperative CTA was performed one month after EVAR to confirm technical success and detect any immediate complications. Follow-up imaging at 12 months was conducted using either duplex ultrasound or CTA to assess long-term outcomes, including persistent endoleaks and aneurysm sac changes.
Follow-Up Strategy
Patients were followed through routine postoperative surveillance. Early T2EL were defined as those detected at the one-month CTA, while late T2EL were those identified after one-month of the procedure. If an endoleak was identified, its persistence or resolution was monitored in subsequent imaging studies. Aneurysm sac changes were recorded, and cases requiring reintervention were noted. Two authors reviewed pre- and postoperative CTA images independently using Sectra Uniview software (Sectra AB, Linköping, Sweden) to evaluate the patency and diameter of both lumbar and inferior mesenteric arteries.
Definitions
T2EL was defined as the presence of contrast within the aneurysmal sac attributed to one or more patent branch vessels, without other visible causes such as type 1 or 3 endoleaks. Collateral patency was assessed based on continuous contrast enhancement within these vessels from the aorta on preoperative CTA. The diameter of LA and IMA was measured at their origins. Total number of covered LA was defined as the number of LA covered during EVAR, despite their preoperative patency (patent and non-patent LA). In contrast, patent LA refers only to covered LA that were patent during the preoperative CTA. Total LA diameter refers to the sum of diameters of all patent LA on preoperative CTA, while total combined diameter corresponds to the sum of total LA diameters and IMA diameter. Aneurysm sac growth or shrinkage was defined as a ≥ 5mm change from the preoperative scan.
Endpoints
The primary outcome was defined as presence of a T2EL following EVAR. Secondary outcomes included aneurysm sac growth or shrinkage at 12-month follow-up, the need for reintervention, and any association between LA and IMA characteristics and the occurrence of T2EL.
Statistical Analysis
Descriptive statistics were used to summarize patient characteristics. Continuous variables were expressed as mean ± standard deviation or median with interquartile ranges, depending on data distribution, while categorical variables were presented as frequencies and percentages. The normality of continuous variables was assessed using the Shapiro-Wilk test.
Comparisons between groups were performed using Student’s t-test or the Mann-Whitney U test for continuous variables, and the chi-square test or Fisher’s exact test for categorical data, as appropriate. A p-value of < 0.05 was considered statistically significant. All statistical analyses were performed using Microsoft Excel version 2019 (Microsoft Corp, Redmond, Washington, USA).
Results
Population Characteristics
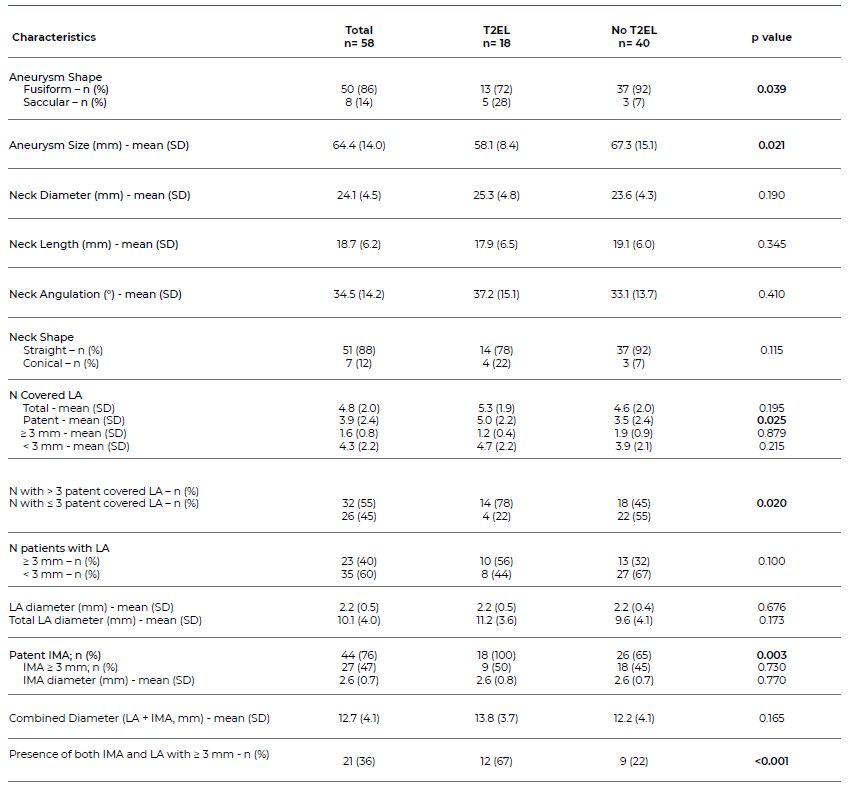
A total of 58 patients were included in our study cohort, 18 (31%) with T2EL and 40 (69%) without T2EL. The majority were male (n=56; 97%), with a median age of 75 (range: 59 to 86). The most common cardiovascular risk factors included hypertension (89.7%), dyslipidaemia (71%) and smoking history (76%), with 31% of diabetic patients included in the cohort. Antihypertensive (84%), statins (78%) and antiplatelet (83%) were among the most common drug classes used by patients, with 43 (74%) under single antiplatelet therapy and 5 (9%) under dual antiplatelet therapy. Six patients (10%) took anticoagulants, the most common indication being atrial fibrillation. Population characteristics are summarized in Table 1.
Most patients had fusiform aneurysms (86%), with only 8 patients (14%) treated for saccular aneurysms. Mean aneurysm size at the time of treatment was 64.4±14.0mm, with a mean neck diameter and length of 24.1±4.5mm and 18.7±6.2mm, respectively. Most aneurysms had a parallel neck (88%), with only seven patients (12%) presenting with conical necks.
Regarding LA, mean number of total covered arteries was 4.8±2.0 and mean number of patent covered arteries was 3.9±2.4, with 55% (n= 32) of patients having more than three LA covered after EVAR. All patients had at least one lumbar artery with ≤ 2mm, with only 23 patients presenting LA with ≥ 3mm. Mean lumbar artery diameter was 2.2±0.5mm and mean total LA diameter was 10.1±4.0mm.
Mean IMA diameter was 2.6±0.7mm, with 27 (47%) patients presenting with an IMA ≥ 3mm. Forty-four (76%) patients had a patent IMA at its origin. Mean total combined diameter was 12.7±4.1mm.
Aneurysm shape, sac and neck characteristics, as well as collateral patency, size and number are summarized in Table 2.
Table 1 Baseline characteristics of EVAR patients included in the study, stratified by the presence or absence of type 2 endoleak
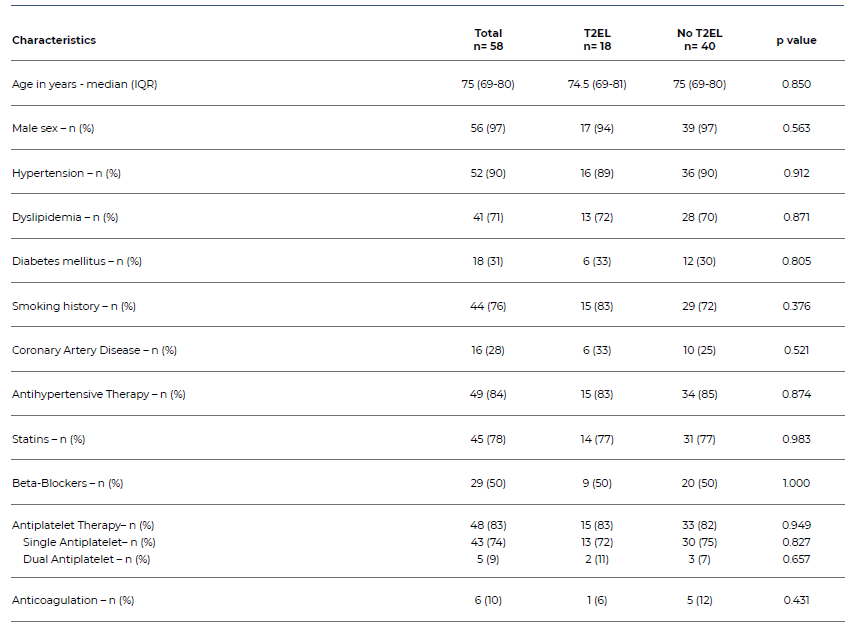
T2EL - Type 2 endoleak; IQR - Interquartile range
Analysis on T2EL
Among the 58 included patients, 18 (31%) developed a T2EL on follow-up, of which 16 (88.9%) early T2EL (detected at one-month CTA) and two (11%) late T2EL (detected at 12-month follow-up). One patient had a type 3 endoleak.
T2EL was present in 17 (30%) males and one (50%) female. Median age was not different between patients with and without T2EL (74.5 and 75 years, respectively; p=0.85). Cardiovascular risk factors and medication therapy were similar between the two groups.
We noticed a statistically significant association between aneurysm shape and development of T2EL (p= 0.039). Notably, 5 (62%) treated saccular aneurysms developed T2EL, whereas only 13 (26%) treated fusiform aneurysms were associated with endoleak. Aneurysm size was smaller in the group with T2EL (58.1±8.4mm vs. 67.3±15.1mm without endoleak, p= 0.021). Aneurysm neck characteristics were similar, although patients with T2EL had slightly wider, shorter and more angulated necks when compared to patients without T2EL (25.3±4.8mm vs. 23.6±4.3mm, p=0.190; 17.9±6.5mm vs. 19.1±6.0mm, p=0.345; 37.2±15.1° vs. 33.1 ± 13.7°, p=0.410). Regarding neck shape, patients with T2EL had more commonly conical necks, although this was non-significant (22% vs. 7%, p=0.115).
Overall number of covered lumbar arteries and patent covered arteries were superior in the group with T2EL (5.3±1.9 and 5.0±2.2 vs. 4.6±2.0 and 3.5±2.4 without T2EL, respectively), with only patent covered LA achieving significance for developing T2EL (p=0.025). Similarly, there was a statistically significant association between covering more than three lumbar arteries and T2EL (p=0.02; 78% T2EL vs. 45% without T2EL), while covering a LA with ≥ 3mm, despite being more frequent in the T2EL group (56% vs. 32% without) was not significantly associated with this complication.
Analysis on IMA showed that all patients with a patent IMA at the origin of the aorta developed a T2EL, while only 65% of patients without T2EL had a patent IMA (p=0.003). Mean IMA diameter was similar between groups (2.6±0.8mm vs. 2.6±0.7mm) and presence of an IMA with ≥3 mm was more common (50% vs. 45%) in the T2EL group than in the group without T2EL, although this was not significant.
On average patients with T2EL had a total LA diameter and a total combined diameter (LA+IMA) superior to patients without T2EL (11.2±3.6mm vs. 9.6±4.1mm and 13.8±3.7mm vs. 12.2±4.1mm, respectively), none of which achieved statistical significance. Presence of both a LA and an IMA with ≥3mm was associated with development of T2EL (p< 0.001) and was identified in 67% of patients with T2EL versus 22% in patients without T2EL. These results are summarized in Table 2.
Follow-Up
At 12 months, among the patients with T2EL, 3 (17%) patients had sac growth of ≥5mm (mean 5.3mm; range 5-6mm) and two (11%) patients had sac shrinkage of ≥5mm (mean 10mm; range 5 - 15mm). Two (11%) patients developed late T2EL. Among the 16 early T2EL, three (19%) had resolved spontaneously at 12-month reassessment. Except for the patient with a type 3 endoleak, none of the patients with T2EL required reinterventions.
Discussion
The population of our study was primarily comprised of males with a median age of 75 years, which aligns with the literature on the typical profile of patients with abdominal aortic aneurysms.1 The incidence of T2EL in our cohort, at 31%, falls within the range reported in existing literature.1,2,5 Interestingly, most T2ELs were detected early, with 89% identified at one-month follow-up. This finding underscores the importance of surveillance with CTA in the early postoperative period to detect and address endoleaks promptly and has been recommended by recent guidelines on follow-up after EVAR.1,6
Demographic factors such as age and gender did not associate with the development of T2EL in our study, nor did common cardiovascular risk factors and medication, although one should take into consideration that among the only two treated females in our population, one developed a T2EL (50%), which might suggest a bias due to the relatively small size of our sample; despite this older age, female sex, hypertension and non-smoking habits have inconsistently been reported has risk factors for developing T2EL.1,7,8
Our analysis revealed several noteworthy associations between aneurysm characteristics and the development of T2EL. Notably, we found a statistically significant association between aneurysm shape and T2EL development, with saccular aneurysms demonstrating a higher propensity for T2EL compared to fusiform aneurysms (62% vs. 26%). To our knowledge, this finding has not been further investigated in the literature, as most studies excluded patients with saccular aneurysms. However, Kuijpers et al. have reported similar findings for patients treated with polyester grafts.5Despite having fewer feeding vessels, saccular aneurysms may be prone to T2EL due to being associated with less preoperative mural thrombus, as well as to differences in hemodynamics within the sac and localized arterial wall weakening in the region where the aneurysm protrudes.
Additionally, we observed a counterintuitive trend where in smaller aneurysm size was associated with a higher incidence of T2EL (58.1±8.4mm with T2EL vs 67.3±15.1mm without T2EL). Initially we had considered that this was due to the higher incidence of saccular aneurysms in the T2EL group. However, after performing a sub-analysis by excluding patients with saccular aneurysms, aneurysm size was still significantly different between groups (mean 60.5±5.6mm with T2EL vs 69.7±7.4mm without T2EL; p= 0.022). This finding may warrant further investigation to elucidate potential mechanisms underlying this association.
Regarding collateral patency, patients with a T2EL had both a higher number of overall covered LA and patent covered LA when compared to patients without T2EL; as it would be expected these findings were only significant for patent LA (p= 0.025). Covering more than three patent LA was also associated with T2EL (78% vs. 45%). Similarly, IMA patency was present in all patients with T2EL and associated with this complication (100% vs. 65%). Both results matched previously published literature regarding LA and IMA patency1,2,9
Presence of a patent IMA ≥3mm and LA ≥2mm has been reported as a common risk factor for developing T2EL1,2 yet this was not the case in our cohort. Despite patients in the T2EL group presenting more commonly with larger IMA and LA than patients without T2EL (50% vs. 45% and 56% vs.32%, respectively), this finding did not achieve statistical significance. In fact, we had to raise the cut-off value for LA size from 2 to 3mm as all patients in our sample had at least one lumbar artery with 2mm.
Similar results were obtained when analysing both average LA diameter, total LA diameter, IMA diameter and total combined diameter (LA + IMA diameters) which were slightly higher for patients with T2EL (2.2mm, 11.2mm, 2.6mm and 13.8mm, respectively), than for patients without T2EL (2.2mm, 9.6mm, 2.6mm and 12.6mm, respectively), none of which achieved significance. Interestingly, the combined presence of a LA and IMA ≥ 3mm was significantly more common in patients exhibiting T2EL (67%) than in patients without this complication (22%). Despite these findings, the authors acknowledge that the non-significant effect of collateral size on T2EL may suggest a limitation due to the relatively small sample size of the study. A larger sample might reveal a significant impact of collateral size, as previously described in the literature.
Lastly, regarding sac remodelling, no reinterventions were required for T2EL in our study, yet at 12 months we noticed that 3 (17%) of these patients showed signs of sac growth ≥5mm (although <10mm); had the follow-up period been longer it is likely that not only more cases of sac enlargement would be identified but also that continuous sac growth could have led to reinterventions.
Conclusion
The significant incidence of T2EL highlights the need for a deeper comprehension of the factors contributing to their development following EVAR. Our findings underscore the prognostic relevance of specific aneurysm characteristics, notably saccular morphology and collateral patency, namely the presence of more than three patent covered lumbar arteries or a patent inferior mesenteric artery. However, the lack of association between vessel diameter and T2EL in our study prompts further exploration into the nuanced interplay between collateral size and endoleak risk. While prophylactic embolization of LA and IMA may benefit certain patients, the lack of association between vessel diameter and T2EL warrants additional investigation to refine embolization strategies.