Introduction
The link between extracranial carotid artery disease and visual symptoms is well-established in clinical practice. Amaurosis fugax, characterized by transient monocular blindness, has been recognized as a precursor to retinal transient ischemic attacks (TIAs). The visualization of cholesterol emboli and fibrin-platelet aggregates within the retinal circulation has provided compelling evidence that carotid plaque embolization can lead to TIAs and strokes. However, not all cases of transient visual symptoms can be attributed to embolization. While carotid atherosclerosis explains some instances of amaurosis fugax, other cases are associated with chronic ocular ischemia resulting from hypoperfusion of the eye.1
This can manifest as visual symptoms resembling classic amaurosis fugax, where severe occlusive carotid lesions may lead to ocular hypoperfusion instead of emboli.2 Our study aims to investigate the potential improvement of visual symptoms following carotid endarterectomy (CEA) in patients with significant carotid stenosis and concurrent hypoperfusion-related ocular manifestations. Through a systematic review, we aim to contribute valuable insights regarding the impact of carotid revascularization on chronic ocular ischemic syndrome (OIS) and associated visual symptoms.
Methods
Literature Search:
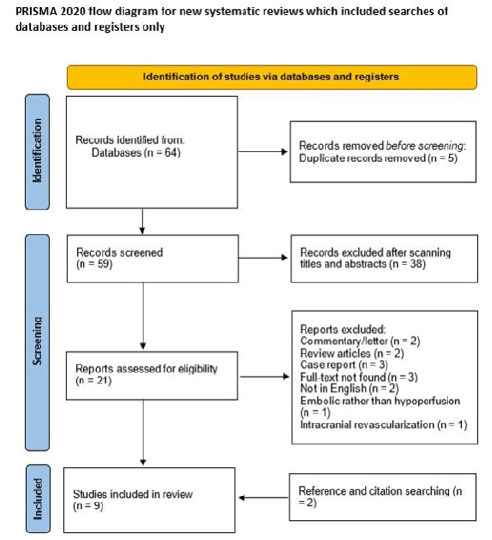
We conducted an electronic search in the PubMed and Embase databases, using a PICO-based keyword combination: (ocular ischemia OR ocular hypoperfusion*) AND (carotid endarterectomy* OR carotid surgery*) AND (outcomes*). PRISMA guidelines were followed.3 After removing duplicates, 59 articles were screened by title. Non-relevant articles were excluded, yielding 21 articles for analysis. From this pool, seven studies were meticulously selected for inclusion. In addition, two articles were included through backwards citation, culminating in a total of nine articles for our systematic review, Figure 1.
Data Collection:
Two independent reviewers manually extracted data from the selected articles. Automation tools were not employed.
Inclusion Criteria:
Our inclusive approach encompassed studies involving patients with OIS or ocular hypoperfusion, exploring the relationship between carotid endarterectomy and outcomes. Study designs included retrospective, prospective, and randomized studies, and meta-analyses with reported statistical values. Gender, ethnicity, and socioeconomic status were not grounds for exclusion. Commentary, letters, expert opinions, non-English articles, animal studies, and those involving pregnant populations were excluded.
Statistical Methodology:
To assess the impact of carotid revascularization on visual outcomes and ocular perfusion, we performed a pooled analysis of the relevant studies. Statistical values reported in the individual studies, such as percentages, mean differences, p-values, and confidence intervals, were extracted.
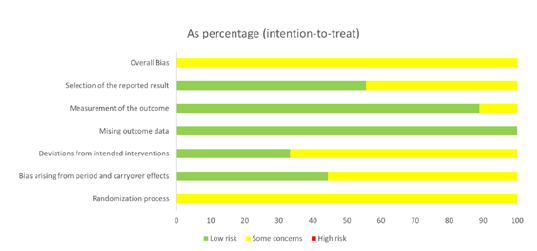
For studies reporting visual acuity, visual field measurements, or ocular blood flow parameters, we performed a qualitative synthesis of the outcomes. For categorical data, the proportions of patients with visual improvement or stabilization were compared across studies. Statistical significance was set at p<0.05. Risk of bias was evaluated using ROB2 crossover bias assessment, Figure 2.
Results
In total, 545 patients were included across nine studies, comprising five retrospective cohort studies and four prospective studies. The baseline characteristics of the patients revealed that most had significant carotid artery stenosis and presented with visual symptoms indicative of ocular ischemia or alterations in ocular blood flow parameters. The patients were 74.2% male and 25.8% female, with a mean age of 65. The most prevalent comorbidities were hypertension, dyslipidemia, tobacco abuse, diabetes, coronary artery disease, and peripheral artery disease.
Carotid Revascularization in Symptomatic Patients and Visual Acuity:
The impact of carotid revascularization on visual functions and ocular blood flow acuity in patients with chronic OIS has been investigated across multiple studies. Five studies, comprising four retrospective studies and one prospective study, with most reporting significant improvements or stabilization of visual function post-procedure, Table 1.
Visual acuity improved or stabilized in 94-100% of cases following carotid revascularization in one study, highlighting the benefits of addressing severe carotid artery disease, as 95% of patients had experienced significant visual deterioration prior to the procedure.4,5 Similarly, other studies reported notable gains in visual acuity after surgery, with statistically significant improvements sustained at 6 and 12-month follow-ups, alongside enhancements in optic nerve function and ocular blood flow parameters, in both acute and chronic OIS cases.5,6
Both CEA and carotid artery stenting (CAS) were effective in improving OIS-related visual outcomes, with comparable efficacy between the two interventions, though both outperformed medical treatment alone.7 However, not all studies reported superior outcomes for surgical interventions. One investigation found that the visual prognosis for OIS remained poor, with significant deterioration in visual acuity for patients with advanced disease, regardless of whether they underwent CEA or received medical therapy.8
Carotid Revascularization in Ocular Hypoperfusion:
Four pertinent studies, one retrospective and three prospective, were examined to ascertain the impact of CEA on ocular blood flow in patients with carotid disease, Table 2.
Cohn et al. analyzed 25 patients with ≥70% ICA stenosis who underwent 29 CEAs to evaluate CEA impact on ocular perfusion via ophthalmic artery (OA) and central retinal artery (CRA) flow velocities. Color-flow ocular duplex scanning measured pre- and post-op velocities. Post-operatively, velocities significantly increased (OA: 38.6 cm/s, p<0.0001; CRA: 12.1 cm/s, p=0.0008). Patients with ocular symptoms had lower pre-operative CRA velocities than those without (p=002). Reversed OA flow pre-operatively didn't correlate with symptoms and all restored anterograde flow following surgery.9 Yoshida et al. conducted a retrospective study to study CEA's effect on ocular ischemia in 41 patients with carotid artery stenosis. Laser speckle flowgraphy measured ocular blood flow (OBF) changes. OBF increased post-CEA on the operated side (p<0.001) but not on the other side (p=0.50). 56.1% reported subjective visual acuity improvement post-CEA. Contrast sensitivity (CSV-1000) scores increased in patients with increased OBF (p=0.04). In those with decreased vision and OBF, CSV-1000 scores significantly improved (p<0.001). Authors conclude that CEA can enhance OBF and reverse ocular ischemia-related visual issues.10
Geroulakos et al.'s prospective study included 22 patients with severe carotid stenosis undergoing CEA. Pre- and post-operative measures of OA and CRA peak systolic velocity (PSV) and peak diastolic velocity (PDV), along with macular photostress recovery and visual parameters, were analyzed. Post-revascularization, CRA PSV increased by 50% (p=0.005), CRA PDV by 22% (p=0.03), and OA PSV by 51% (p=0.001), while macular photostress decreased (p=0.001). Visual acuity improved or stabilized in 77.3% of patients. The findings imply that carotid surgery enhances ocular hemodynamics. 11
Yan et al. assessed post-CEA vision changes in 15 patients (30 eyes) with severe carotid artery stenosis (>70%). Standard ophthalmic examination measured visual acuity, intraocular pressure (IOP), kinetic and static visual fields (VF). Optical coherence tomography scanned retinal nerve fiber layer (RNFL) thickness. Post-CEA, visual acuity improved, IOP decreased (p=0.0022), kinetic VF range increased (p=0.0126), mean sensitivity improved (p=0.0208), and mean defect decreased (p=0.025). Auhtors concluded that CEA enhances both subjective and objective visual function but doesn't affect RNFL thickness. 12
DISCUSSION
The reviewed studies collectively underscore the potential of CEA to improve visual function and alleviate ocular hypoperfusion-related symptoms effectively. These findings emphasize the significance of carotid revascularization in the outcomes of OIS. Furthermore, the observed improvements in visual acuity, visual fields, and ocular blood flow parameters support the notion that CEA positively impacts both subjective and objective aspects of visual function.Considering the 2023 European Vascular Guidelines on the management of atherosclerotic carotid and vertebral artery disease, which emphasize the potential benefits of carotid revascularization in patients with OIS, the findings from our systematic review further corroborate the potential of such interventions in managing ocular hypoperfusion-related symptoms.13
Our review supports the notion of progressive nature of visual impairment in OIS, by highlighting the substantial improvements in visual function observed post-CEA in patients with chronic OIS.
Studies by Clouse et al., Neroev et al., Kawaguchi et al., and Yan et al. all reported stabilization or improvement in visual acuity following CEA, suggesting a potential reversal or mitigation of the visual deterioration associated with chronic ocular ischemia.4-7Across the reviewed studies, CEA led to improvements in ocular perfusion parameters, such as ophthalmic artery and central retinal artery flow velocities.
Table 1 Characteristics of articles reporting on patients treated for splenic artery aneurysm, from January 2019 to January 2024, included in the systematic review
| Authors / date / country | Study design | N | Female | Age - mean | Degree of stenosis | Main findings |
|---|---|---|---|---|---|---|
| Clouse et al. 2002 USA | OR | 17 | 29% | 66 | >50% | Symptomatic eyes had worse ipsilateral ICA stenosis. Subjective visual improvement or stabilization in 94% following CAE |
| Kawaguch et al. 2001 Japan | OP | 11 | 0% | 67 | >70% | Reversed flow in OA resolved in each patient after CAE. The average peak systolic flow velocity rose significantly. At the end of follow-up period, visual acuity had improved in 5 patients and had stabilized in the other 6 patients. |
| Neroev et al. 2012 Russia | OR | 180 (104 acute) | 12% | 61 | >70% | After CAE, visual acuity increased. Mean indices of blood-flow velocities increased at 6 and 12 months after surgery. There was ocular blood flow acceleration and decrease of vasoresistance in orbital arteries in both groups. |
| Sivalingam et al. 1991 USA | OR | 52 (15 CAE) | 27% | 64 | Mean 97% | Subjective visual improvement or stabilization in only 40% (4 of the 15 CAE were performed on occluded ICA), compared to 39% in patients treated medically. |
| Yan et al. 2013 China | OR | 182 (78 OIS) | 41% | 65 | 69% (with OIS) | OA hemodynamics indices significantly improved in patients with OIS treated with CAS and CAE. Both CAE and CAS were more effective than medical treatment. |
OR - observational retrospective; OP - observational prospective; OIS - oculo-ischemic syndrome; ICA - internal carotid artery; OA - ophthalmic artery; CEA - carotid endarterectomy; CAS - carotid stenting;
Table 2 Summary of studies evaluating the impact of carotid endarterectomy on ocular blood flow.
| Authors / date / country | Study design | N | Female | Age - mean | Degree of stenosis | Main results |
|---|---|---|---|---|---|---|
| Cohn et al. 1999 USA | OP | 25 (29 CAE) | 36% | 69 | >70% | After CEA, the PSV increased significantly in OA and CRA. The patients with OIS had significantly lower preoperative PSVs in the CRA as compared with those patients without visual symptoms. |
| Geroulakos et al. 1996 UK | OP | 22 (23 CAE) | N/A | 68 | Mean 75% | The CRA PSV increased by 50% and PDV increased by 22%. The OA PSV increased by 51%. Visual acuity improved or stabilized in 77.3% of the patients. |
| Yan et al. 2019 China | OP | 15 | 27% | 62 | >70% | After CEA, both uncorrected and visual acuity improved,intraocular pressure significantly decreased. Kinetic visual fields range increased significantly |
| Yoshida et al. 2021 Japan | OR | 41 | 15% | 74 | Median 72% | OBF significantly increased after CEA. After CEA, 56% of patients reported subjective visual improvement on the operated side. Visual acuity improved significantly among the patients with increased OBF after CEA but not among those without increased OBF. The visual acuity scores increased significantly after CEA in 18 patients with decreased vision and decreased OBF, but not in the 23 patients without those. |
OR - observational retrospective; OP - observational prospective; OIS - oculo-ischemic syndrome; ICA - internal carotid artery; OA - ophthalmic artery; CEA - carotid endarterectomy; CAS - carotid stenting; PVS - peak systolic velocity; PDV - peak diastolic velocity; CRA - Central retinal artery; OBF - Ocular blood flow.
Subjective enhancements in visual acuity and other visual parameters accompanied these improvements. The findings collectively underscore the efficacy of CEA in reversing ocular hypoperfusion-related symptoms and improving both subjective and objective aspects of visual function.
In clinical practice, the findings from our review suggest that carotid revascularization, particularly carotid endarterectomy (CEA), could play a crucial role in managing patients with ocular ischemia and carotid artery disease. Given the potential for visual improvement and stabilization post-CEA, clinicians should consider early intervention in patients with significant carotid stenosis who present with visual symptoms suggestive of ocular ischemia. This approach underscores the importance of recognizing ocular ischemic symptoms as an indicator for possible surgical intervention, especially in patients with severe carotid stenosis.
This systematic review has several limitations that should be considered. Firstly, the included studies exhibited heterogeneity in study designs, sample sizes, and outcome measures, which may limit the generalizability of the findings. Many studies relied on retrospective data, introducing potential biases and restrict the ability to establish causality. Additionally, the small sample sizes in some studies reduce the statistical power to detect differences or associations, and the lack of standardized protocols for measuring ocular blood flow and visual outcomes further complicates comparisons across studies. Another limitation is the variability in follow-up durations, with some studies providing only short-term data, which may not fully capture the long-term effects of carotid endarterectomy (CEA) on visual function. Furthermore, the exclusion of non-English articles may have introduced selection bias, potentially omitting relevant studies published in other languages or regions.
Conclusion
In conclusion, this systematic review summarizes the impact of CEA on visual symptoms and ocular hemodynamics in patients with carotid artery stenosis and associated ocular ischemic manifestations. Our analysis highlights the promising potential of CEA as a therapeutic intervention for enhancing visual outcomes in patients with carotid artery stenosis and ocular hypoperfusion-related symptoms.
urability of CEA in managing ocular ischemia.