Introduction
Type IV thoracoabdominal aortic aneurysms (TAAA-IV) compose up to 25% of thoracoabdominal aortic aneurysms. Though fully intra-abdominal, they have far different outcomes from more distal abdominal aortic aneurysms. Nonetheless, morbidity and mortality appear greater in the remainder of thoracoabdominal aneurysms other than type IV, probably due to simpler surgical techniques and no need for distal perfusion/extracorporeal circulation.1
Mortality rates of 7 to 11% are generally described in current literature from high-volume centers, but may increase up to 20%.2,3 Post-operative complications are common, and mostly renal, cardiac, and pulmonary.4 Survival at five years has been estimated at 62%.5
This study aims to perform a descriptive analysis and outcome evaluation of open repair of type IV aneurysms in our center, in an elective setting.
Methods
This study followed the reporting guidelines for cohort studies from the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement.
An observational, descriptive, single-center, retrospective cohort study was performed from January 2008 to December 2023. The primary endpoint was in-hospital mortality, but data regarding acute and late complications and the need for re-intervention were also analyzed. All consecutive patients submitted to open repair of TAAA-IV were included. Patients submitted to repair in urgent/emergent settings (ruptured, symptomatic, or mycotic) were excluded. There was no restriction regarding the surgical approach to the visceral and renal arteries.
Patient identification was retrieved from the operating room logbook and previous department databases. The remaining data was obtained from the hospital records. Imaging data regarding pre- and post-operative imaging was obtained from the hospital imaging database. CTA’s were used to evaluate aortic measures, patency of visceral and renal arteries, and other long-term complications.
In hospital logs were consulted, collecting data regarding post-operative complications, namely stroke - with neurological signs and CT scan lesions; myocardial infarction (MI) - with clinical signs and myocardial enzymes elevation; acute kidney injury (AKI), defined as urinary output bellow 0,5mL/kg/h or an increase in at least 1.5x basal serum creatinine (Acute Kidney Injury Network - AKIN I AKI) and possible need for hemodialysis; intestinal ischemia, with endoscopic, CTA and/or operative confirmation; and paraparesis, with documented de novo motor deficit. In ambulatory settings, appointment logs were consulted, and data regarding clinical or laboratory de novo findings were collected.
We performed a descriptive analysis of our data. Continuous variables are presented as mean (standard deviation) if normally distributed and median (minimum-maximum) if not. Dichotomous and categorical variables were expressed in numbers (percentage). Statistical analysis was carried out using STATA 16 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC).
Results
From our logs, 38 patients were initially identified. Ten urgent/emergent cases and four other cases were excluded due to inconsistent records, resulting in a final cohort of 24 patients, Table 1. Twenty-two were men (91,6%), with a mean age of 68 years (SD 7.6). The mean aortic diameter was 69,6mm (SD 16.2).
Table 1 Demographics of patients with elective type IV thoracoabdominal aneurysm, included in the study.
| Variable | N=24 |
|---|---|
| Age, years - mean (SD) | 68 (7.6) |
| Male gender - N (%) | 22 (92) |
| Hypertension - N (%) | 15 (62) |
| Past smoking - N (%) | 14 (58) |
| Current smoking - N (%) | 9 (37) |
| Diabetes - N (%) | 3 (12) |
| CKD (Creatinine >1.5) - N (%) | 14 (58) |
| Coronary artery disease - N (%) | 4 (17) |
| Peripheral artery disease - N (%) | 8 (33) |
SD - standard deviation; CKD - chronic kidney disease
All patients were submitted to paramedian laparotomy with medial visceral rotation. The approach to visceral and renal branches varied. Most reconstructions (22, 92%) were performed with a beveled anastomosis, encompassing the celiac trunk (CT), superior mesenteric artery (SMA), and right renal artery (RR). Most variations were due to the left renal artery (LR), with five revascularized by heterologous bypass (6mm Dacron grafts), two abandoned due to atrophic kidneys, and the remaining 16 re-implanted.
The median hospital stay was 20 days (4-131), and the intensive and intermediate care stay was 7 days (1-62).
A summary of complications is presented in Table 2. The most common complication was AKI, in 87% (N=21), AKIN 3 in 39% (N=7), requiring hemodialysis in five patients (21%), only one with no recovery (4%). We found a rate of 29% of infectious complications (seven in five patients). Lower respiratory infection was the most common (17%), followed by one non-ischemic perforated diverticulitis and one superinfection of an ischemic kidney. Left renal artery occlusions occurred in 37% (N=7/19), most of them (N=5; 26%) after re-implantation and 10% (N=2) of the right renal artery; one patient had bilateral renal artery occlusion. During follow-up, there was no visceral artery occlusion (Figure I). Two patients (8%) had cardiac complications - one acute myocardial infarction and one non-ischemic cardiogenic shock.
Table 2 In-hospital and late complications of patients with type IV thoracoabdominal aneurysm treated with elective open surgery, included in the study.
| Complications | N (%) |
|---|---|
| In-Hospital | |
| Infection (n=21) | 7 (29) |
| Brachial plexus lesion (n=21) | 1 (5) |
| Wound infection | 1 (5) |
| UTI | 1 (5) |
| Peritonitis | 1 (5) |
| Cardiac (n=21) | 2 (9) |
| AMI | 1 (5) |
| Acute Cardiac Insufficiency Cardiogenic shock | 1 (5 |
| AKI (n=24) | 21 (87) |
| AKIN 1 | 11 (46) |
| AKIN 2 | 3 (12) |
| AKIN 3 | 7 (29) |
| HD | 5 (21) |
| Acute limb ischemia (n=21) | 4 (19) |
| Intestinal ischemia (n=21) | 1 (5) |
| Stroke (n=21) | 1 (5) |
| Brachial plexus lesion (n=21) | 1 (5) |
| Late (n=18) | 7 (39) |
| Aortic dilation (contiguous aneurism) | 2 (11) |
| Anastomotic pseudoaneurysm | 2 (11) |
| Limb occlusion | 2 (11) |
| Graft infection | 1 (5) |
VAP - ventilator-associated pneumonia; UTI - urinary tract infection; AMI - acute myocardial infarction; AKI - acute kidney injury; AKIN - Acute Kidney Injury Network score; HD - hemodialysis
Late complications were related to aortic and graft related events, with two aortic dilations (one of a visceral patch) at 13 months and seven years, two anastomotic false aneurysms at five and nine years, two graft limb occlusions, at nine and 12 years and one infected graft, which is associated to the false aneurysm and limb occlusion at nine years. None of these patients had progression of dilation warranting re-intervention for the time they were followed at our institution. Limb occlusions presented as claudication, not leading to re-intervention, and the patient with the infected graft was treated conservatively with prolonged antibiotic therapy until his death (approximately two years later), from other comorbidities. Target vessel patency is presented in Figure 1.
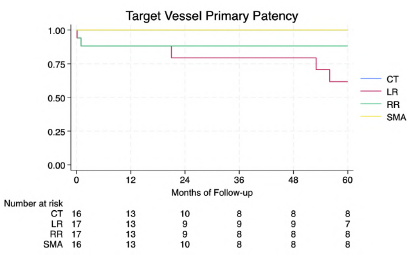
Figure 1 Kaplan-Meier analysis of target vessel patency of patients with type IV thoracoabdominal aneurysm treated with elective open surgery, included in the study. CT - celiac trunk; LR - left renal artery; RR - right renal artery, SMA - superior mesenteric artery.
In our cohort, two patients had lower limb ischemia in the early post-operative period, warranting re-intervention (thromboembolectomy in one and construction of an axilo-bifemoral bypass in another), and two others, already mentioned, an acute diverticulitis with need for sigmoidectomy, and left renal ischemia with super-infection, requiring nephrectomy. Still, a 91% (95% CI 51-99%) rate of freedom from re-intervention at two years was found, Figure 2.
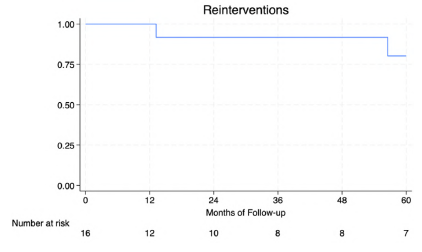
Figure 2 Kaplan-Meier analysis of re-intervention of patients with type IV thoracoabdominal aneurysm treated with elective open surgery, included in the study.
The overall in-hospital mortality rate was 21% (5/24). Two patients (8.6%) died intra-operatively, both in refractory hemorrhagic and distributive shock, one of them due to disseminated intravascular coagulation associated with a known immune thrombocytopenic purpura. One patient (4%) died in the first 24 hours, also in refractory distributive shock. In the long-run, the Kaplan-Meier survival analysis shows survival rates of 80% 1 year (95% CI 50-93). We assume our data may be highly affected from reporting bias and losses to follow-up (42%).
Discussion
As previously stated, mortality rates of surgical repair of TAAA-IV are highly variable and may be as high as 20%.3 The most extensive series reported, by Coselli et al,6 comprising 427 patients over up to 20 years, described a mortality rate of 3%. In another series with a large numbers of patients, Patel et al reported an in-hospital mortality of 2.8%.4 However, Kieffer et al and Bicknell et al, with 174 and 130 patients, respectively, reported 13% and 20% mortality rates.1,3 Our cohort comprises only 24 patients, with no urgent cases considered (unlike these high volume series), with a compound in-hospital mortality of 21%. These authors, nonetheless, refer in their works that operative mortality is reduced with higher surgeon and institutional experience, with Kieffer1 describing a specific difference in outcomes from their most experienced surgeons in this approach. One of the factors described as significant is the presence of visceral bypass and increased visceral ischemia time.3 There also seems to be a high rate of urgent repairs in the series with the poorest results. In a meta-analysis published in 2018, the analysis of nine studies showed a pooled mortality rate of 7.20% (95%CI: 4.19-10.84).2
In comparison, endovascular series show much lower mortality rates. Oderich et al report 1.8% early mortality in a cohort of 112 Crawford type IV aneurysms, with a 56% survival rate at 5 years.8 Nonetheless, early adverse event rates are not at all negligible, with a total of 36% in this cohort, including spinal cord injury (2.7%).
Renal occlusion has been described in up to 39% of patients with higher numbers in bypasses and branches than natives arteries, and acute kidney injury is globally recognized as the main complication, but Patel et al has shown an increased likelihood associated with previous chronic kidney disease.4,5 In our series, renal artery occlusion seems to be, according to data in literature, with a much higher rate of AKI, which may be attributable to hemodynamic factors and previous CKD. Our complication rate is high, but mostly attributable to AKI and infections, with a low need for re-intervention.
We still find several late graft and aortic-related complications (39%), but this doesn’t seem to be far from the literature (32% in a cohort of 154 patients)7 and with a low need for re-intervention in the long term.
Limitations to our study include the small cohort and its retrospective nature, which limits the data collection to clinical reports with a high risk of reporting bias. There is also a wide variability of follow-up, both due to duration and important losses to follow-up, with potential loss of a wide array of medium-and long-term data, mostly in aortic and graft-related complications or lack thereof.
Conclusion
In this cohort we found a high mortality rate (superior to those described in high volume centers), which leads us to assume that results highly depend on surgical and post-operative care experience. Complications are frequent, especially AKI, which is much more frequent than the loss of renal arteries, leading us to assume other causes are in play.















