Background
Primary aortic mural thrombus (PAMT) is a rare cause of peripheral embolization and is often associated with hypercoagulable states. In most cases, the diagnosis is made following an embolic event. Anticoagulation therapy is typically the first-line treatment; however, it carries a significant risk of embolization, which can be as high as 73% in patients with pedunculated thrombi.1-3 To address this risk, TEVAR (Thoracic Endovascular Aortic Repair) has emerged as a successful alternative. Compared to open surgery, TEVAR is minimally invasive and offers lower perioperative morbidity and mortality. It is particularly effective in achieving thrombus exclusion, thereby preventing embolization to distal arterial beds, as previously mentioned.2-4
Case Report
A 51-year-old male patient, under follow-up for right lung carcinoma, underwent a computed tomography angiography (CTA) scan for staging of the lung disease. Incidentally, a thrombus in the descending thoracic aorta was detected. The patient’s medical history included hypertension, diabetes mellitus, dyslipidemia, and obesity. Given that the patient was asymptomatic, conservative treatment with enoxaparin at a dose of 1 mg/kg was initiated.
However, one week later, the patient developed symptoms of pain and paresthesia in the left lower limb, without motor impairment. On physical examination, only the right femoral pulse was palpable. An arterial Doppler ultrasound identified emboli in the left femoral arteries. These findings were confirmed by CTA, which revealed near-total occlusion of the left common femoral artery at its bifurcation and a distal occlusion of the left superficial femoral artery. The CTA also identified two distinct pedunculated floating thrombi in the descending thoracic aorta. The proximal thrombus appeared to be the same one previously detected incidentally, though it had decreased in size. The distal thrombus, however, was a new finding, Figure 1. Hence, a diagnosis of left acute limb ischemia, Rutherford grade IIa, due to embolization originating from a PAMT was assumed. Continuous perfusion of unfractionated heparin was initiated, and urgent surgery was proposed.
Two pediculated thrombi are visible in the anterior aspect of the descending thoracic aorta. Two pediculated thrombi are visible in the anterior aspect of the descending thoracic aorta.
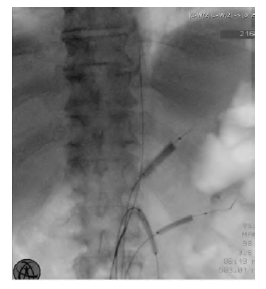
TEVAR was performed to control the embolic source and prevent further events. To minimize the risk of visceral embolization during the procedure, selective catheterization of the visceral arteries was carried out via the contralateral right common femoral artery, where a 12Fr sheath was placed. Low-pressure angioplasty balloons were inflated in the visceral arteries, including the celiac trunk, superior mesenteric artery, and left renal artery, Figure 2. The left renal artery was selected due to its better appearance when compared to the right. The thrombi were successfully excluded using a Valiant® stent graft (30x150mm), with a 20% oversize relative to the native aortic diameter. Subsequently, a left transfemoral thrombectomy was performed, achieving normal blood flow to the foot.
Low-pressure angioplasty balloons are seen inflated in the celiac trunk, superior mesenteric artery, and left renal artery, prior to stent graft deployment
No adverse events occurred during the postoperative period. The patient was discharged on a regimen of aspirin 100 mg and rivaroxaban 20 mg and has continued under close follow-up in outpatient care for five years, remaining asymptomatic. Follow-up CTA confirmed the correct positioning of the thoracic aortic graft and showed no evidence of thrombus recurrence, Figure 3.
A thoracic stent graft is visible, adequately excluding the pre-existing mural thrombus
Discussion
Although rare, PAMT should be considered as a potential embolic source, particularly in patients with hypercoagulable states such as malignancies. Due to its rarity, the management of PAMT remains controversial.2-5 Anticoagulation alone is usually considered the first-line treatment. However, compared to intervention, there is a higher risk of thrombus persistence and embolization.6 Traditional open surgery offers the advantage of immediate and complete thrombus removal. Nonetheless, this approach is significantly more invasive and is associated with risks such as bleeding, infection, and anesthesia-related complications. TEVAR for thrombus exclusion emerged as a successful alternative, offering lower perioperative morbidity and mortality while demonstrating potentially equal or superior efficacy compared to classic open surgery.3
Using low-pressure angioplasty balloons as a protective measure against visceral embolization proved an effective strategy. In fact, Sadeghi-Azandaryani et al. described a similar technique in 2009 during open thoracic aortic repair to prevent visceral embolization.7
Our case demonstrates that in cases of recurrent embolization despite anticoagulation therapy, using TEVAR to exclude aortic thrombi effectively prevents additional embolization. In these circumstances, the risks associated with the procedure are possibly outweighed by the potential catastrophic complications related to embolization.