Background
Tumours of the Inferior Vena Cava (IVC) are rare. These may be classified as primary or secondary tumours. Less than 500 cases are described in the literature as primary tumours, mostly leiomyosarcomas.1 Leiomyomas are even rarer and originate in the smooth muscle of the IVC walls. The most frequent secondary tumours are intravenous leiomyomatosis, which is only present in women, arising from the uterus and propagating through the blood to the IVC walls.2,3 Symptoms typically manifest late over the course of the disease and are often nonspecific. The only definitive treatment is surgery. The authors present a case of a leiomyoma of the IVC, initially diagnosed as a deep venous thrombosis.
Case Report
A 49-year-old male patient, with a history of varicose vein surgery one month prior, presents to the emergency department with right leg swelling. The surgery had been performed in another institution, and further information could not be retrieved. Doppler ultrasound revealed thrombosis of the right iliac and femoral vein, with presumed permeability of the IVC, given the symptoms were unilateral. These findings were confirmed by computed tomography angiography (CTA), which also revealed pulmonary thromboembolism. The patient remained in the hospital for one week and was discharged on anticoagulation therapy, with rivaroxaban 15mg bid, and prescribed class 2 elastic compression stockings.
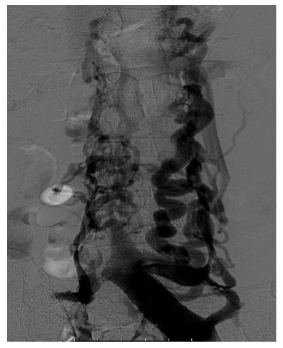
After one year, the complaints of right leg swelling and discomfort persisted, raising the suspicion of post-thrombotic syndrome. A CTA revealed a 12 cm thrombus in the infrarenal IVC, Figure 1. Despite ongoing anticoagulation, symptoms persisted with intermittent improvements and worsening. The diagnostic workup and the proposal for surgery were delayed due to circumstances caused by the COVID-19 pandemic.
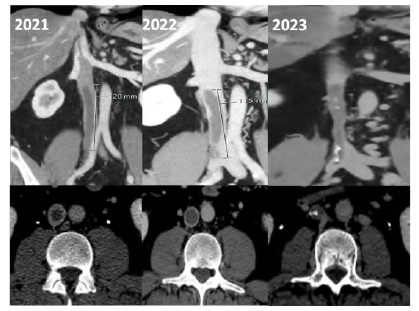
Figure 1 Computed tomography angiography - coronal (top) and axial (bottom) views.Evolution over time is noted from left (2021) to right (2023).
Consequently, a phlebography, a magnetic resonance, and a positron emission tomography (PET) scan were performed to clarify the etiology, which raised the suspicion of a leiomyoma of the IVC. The PET scan was conducted to determine whether the lesion exhibited high proliferation, which could indicate a malignant neoplasm. Nevertheless, the mass was identified as a low-proliferation lesion. The phlebography confirmed an occlusion of the inferior vena cava with repermeabilization above the known lesion, with slow progression of contrast. Subsequently, an endovascular biopsy, performed with a Cordis® biopsy catheter, confirmed the suspicion of a IVC leiomyoma. A left femoral access was obtained with a 9Fr introducer, the biopsy catheter was then advanced to the IVC wall, and a mass sample was collected, Figure 2 and 3. The biopsy was successful, with the histopathological examination reporting a myxoid leiomyoma.
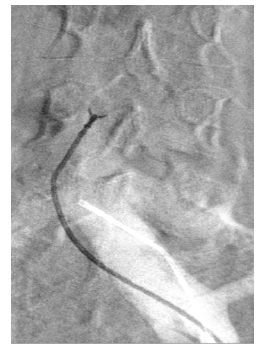
Figure 3 Intra-procedural fluoroscopy image. The endovascular biopsy catheter is shown collecting IVC samples.
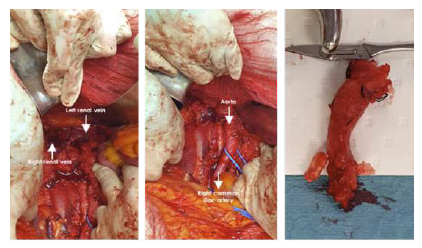
Surgical tumour resection and IVC reconstruction, if needed, were proposed and accepted by the patient, given the risk of distal progression of the leiomyoma with possible compromise of the renal veins. A xiphopubic incision was completed to facilitate visualization of the IVC. A meticulous dissection was carried out, confirming the presence of the neoplastic lesion, which was subsequently resected. IVC reconstruction was deemed unnecessary, since the patient already had a well-developed collateral circulation, Figure 4. The operation was performed under general anesthesia with a duration of 3h30, no intraoperative heparin was administered and estimated blood losses were 300 cc.
On the left, exposure of the IVC and renal veins; on the center, tumor resection; on the right, surgical specimen.
The postoperative period was uneventful. The patient was anticoagulated with low-molecular-weight heparin (enoxaparin) and underwent intermittent pneumatic compression, with no complications. The patient spent three days in intensive care and was discharged from the hospital after a week, with rivaroxaban 15mg bid and compression socks. At the one-month follow-up, the patient remained asymptomatic.
Discussion
IVC leiomyomas often manifest with nonspecific symptoms, such as abdominal discomfort, back pain, weight loss, and recurrent thrombosis. Given its nonspecific symptoms and insidious evolution, IVC leiomyomas are usually diagnosed late in their evolution.1,4 In this clinical case, the patient's sole symptom was thrombosis of the femoral, iliac, and inferior vena cava, which proved refractory to anticoagulation therapy. The diagnostic workup usually involves an ultrasound, CTA and magnetic resonance. However, a biopsy of the tumour is required to confirm the diagnosis.5 Given the location of the IVC, the performance of a percutaneous biopsy can be challenging. Endovascular biopsy, a relatively novel technique that has increasingly been used, was first described to diagnose vascular tumours in 1972 in the United States, where gastroscopic biopsy forceps were used to obtain the biopsy material.6 Since then, several devices have been used to perform the biopsy, and this technique is now safe and effective, reducing the risk of major haemorrhage and the pain related to the biopsy.7,8 In this patient, we performed an off-label endovascular biopsy with a Cordis® biopsy catheter designed to perform endomyocardial biopsies. The IVC biopsy proved to be effective and safe, with no complications associated with the procedure. The resection of the IVC was performed to prevent the proximal propagation of the IVC leiomyoma, which could potentially extend and lead to thrombosis of the renal veins. After IVC resection, IVC reconstruction was not considered, given the poor condition of the iliac vein walls and the extensive collateralization. This proved to be adequate for venous drainage, likely attributable to the extended duration of the pathology.9,10 Reconstruction would also likely result in increased haemorrhagic risk and a higher chance of iatrogenesis, with minimal benefit to the patient.
Conclusions
IVC leiomyomas are exceptionally rare and often manifest with nonspecific symptoms, such as abdominal discomfort, back pain, weight loss and recurrent thrombosis leading to a delayed diagnosis. Given the unspecific symptoms and insidious evolution, IVC leiomyomas require a high level of suspicion to be diagnosed.