Background
At the end of 2019, several health units in Wuhan, China, reported agglomerations of patients with pneumonia with an unknown cause. Epidemiological and etiological investigations detected that the source was a new Coronavirus (SARS-CoV-2) (Zuh et al., 2020). In March 2020, the disease caused by the virus (COVID-19) was declared as a pandemic, due to its global spread, which caused widespread concern among healthcare agencies and professionals (WHO, 2020).
Before the virus quick dissemination and overload of health services, there was limited availability of individual protection equipment and resources for the patients’ treatment. In addition to this, the therapeutic guidelines regarding the coronavirus symptoms were not well established. This context caused a considerable psychological pressure over the health professionals that were in the frontline, especially, nurses (Lai et al., 2020; Xiang et al., 2020), who experienced physical and psychological burden that was observed on previous coronavirus epidemics (Chou et al., 2010; Kang et al., 2018).
Consequently, many nurses have felt confused and unprepared to, adequately treat the patients and experienced feelings of uncertainty and fear, in addition to difficulties in managing their workload. They also had to face the loneliness due to the absence of interaction with relatives for fear of bringing the contamination to their loved ones. The union of these factors can contribute to the appearance of emotional and psychological reactions, such as anger, anxiety, insomnia, and stress associated with the pandemic of COVID-19 (Huang et al., 2020; Ran et al., 2020; Zhang et al., 2020).
The experience of significative psychological stressful factors may lead to the development of Burnout Syndrome, which happens when the work and personal context collaborates to the feeling of overload, anxiety, impotence, stress and exhaustion, caused by an excessive expenditure of energy, strength, and resources (Ko & Kiser-Larson, 2016). The Burnout Syndrome assumes a multidimensional conception, whose manifestation is characterized by emotional, depletion, reduction of the personal fulfillment in work and the professional’s depersonalization (Pêgo & Pêgo, 2016).
Therefore, Burnout is correlated with the nurses’ physical and mental health, with a direct impact on the assistance’s quality and safety (Liu & Aungsuroch, 2019). The Burnout is considered as a construct with three dimensions: 1) Emotional Exhaustion: feelings of fatigue and shortage of emotional resources to deal with a stressful situation and high demands from work; 2) Depersonalization: the manifestation of negative and insensitivity attitudes with the work team, due to isolation behaviors or withdrawal from colleagues and clients and by the affective hardening in interpersonal relationships; and 3) Reduced professional achievement: which is manifested by the sensation of low satisfaction with the work, feeling of detachment from the work and professional frustration (Vieira, 2010; Vieira et al., 2006).
During the epidemic of the MERS-CoV and SARS- CoV in Taiwan, the Middle East and South Korea, the nursing team has lived significative psychological stressful factors, which culminated in high levels of burnout. These conditions were predictors of misconduct, treatment delays due to communication flaws and absenteeism, among others (Ornell et al., 2020; Kang et al., 2018; Chen et al., 2005). Recent studies have already demonstrated the high risk of Burnout development among nurses during the current COVID-19 pandemic (Zerbini et al., 2020; Matsuo et al., 2020).
To extend the identification and comprehension of the constructs associated with burnout is important to subsidize strategies for its prevention, with benefits to the worker’s health and the quality of work (Nogueira et al., 2018).
The identification of the constructs triggering the Burnout syndrome in nurses in the front line of COVID-19 can support the implementation of evaluative and preventive measures focusing on workers' health and guaranteeing excellent nursing care for people diagnosed with coronavirus.
The study aimed to identify constructs that trigger the Burnout syndrome in nurses on the front line to COVID-19.
Method
The adopted knowledge overview method was an integrative review. This method enables the health professionals’ quick access to the research’s relevant results that underlie the conduct and decision making, thus providing critical knowledge (Mendes, Silveira & Galvão, 2008).
For the investigation conduct, six stages were covered: identification of the theme and selection of the research’s guiding question; establishment of inclusion and exclusion conditions for the studies; categorization of primary studies; evaluation of the studies included in the integrative review; interpretation of the results and knowledge overview from the main results revealed in the included articles’ analysis (Mendes, Silveira & Galvão, 2008).The choice to carry out the integrative review was due to the fact that this approach allows a comprehensive synthesis of the subject investigated. The guiding research question of the integrative review was: What constructs triggering the Burnout syndrome are present in nurses on the front line to COVID-19?
For the selection of primary studies, the following databases were consulted: PubMed, Nursing Database (BDENF), Latin American and Caribbean Literature in Health Sciences (LILACS), Web of Science, and Scopus.
The search for primary studies took place from March to August 2020 and updated in May 2021. In each database, the controlled descriptors were delimited (Medical Subject Headings-MeSH and Descriptors in Health Sciences-DeSC) and defined the keywords- key. The search strategy adopted for all databases was (Coronavirus OR “COVID- 19” OR “SARV-COV-2”) AND ("Professional Exhaustion" OR "Professional Exhaustion") AND (Nursing OR "Nurses" ) for BDENF and LILACS; and (“Coronavirus Infections” OR “COVID- 19” OR coronavirus OR “SARV-COV-2”) AND ("Burnout, Professional" OR "Occupational Burnout") AND (Nursing OR Nurse) for PUBMED, Web of Science and SciVerse Scopus.
At this stage of the review, the Rayyan software developed by Qatar Computing Research Institute (QCRI) was used as a tool to support archiving, organization, and selection of the articles.
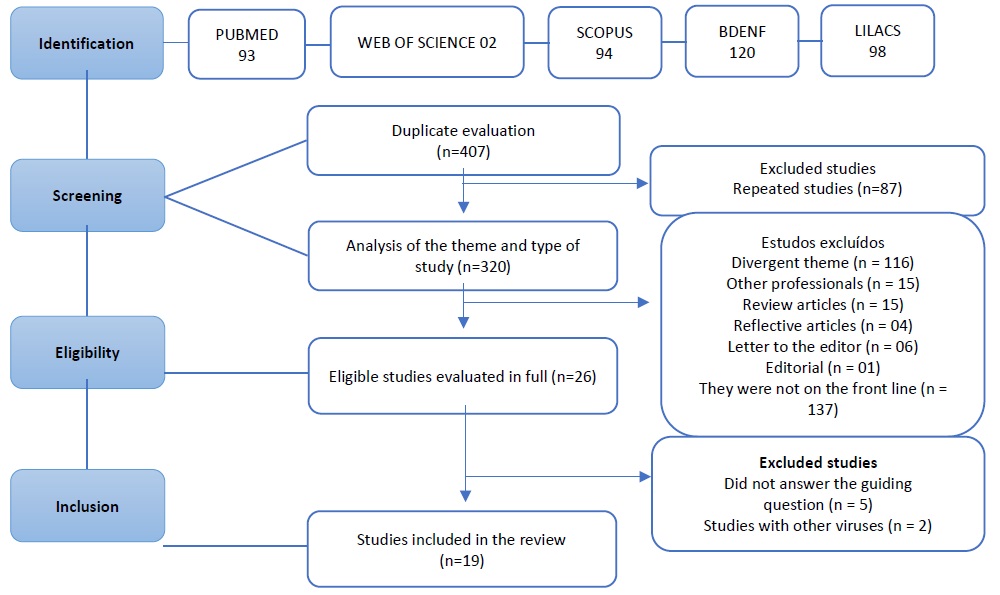
The delimited selection criteria were primary studies that addressed the triggering constructs of Burnout syndrome in nurses in the front line to COVID-19, without time restriction. Case studies, review and reflective articles, editorials, letters to the editor and research notes, studies with professionals who were not on the front line were excluded. For the inclusion of scientific articles, the study followed the flowchart of stages (Figure 1), accordingly with the recommendation from the PRISMA. Primarily, an identification of the studies that involved the theme in the selected databases was made. 407 articles were found, available in the databases.
The studies found in the databases were transported to the Rayyan software, which automatically identified and excluded 87 repeated articles. Moreover, it was made a presetting of the articles with an analysis of the theme and exclusion of duplicates through the reading of the title and abstract. In the following stage, one considered the articles’ eligibility through the reading of the whole content, with an analysis of the methodological rigor and respect to the theme. Finally, 19 records that really possess the capacity to contribute to the study’s scope were included.
The data extraction of the primary studies was made with the support of an instrument that was elaborated and submitted to apparent and content validation (Ursi & Galvão, 2006). This stage was made by two revision authors independently. The data analysis of the integrative review was made descriptively. Each included study was thoroughly analyzed by the authors and two synthesis Tables containing the following information were made: authors, year of publication, objective, sample, city, and year of data collection, dimensions, and constructs related to the Burnout Syndrome in nurses in the front line of COVID-19.
Results
Nineteen articles were included, with health professionals at the forefront of care for people with COVID-19, in 14 health institutions in different geographic locations (Table 1).
Table 1 Characterization of the studies included in the sample. Brazil. 2020.
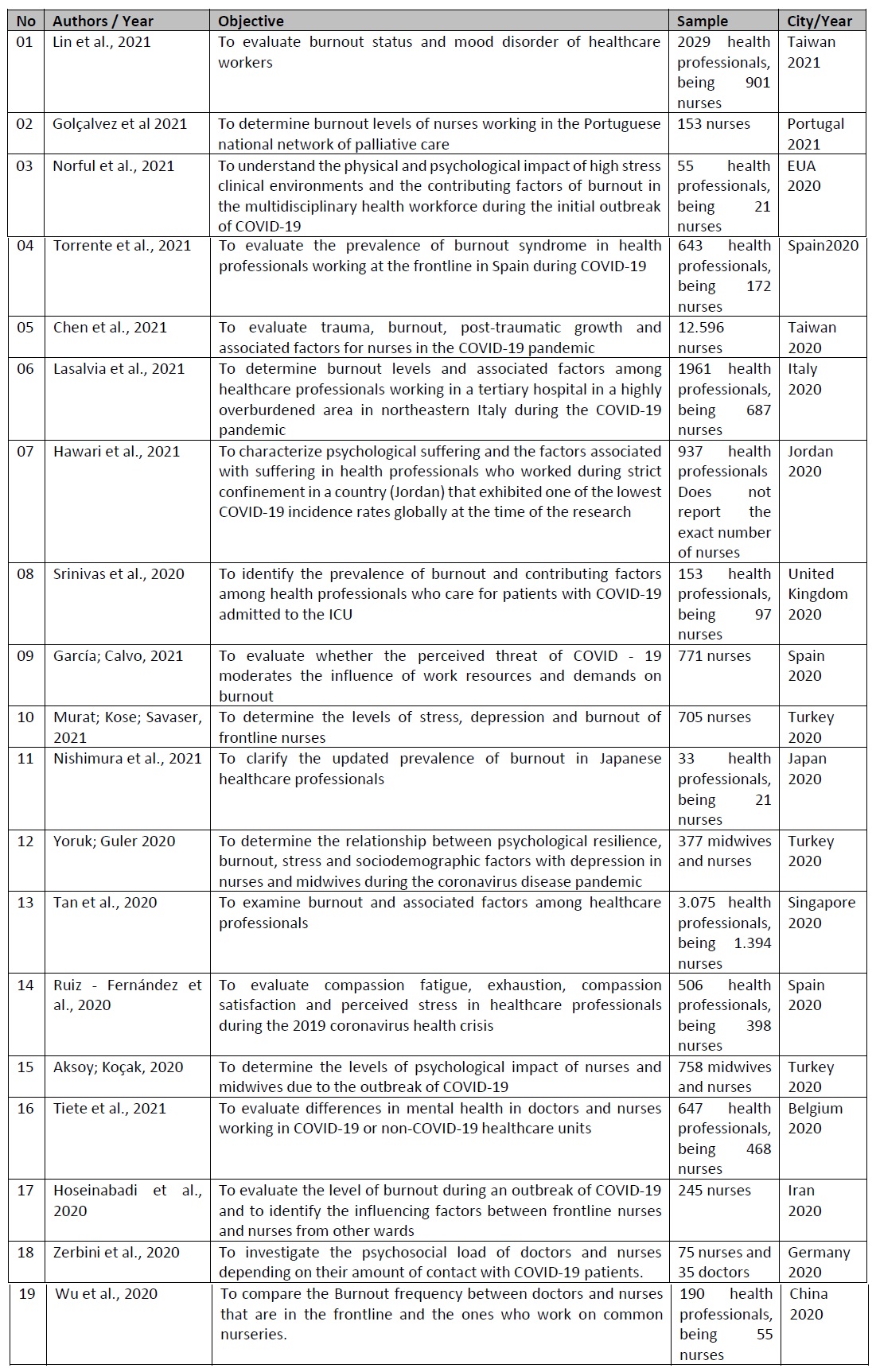
Source: Research data, 2021
The analysis of the results of this study allowed to identify of 10 constructs related to the three dimensions of burnout in nurses in the front line in the assistance to COVID-19 (Table 2). There was a greater identification of constructs in the emotional exhaustion dimension, with a predominance of emotional exhaustion, occupational stress, fear, anxiety, and occupational overload.
Table 2 Synthesis of the constructs related to Burnout Syndrome in nurses at the forefront in assisting COVID-19 and the articles that address each construct. Brazil. 2021
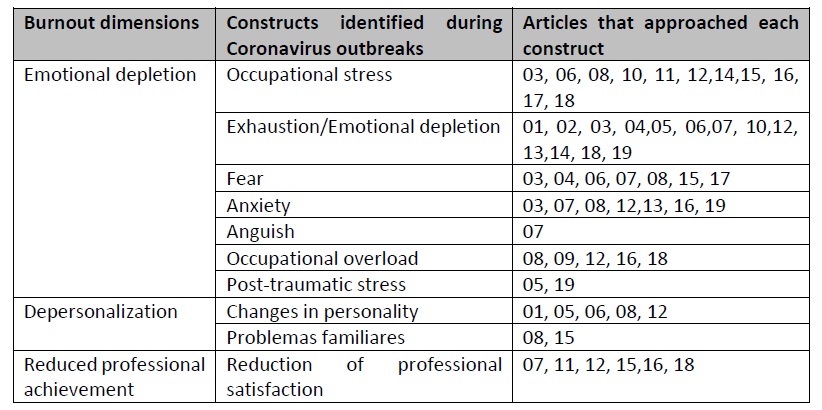
Source: Research data, 2021.
Consequences of Burnout syndrome on nurses that are in the frontline of Coronavirus
Emotional depletion
The nurses that are in the frontline of coronavirus experienced higher symptoms of emotional and physical deterioration. A frequent occurrence of fear and anxiety were observed, along with feelings of sadness and occupational stress due to the increase of the workload, morbidity, mortality, and unpredictable risks (Norful et al., 2021; Torrente et al., 2021).
The levels of emotional exhaustion seemed higher than the normative values and the percentage of nurses with high levels of exhaustion is significantly higher in the front line of care for people with COVID-19 than in other normal work situations (Zerbini et al., 2020; Chen et al., 2021). High levels of professionals with symptoms of post-traumatic stress disorders, anxiety disorders, depressive disorder, and emotional depletion were also identified (Wu et al., 2020; Chen et al., 2021). Emotional exhaustion related to nursing care for patients confirmed with the disease caused by COVID-19 was considered the biggest influence factor of burnout (Lasalvia et al., 2021; Hawari et al., 2021).
Depersonalization
The physical and emotional deterioration experienced by the nurses had an impact on their personalities. The findings have shown that there were low to elevated levels of depersonalization (Srinivas et al., 2020; Yoruk; Guler 2020). Due to the overload, the uncertainty in the work environment, and the threat of transmitting the disease, nurses changed their personality and lifestyle. There was a decrease in contact with patients and other health professionals, a fact that interfered in professional relationships and generated inadequate communication in decision making (Wu et al., 2020; Giusti et al., 2020).
Reduced professional achievement
There was an increase in the rate of job dissatisfaction due to emotional exhaustion in nursing care for patients with coronavirus. The reduction in job satisfaction was associated with lower levels of purpose and hope. In addition, they suffered from the possibility that their work environment could be a vector for transmitting the disease to friends and family (Tiete et al., 2021; Wu et al., 2020).
Discussion
The analysis of the studies included in this review highlighted the repercussion of the nurses that are acting in the frontline against coronavirus, in their productivity, work quality, and personal life, at which were identified constructs directly associated with the dimensions from the Burnout Syndrome.
Our results reported an agreement with other studies highlighting that nurses in direct contact with a patient infected by coronavirus are among the health professionals that showed the highest level of psychological charge (Zerbini et al., 2020; Matsuo et al., 2020). This data indicates that as a part of the hospital management planning during the outbreak of respiratory infection, an evaluation of the work conditions and mental health of the nurses must be made, with to ensure the quality of the care and occupational well-being (Kang et al., 2018).
For this purpose, it is vital to identify the constructs that can harm the mental health of nurses who are in the frontline and, consequently, the sizing of the nursing team and the quality of their assistance.
Studies report that acting on the frontline of COVID-19 had a negative impact on the mental and physical health of health professionals, in particular, nurses. In this study, 10 constructs related to the dimensions of Burnout Syndrome were identified, with predominance of constructs in the dimension of emotional exhaustion. The new health scenario imposed by the COVID-19 pandemic increased the workload, reduced downtime and several changes in their roles and responsibilities in a short time, in institutions in all countries of the world (Srinivas et al., 2020).
A consulted study explains that professionals who have direct contact with patients with COVID-19, especially those who require intensive care, tend to have a higher risk of occupational exhaustion and risk of burnout. To reduce the risk of burnout during this time of a pandemic, hospital administrations must recruit additional professionals in order to favor the dimensioning of frontline health professionals and reduce excessive workload, minimizing the risk of burnout (Lasalvia et al., 2020). It is worth clarifying that nurses with high levels of emotional deterioration can develop a mechanism of behavior defense which leads to depersonalization (Vieira et al., 2010). Study in Turkey showed that mean depersonalization scores were significantly higher and nurses, with high depression scores (Yoruk; Guler 2020). Consulted studies infer that emotional exhaustion resulting from nursing care to patients with COVID-19 can cause depersonalization, a factor of vulnerability to burnout (Hu et al., 2020; Hoseinabadi et al., 2020).
This mechanism represents the interpersonal aspect of the burnout syndrome, which represents a possible unconscious psychic shielding of nurses to avoid emotional involvement with patients in face of the severity of the disease (Silva et al., 2015).The depersonalization can lead the professionals to become indifferent to the needs of others, including the patients. This can compromise the quality and humanization of the care. In addition, the depersonalization of nurses can induce a reduction in interest in work, and generate professional dissatisfaction, which, over time, becomes vulnerable to burnout syndrome (Dalmolin et al., 2014; Schmidt et al., 2013).
In fact, studies have shown that there has been a reduction in the job satisfaction of nurses who were at the forefront of care during the pandemic (Nishimura et al., 2021; Yoruk; Guler 2020). Stress and professional exhaustion influence the dimension of achievement. This happens due to the feeling of being overwhelmed, the depression and anxiety imposed by this new health scenario (Nishimura et al., 2020). Corroborating these findings, a recent study on nursing performance identified lower levels of achievement related to work in wards for patients with COVID-19 compared to their colleagues in regular wards (Zerbini et al., 2020).
Studies suggest that professional satisfaction is a predictor of permanence in the job, motivation, and professional productivity. However, the level of job satisfaction of nursing staff is reduced around the world due to the current current pandemic (Hu et al., 2020; Zerbini et al., 2020; Aksoy; Koçak, 2020; Tiete et al., 2021). The main sources of professional dissatisfaction in nursing involve high care pressure before the increase in the number of hospitalizations, occupational overload and lack of professional recognition (Lu et al., 2012). Thus, it is important to recognize nurses' work as essential and create a favorable work environment. These efforts may positively influence the quality of care for patients with coronavirus.
In the studies presented in this review, there was unanimity in the risk of developing burnout among nursing professionals on the front line of the coronavirus. Despite different geographic regions, the prevalence of burnout was significantly higher among nurses with direct assistance to patients, mainly caused by constructs associated with the dimension of emotional exhaustion (Hu et al., 2020; Golçalvez et al 2021; Norful et al., 2021).
Such condition can be related to the fact that the symptoms of emotional exhaustion, depersonalization and reduced professional performance, characteristic of the burnout syndrome, appeared and intensified when nurses started to attend a greater number of patients, with an increased fear and anxiety of acquire the disease and transmit it to family members.
Our findings highlight the importance of organizational support to nurses in the front line of COVID-19. Health administrators must implement strategies to mitigate the negative results of emotional exhaustion, depersonalization and reduced job satisfaction, in addition to addressing other psychosocial concerns of nurses and the working conditions they face in this new moment of crisis.
Predicting and identifying adverse factors, such as stressors in a crisis situation, may permeate the early implementation of interventions, in order to reduce/neutralize the development of Burnout Syndrome in nurses.
A limitation is the absence of investigations covering all countries affected by COVID-19, which prevents the generalization of the results. It is hoped that further studies can be conducted, with nurses from various geographical locations, especially in the west and underdeveloped countries such as Brazil, in which the findings can be even more worrying.
Conclusion
The constructs that trigger the burnout syndrome in nursing professionals working on the front line to COVID-19 are occupational stress, emotional exhaustion, fear, anxiety, anguish, occupational overload, post-traumatic stress, changes in personality, family problems and reduction professional satisfaction.
Implications for clinical practice
The prevention of burnout syndrome is a necessity when the health system is in a critical situation, as observed in the current health scenario. Thus, when identifying the constructs that trigger burnout in nurses in the front line of COVID-19, the study exposes the need for prevention and control interventions as a priority in health institutions, regardless of geographic location, in addition to better working conditions, Adequate PPE and support services for counseling