INTRODUCTION
The first coronavirus disease (COVID-19) cases, caused by SARS-CoV-2 infection, occurred in the city of Wuhan, China, in December 2019. Since then, rapid viral spread has led to a pandemic in a few months.1 There are several reports about COVID-19 pulmonary and extrapulmonary manifestations and every day more is discovered about the pathophysiological mechanisms. In which concerns dermatological aspects, several reports associate cutaneous manifestations with the suspicion of infection, while the reports with laboratory confirmed cases are limited. One of the biggest controversies about these manifestations is about the culprit: is it a direct reaction to viral infection or a drug-induced hypersensitivity?
To date, some review studies have been published with the aim of synthesizing dermatological findings in COVID-19. However, there are no studies that quantify the skin disorders prevalence and characteristics. Therefore, the objective of this meta-analysis is to summarize and evaluate the skin disorders characteristics that are being reported in patients with a COVID-19 confirmed diagnosis.
METHODS
This meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations. A review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) under identification CRD42020213921.
The ethical board approval was not necessary because it is a literature review study.
Data sources and search strategy
Searches for articles were carried out on PubMed, SciELO and ScienceDirect from 01/01/2020 to 09/28/2020. The search strategy used was: (“COVID-19” OR “novel coronavirus” OR “SARS-CoV-2”) AND (“skin” OR “dermatologic” OR “dermatosis” OR “cutaneous”). The search was done using the field tag “[tw]” in each word in PubMed. There was no language restriction.
Study Section
All studies found should include the following criteria to be considered in this work: (a) Study design: observational studies (cross-sectional, cohort and case-control), research letters, case report or case series; (b) Participants: laboratory-confirmed COVID-19 with cutaneous manifestations; (c) variables for observational studies: cutaneous manifestation classification and frequency; (d) variables for case report or case series: age, sex, cutaneous manifestation and topography. Comments and review articles were excluded.
Two independent authors (KOR, VVZ) evaluated the titles and abstracts of all identified articles. Full articles were obtained when the titles and abstracts met the eligibility criteria or when they did not provide enough information for decision making. Inclusion was carried out after the texts had been completely read. Controversial decisions between authors were reviewed and resolved in a third author (LML) presence.
Data extraction
One author (KOR) extracted the information using two standard tables, one for observational studies and the other for case reports. These data were evaluated by (LML). The extracted data are: (a) Study identification: first author, publication year, country. (b) study design and participants; (c) variables: age, sex, cutaneous manifestation, length, latency, topography, signs and symptoms, laboratory findings, prognosis.
risk of publication bias
Two independent authors (KOR, VVZ) evaluated studies quality and risk of bias using the National Institutes of Health Study Quality Assessment Tools for observational designs and case reports. (Supplementary Table 1.1 and 1.2)
Data synthesis and statistical analysis
The data generated from observational studies and case reports were analyzed in different ways. To assess the case reports, in the dichotomous variables, the association inference was made by the appropriate chi-square test (Pearson or Fisher). The continuous variables normality was assessed by the Shapiro-Wilk test. Difference inferences between continuous variables were made using the T test or the Mann-Whitney test. These assessments were conducted using the
IBM SPSS Statistics v22 software.
To assess observational studies, the weighted mean prevalence and 95% CI was calculated when there were at least three studies for a given dichotomous variable. This evaluation used the Random-effects model with the DerSimonian and Laird (DL) method and normalization in logit. The studies heterogeneity was measured using the I2 values, which measure the studies total variation percentage. Heterogeneity is considered substantial when I2> 50%. The publication bias was subjectively assessed using funnel plot (Supplementary Table 2.1). Egger’s test was not used because there were no more than 10 studies for each variable. These assessments were made using the R language with the metafor 2.4-0 library.
A type I error of 5% was considered for all analyzes.
RESULTS
In the three databases, 551 articles were identified. After removing the duplicate articles, the titles and abstract of 418 articles were evaluated by the eligibility criteria. The excluded works totaled 333, being classified as irrelevant to the
theme (n=247), review articles (n=54), perspectives (n=21), guidelines (n=8) and sample overlap (n=2). After the screening, 65 case series and case reports and 19 observational studies remained. After reading these works in full, 27 case/ series reports were excluded because they deal with only suspected, but not confirmed, patients with COVID-19. Thirteen observational studies were excluded because they deal with a population specific to a disease (n=10) or due to insufficient information (n=3). Finally, the eligible studies totaled 38 for case/series reports and 6 for observational studies.
The case/series reports resulted in 87 individuals and the observational studies resulted in 363 individuals with confirmed COVID-19 and with cutaneous manifestation (Fig. 1).
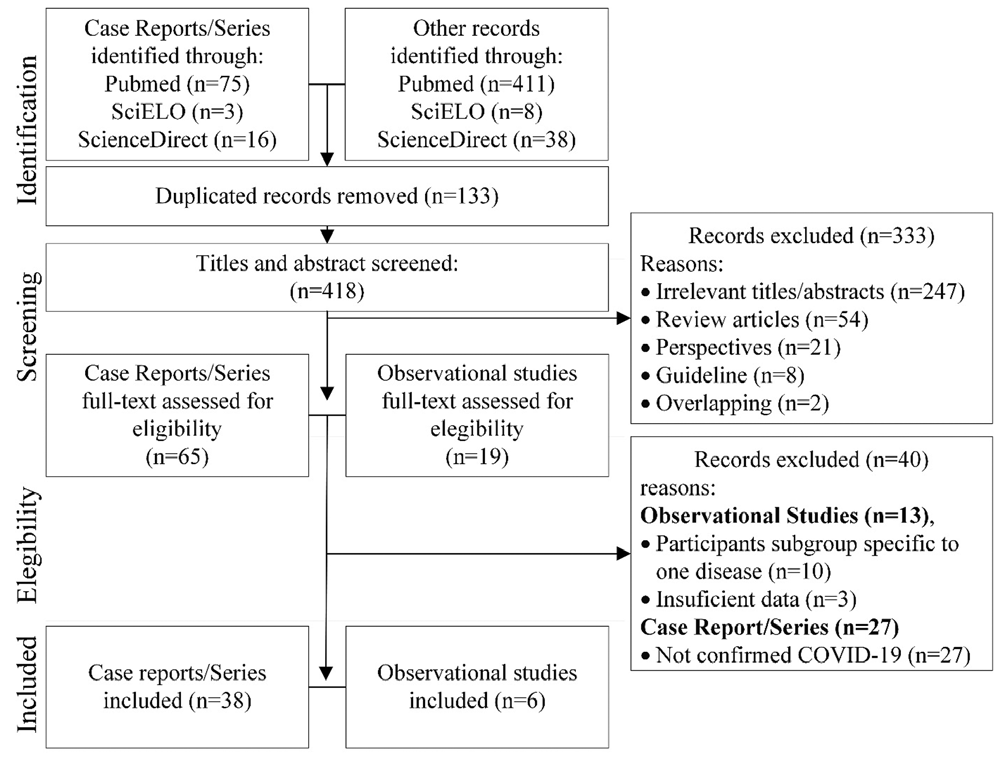
Figure 1 PRISMA diagram describing the selection process. SciELO, Scientific Eletronic Library Online.
Demographic
The case/series reports have patients from 22 countries: Italy (27.6%), Russia (16.1%), USA (13.8%), France (5.7%), Japan (4.6%), Iran (3.4%), Egypt (3.4 %), Romania (3.4%), Spain (3.4%), Tunisia (2.3%), Belgium (2.3%), United Kingdom
(2.3%), India (1.1%), Morocco (1.1%), Paris (1.1%), Saudi Arabia (1.1%), Iraq (1.1%), Brazil (1.1%), Greece (1.1%), Paraguay (1.1%), Portugal (1.1%), Wales (1.1%).
Observational studies have patients from 5 countries: Spain (66.4%), Turkey (14.3%), China (14.3%), India (3.6%), Jordan (1.4%) (Fig. 2).
Men frequency was higher in both study designs. In case reports and observational studies, men represent 56.3% and 65.6% of the sample, respectively. In the case reports, the median age reported was 54 (32 - 66) years in the general
sample; 57 (25.5 - 69.5) years in men; 50 (33.5 - 62.5) years in women (Fig. 2).

Figure 2 Case/series reports characteristics frequency distribution. (a) age frequency, (b) continental frequency, (c) skin disorder duration until remission or hospital discharge, (d) skin disorder latency relative to the first general manifestations (e.g. fever, dyspnea). Q1: first quartile; Q3: third quartile.
Skin manifestations
Eleven types of skin disorders in COVID-19 confirmed patients are described: papulovesicular, maculopapular, purpuric, urticarial, erythema multiforme, livedoid, chilblain-like, zosteriform, bullous, papulosquamous, erythoderma.
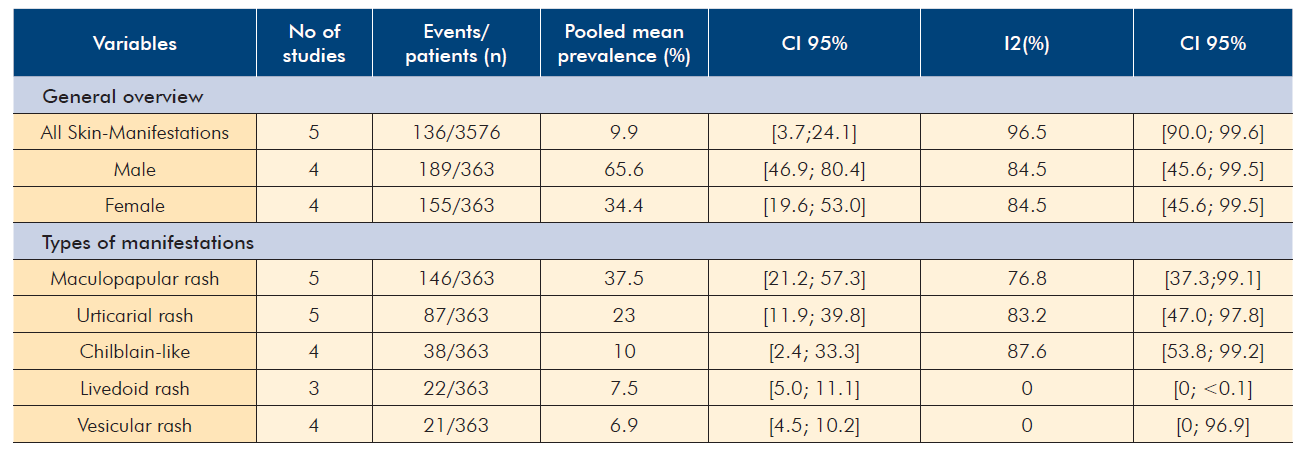
These disorders frequencies, found in the case reports, are described in Table 1. The prevalences estimated by observational studies are described in Table 2. In the assessment of case reports, female patients are associated with a greater maculopapular rash description (p=0.015). Other cutaneous descriptions were not associated with sex. Cases described with chilblain-like lesions are associated with age below 20 years (p=0.002).
Table 1 Sex, skin manifestation, symptoms, topography and laboratory markers frequency described in 87 cases.
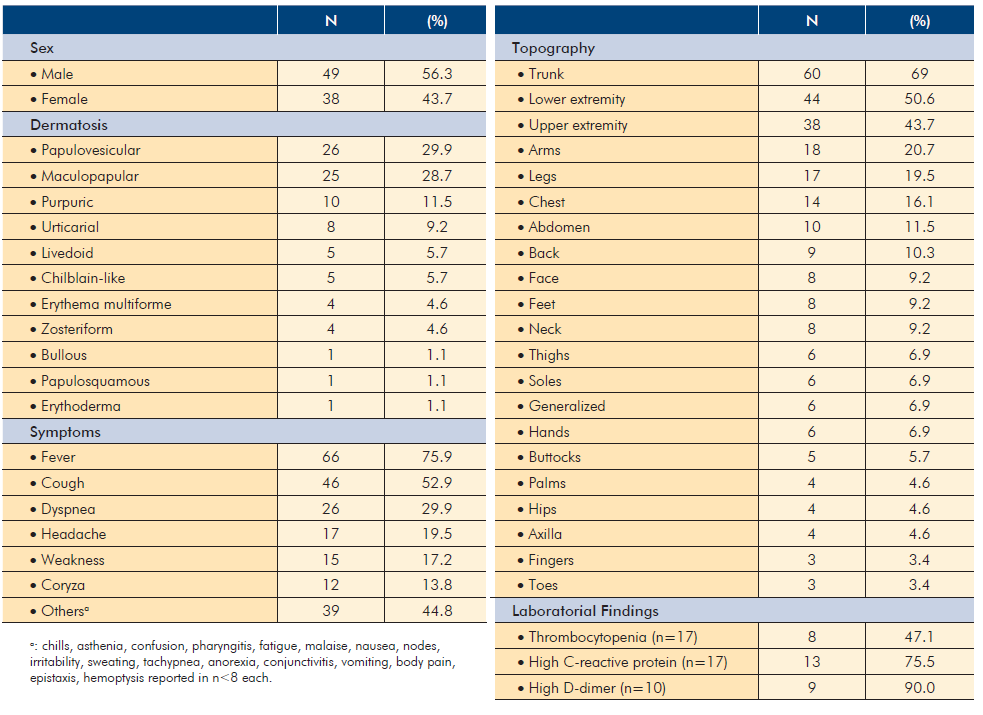
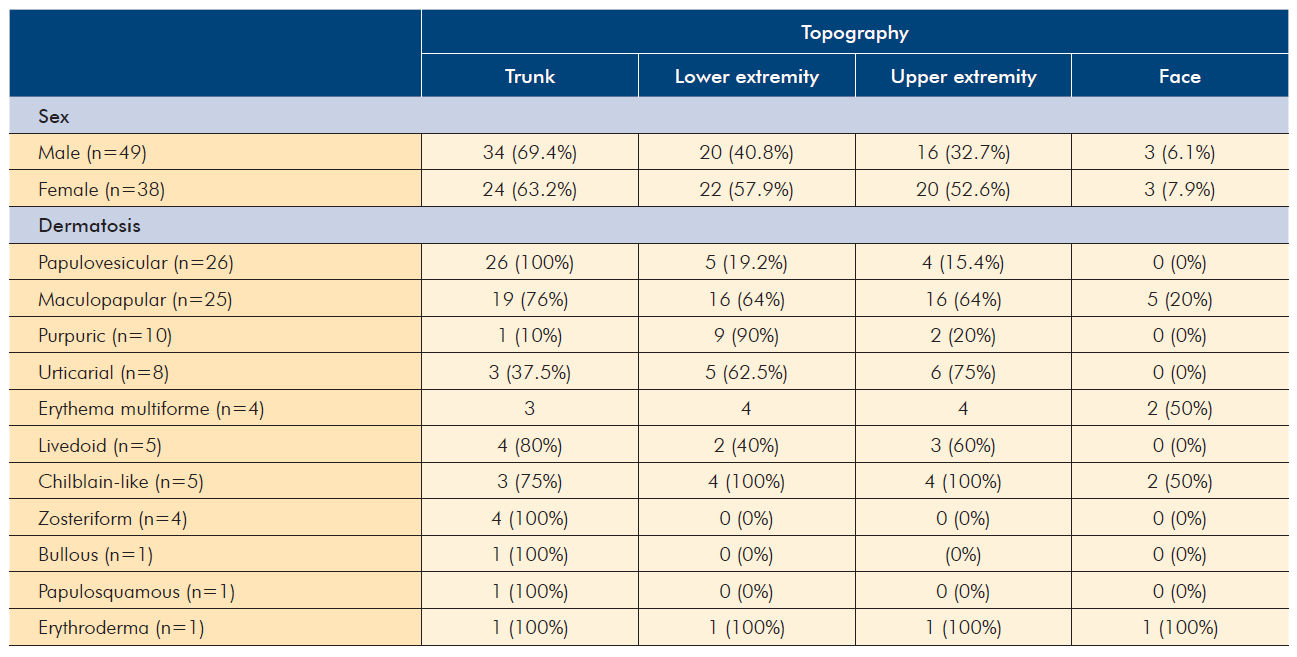
Topography
The topography most reported was in the trunk, described in 69% of the cases. Generalized involvement accounted for 7% of cases. Injuries to the palms or soles are described in 9% of cases. There was no sex association with facial, trunk, upper or lower extremities lesions. Upper extremity involvement was associated with maculopapular rash reports (p=0.015). The purpuric rash reports were associated with lower extremity topography (p=0.015). Papulovesicular rash reports were associated with trunk topography (p<0.001).
General symptoms
Thirty-one distinct signs and symptoms are described. The ten most frequent are shown in table 1. Symptoms frequency due skin disorder is shown in Table 3. Chilblain-like reports was associated with the non-description of fever (p=0.011).
Maculopapular rash was associated with the non-description of dyspnea (p=0.021). Papulovesicular rash was associated with pruritus (p=0.014), fever (p=0.004) and airway symptoms (i.e. dyspnea, cough or coryza) (p=0.001) description.
Other skin disorders were not associated with fever or airway symptoms description. Sex was not associated with general symptoms.
Duration and latency
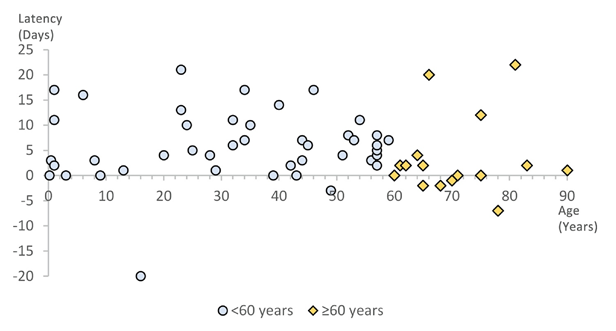
The skin disorder duration was quantified in 23 cases. The median was 8 (7 - 14) days until remission or hospital discharge. There was no association between the disorder type and its duration over 5 or 8 days. Latency for the skin disorder appearance was reported in 60 cases. The median was 4 (1 - 9.5) days (Fig. 2).
Papulovesicular rash was associated with latency less than 6 days (p=0.016). Maculopapular rash was associated with latency greater than or equal to 8 days (p=0.043).
Other skin disorders were not associated with latency greater than or equal to 2, 4, 6 or 8 days. Latency and duration did not differ statistically between sexes or ages between 20 and 40 years. Latency was significantly lower in patients over 60 years old (p=0.041) (Fig. 3).
For each skin disorder, the mean latency was: 3.65 ± 3.71 days for papulovesicular rash (n=20); 7.8 ± 7.47 days for maculopapular rash (n=20); 6.17 ± 8.35 days for urticarial rash (n=6); 10.25 ± 7.50 days for purpuric rash (n=4).
Laboratorial findings
Laboratory descriptions were poor in the cases reported. Low hemoglobin values (n=5; 6%), lymphopenia (n=11; 13%), lymphocytosis (n=0), low platelets (n=8; 9%), high C-reactive protein (CRP; n=13; 15%), high d-dimer (n=9; 10%). Skin disorders were not associated with anemia, thrombocytopenia and increased values of C-reactive protein and d-dimer.
DISCUSSION
The advantage of studying two different study designs, observational and case/series reports, is to approach the same theme from different perspectives. The prevalence estimate was made possible by the observational studies evaluation.
This is not possible only by evaluating case/series reports, as there is no methodological control in this study design. However, case/series reports are sufficient to detail morbid aspects, allowing intrinsic inferences in each morbidity, dealing with strictly independent cases.
The high heterogeneity found in the prevalence analysis is expected. Immunity and responsiveness to an infection depends on several factors, such as sociodemographic, nutritional, genetic, age and morbid history.2 Cutaneous manifestations vary according to individual characteristics, however, there are reports of individuals from the same family who manifested similar disorders while in isolation at home.3 This suggests that the COVID-19 cutaneous presentation may not be a random phenomenon, but a pattern may exist. One way to reduce the observations heterogeneity between studies is to work with specific subgroups. However, it was not possible to extract these data from observational studies eligible for this work.
The skin disorders pooled mean prevalence in patients with COVID-19 positive diagnosis is 9.9% (95% CI: 3.7-24.1).
Only five skin manifestations had a concomitant presentation in at least three observational studies. The most prevalent was maculopapular rash (37.5%; 95% CI: 21%-57%). In parallel with the evaluation of the case/series reports, the maculopapular rash is one of the most published to date.
The demographic distribution has an aspect of scientific bias. To date, the countries that lead the COVID-19 confirmed cases are USA (7 499 341 cases), India (6 757 131 cases) and Brazil (4 969 141 cases). However, they are the least representative countries in this sample. This may reflect a low incentive to conduct research and scientific reports.
The most prevalent skin disorder was maculopapular rash (37.5%; 95% CI: 21%-57%). This finding is coherent, as this rash is the most common among viral infections or drug-induced non-immediate hypersensitivity reaction.4 In the case/series reports, there was an association with females (p=0.015), no description of dyspnea (p=0.021), upper limbs topography (p=0.015) and described latency greater than 8 days (p=0.026). It was described as a rash with confluent erythematous macules and papules, which acquired a pale color under pressure (blanchable). The average age was 43.3 ± 28.2 and four cases (16%) reported pruritus.
Despite being the most frequent rash on upper limbs (42%), it was described on the trunk, lower limbs and face in 74%, 65% and 17% of cases, respectively. It was generalized in 16% of cases. The description of fever was common during the rash manifestation,5 but in some cases the rash manifested without fever6 or after the end of the feverish period.7
Many cases did not report rash duration, as some patients were discharged before complete remission of the condition.
The average duration presented in 12 cases is 9.0 ± 4.5 days. When specified, treatments varied with the use of systemic or topical corticosteroids or/and intravenous or oral antihistamines.5,8-10
There is a hypothesis that some skin disorders associated with COVID-19 may be a drug-induced reaction. Maculopapular rash is one of the main manifestations of non-immediate hypersensitivity to drugs.11,12There are some histological features that help to identify and guide the etiology. In cases of hypersensitivity, maculopapular rash tends to present superficial lymphocytic infiltrate, containing eosinophils and, sometimes, neutrophils; basal vasculopathy and little or no spread of lymphocytes in the dermal papilla or epidermis.12
However, some reports present histopathology with dense lymphocytic infiltrate in the dermal papilla and perivascular, as well as the absence of eosinophils, which is an atypical drug-induced reaction finding.8,10Other reports dismiss this hypothesis due to clinical history, since the rash manifested itself before any drug use.13 Other reports of skin disorders have also ruled out the drug-induced reaction hypothesis.14,15
In four cases, they are described as erythema multiforme-like, with a circular maculopapular aspect in the shape of a target. Erythema multiforme, in a general context, has less than 1% prevalence and is typically more common in women in 1.5:1 ratio. Precipitating factor is related to an infection in 90% of cases.16 In evaluated reports, fever and pain were described in two (50%) and one (25%) cases, respectively. Pruritus has not been described. The distribution was uniform in upper and lower extremity and trunk. Generalized involvement occurred in two (50%) cases. Three (75%) cases are female. Purpuric rash was described as those that did not acquire a pale color under pressure (non-blanchable). It is related to inflammation of small vessels in the dermis and blood leakage.12 In ten cases, there was an association with lower extremities presentation (p=0.015), described in 90% of the cases. Six cases reported platelet values, only one (17%) reported thrombocytopenia. Histopathological evaluation in three patients without previous comorbidities describes little inflammatory infiltrate, fibrin thrombus and vessel wall complement deposition.15,17Some purpuric lesions are more frequently related to lower extremities, especially in the absence of thrombocytopenia. Venous hypertension and blood stasis, associated with capillary fragility, can be cofactors for this clinical condition.18
Papuloveiscular rash has been described as a varicella-like rash, with vesicles forming on a papulo-erythematous base, which leads to superficial erosions upon rupture. Pruritus was associated with this rash presentation (p=0.014),
which is frequent in 38% of cases. No pustules were described and the liquid eliminated was described as translucent.
These cases were also associated with fever (p=0.004) in 96% of the cases and airway symptoms (p=0.001) in 85% of the cases. All cases involved trunk. In most cases, vesicles appeared during the fever episode, with an average latency of 3.7 days, ranging from -2 to 13 days.19 Histological reports have admitted features consistent with a viral rash.14
Chilblain-like lesions description was associated with age under 20 years old (p=0.002). These lesions are described as erythematous or violaceous, edematous and painful in the acral region. There was no association with description of fever (p=0.011). Pain and pruritus were described in 40% and 20% of cases, respectively. Male sex represents 80% of cases. Kerber et al raises a hypothesis that this condition may be a COVID-19 late manifestation. Two cases have positive SARS-CoV-2 IgG and negative SARS-CoV-2-IgM values, with no recent clinical comorbidities.20,21During this study eligibility process, some cases of chilblain-like were discarded because they did not present a positive COVID-19 laboratory diagnosis. Considering the hypothesis of latent manifestation, it is prudent, in the future, to conduct investigations about these manifestations in COVID-19 suspected cases.
Urticarias were defined as erythematous plaques or papules with irregular contours. Female sex represents 62.5% of the cases. Fever and pruritus were described in 75% and 37.5% of cases, respectively. There was no description of pain. Upper extremities were the most affected (75% of cases). Management included the use of antihistamines and corticosteroids which were associated with a good lesional remission.22-24The average latency was 6.2 ± 8.4 days. Full symptoms duration has not been quantified, only reported as gradual improvement. In two cases existence of previous atopy or allergy clinical history that might justify the lesions was denied.22,25
According to the Centers for Disease Control and Prevention (CDC, 2020), fever, cough and dyspnea are the most common COVID-19 symptoms.26 Symptoms distribution found in the case/series reports are coherent. Fever, cough and dyspnea were reported in 76%, 53% and 30% of cases, respectively. From the first fever or airway manifestation, the cutaneous signs appeared in a median of 4 (1 - 9.5) days.
Unfortunately, sixty-four (74%) cases were not sufficient to report the skin disorder duration. In some cases, hospital discharge was made before complete resolution. In others, clinical remission was quantified (e.g. “in a few days”). There is a hypothesis that the use of corticosteroids and antihistamines are sufficient to improve COVID-19 skin manifestations.
However, due to lack of data related to duration and treatment, it was not possible to stratify the sample and perform the appropriate hypothesis test.
The median latency between skin disorder onset and first general symptoms (e.g. fever, dyspnea, coryza) was significantly lower in patients over 60 years old (p=0.041). The immune system natural degeneration by age is a factor that reflects changes in innate and adaptive responses, as well as susceptibility and manifestation to infectious diseases. Aging process, by itself, results in altering the balance of inflammatory and anti-inflammatory mediators by the greater oxidative process and cellular apoptosis. The result is an immune remodeling with increased pro-inflammatory mediators production.27 It is possible that age increases COVID-19 skin disorders susceptibility. The average latency in individuals younger (n=45) and older (n=15) than 60 years was 5 (2 - 10) and 2 (-1 - 4) days, respectively.
This study has several limitations. As most of the observations were conducted in Europe and Asia, care must be taken when generalizing these results to the whole world. Few observational studies have been included, which considerably increases the confidence interval of the results. The case/ series reports have low or very low level of evidence and many did not follow the Case Reports Guideline (CARE) methodological rigor. The funnel plots evaluation showed substantial publication bias (publication bias), represented by the asymmetry of the points. We recognize, however, that may be some studies, published in local non-indexed journals, were not included in this study.
CONCLUSION
In conclusion, skin disorders prevalence in COVID-19 laboratory- confirmed patients is around 10%. Each cutaneous manifestation presented different peculiarities in the case/series reports evaluation. Maculopapular rash is the most prevalent manifestation and its description is associated with upper extremities topography and latency over 8 days. Purpuric rash description is associated with lower extremities topography. Papulovesicular rash is associated with pruritus, fever and airway symptoms. Chilblain-like lesions are associated with age under 20 years and absence of recent signs and symptoms. The median overall latency was 8 days.
Individuals over 60 years of age had a significantly lower median latency. Fever, cough and dyspnea are the most described signs and symptoms. There are no reports of specific skin manifestations. So far, there is no approved COVID-19 treatment and the infection and skin disorders relationship as cause and effect is still unclear.