Introduction
Skin diseases have a high prevalence and incidence in hospital settings, regardless of the primary causes of hospitalization. Skin lesions may occur because of inherent skin conditions, cutaneous manifestations of systemic illnesses, or even as a result of hospital care procedures. 1,2Skin disorders in hospital settings encompass a heterogeneous group of conditions with variable severity, including urticaria, angioedema, viral and bacterial infections and autoimmune diseases, 3 among others. In patients with non-dermatological illnesses who develop skin conditions during their hospital stay present a higher risk of mortality than individuals without associated skin disorders, which highlights the importance of early diagnosis and treatment of these conditions. 4 Besides, during hospitalization, bed confinement, frequent exposure to antiseptics and dressings, catheter punctures and other factors may lead to the development of contact dermatitis, decubitus ulcers, or skin infections due to the rupture of skin integrity. 5 Although in most cases the Dermatology service is not directly responsible for these patients, its staff is often tasked with establishing the initial dermatological diagnosis and management of skin conditions. 6,7Therefore, it is essential to evaluate the most prevalent skin conditions in inpatients, as well as the role of Dermatology in their care, either as an assisting team or as medical consultants. 8,9To contribute in this scenario, this study presents a systematic literature review aimed at analysing the impact of dermatological diseases in hospital care.
Methods
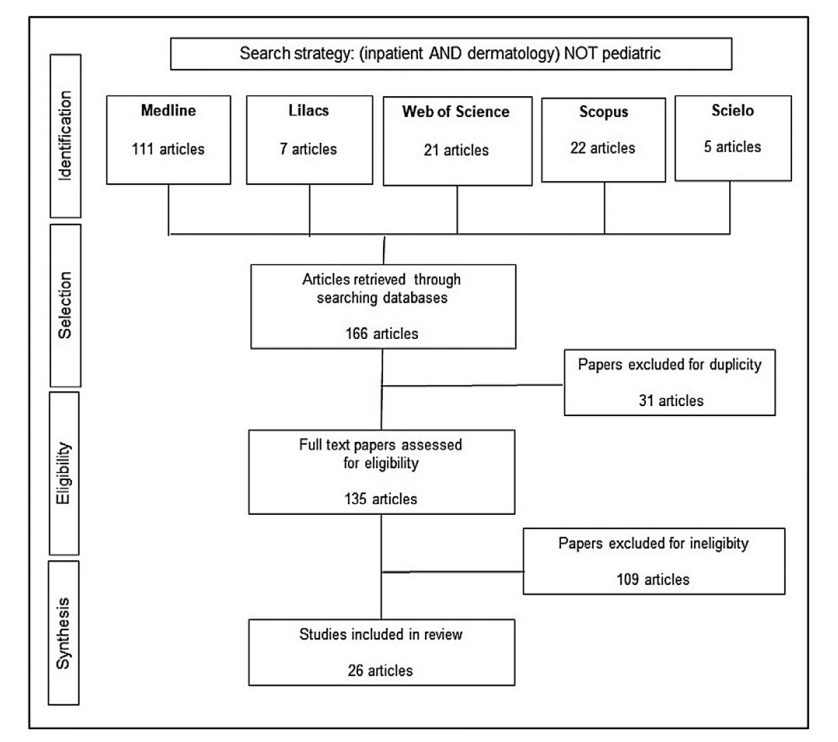
This study consisted of a systematic literature search and a narrative review about skin diseases in hospital settings, discussing and analysing these findings and the contribution of Dermatology. The systematic review process searched five databases: Medline (Medical Literature Analysis and Retrieval System Online), SciELO (Scientific Eletronic Library Online), LILACS (Latin-American and Caribbean Literature on Health Sciences), Web of Science and Scopus (SciVerse Scopus Elsevier). It was registered in the PROSPERO (International prospective register of systematic reviews) database under the register number CRD42020180078. The search strategy used as keywords: (“Inpatients” AND “Dermatology”) AND NOT “Paediatric”. The exclusion of the term “Paediatric” was established in order to avoid confusion bias, since the epidemiological profile in children and teenagers (i.e., under 18 years of age) differs from that of the adult population. We selected articles published in the past ten years, from January 2010 to January 2020, adopting the terms “human”, “full text” and “ten years” as search filters. Amongst the search strategy results, we selected studies using as inclusion criteria: studies about prevalence and incidence of dermatoses and dermatological lesions in hospital environments, and studies on patients under dermatology team care, either in direct patient assistance or as consultants to assistant team. The exclusion criteria were articles about prevalence and/or incidence of specific skin diseases, articles about outpatient care, as well as studies on a paediatric population.
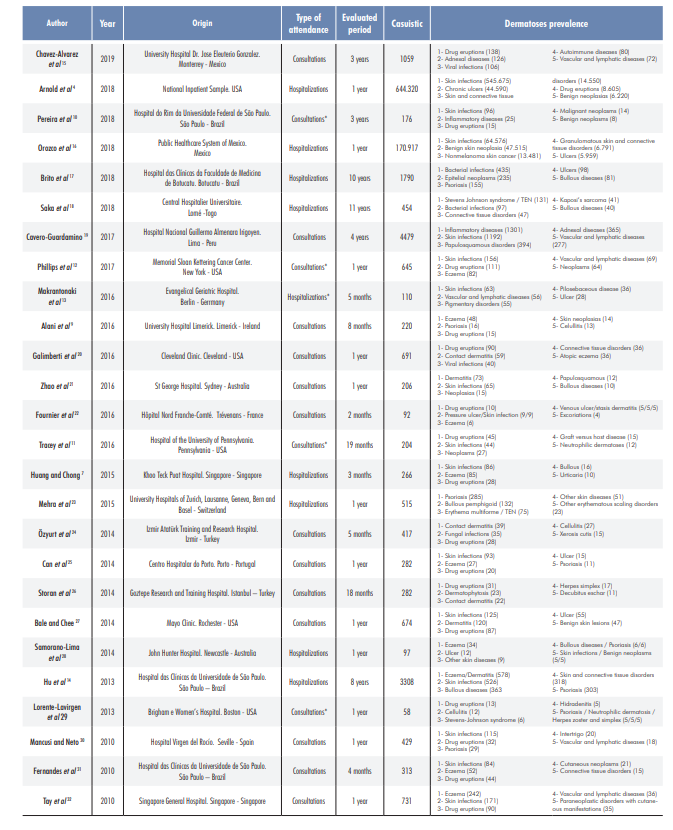
Selected articles were analysed by two independent evaluators who verified data such as hospital of origin, nature of hospital dermatology evaluations, casuistic of patients, duration of the investigations, and the most prevalent dermatoses identified by these studies. Due to them heterogeneity of the evaluated data, which included diverse population characteristics and different research durations, the data synthesis was performed by grouping the most prevalent diagnoses into classes of dermatoses.
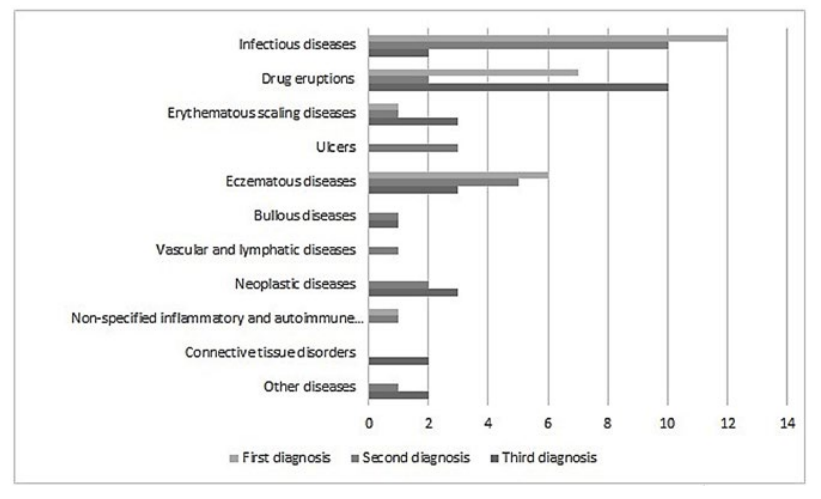
From this strategy, we analysed the five main diagnoses reported by each study, which were ranked based on their epidemiology frequencies (incidence or prevalence). Then the most prevalent/incident skin diseases were summarized in 11 categories: “infectious skin diseases”, “drug reactions”, “erythematous scaling diseases”, “ulcers”, “bullous diseases”, “eczematous disorders”, “neoplastic diseases”, “vascular and lymphatic diseases”, “non- specified inflammatory diseases”, “connective tissue disorders” and “other dermatological diseases”. Then, these dermatological disease groups were organized from the most frequent disease groups to the least frequent ones, thus summarizing the frequencies of hospital dermatoses.
The narrative review was conducted through the authors’ selection of relevant references about hospital dermatology, including review articles, books and other publications. From these findings, we proposed an analysis of the contributions of Dermatology in hospital settings and its challenges to meet health care systems’ needs.
Results
Based on the systematic review strategy, we found 166 publications in databases, and 31 articles were excluded due to duplication. From the 135 eligible studies, we excluded articles that did not meet the established criteria, that is, those which included the paediatric population, outpatient care, and prevalence of particular skin diseases (Fig. 1). From this perspective, 26 studies were included, and we analysed the prevalence and/or incidence of dermatoses among inpatients and the types of dermatological assistance: dermatological consultancy or dermatological care.
Regarding article profile, we observed that most studies were published in the International Journal of Dermatology (six publications) and Actas Dermo-Sifilográficas (three publications) and were written either in English (21 articles), Spanish (three articles) or French (two articles). Moreover, most articles were published in 2014 (five publications), 2016 (six publications) and 2018 (five publications) - (Table 1). Regarding types of medical care, nine studies explored dermatoses based on inpatient diagnosis, while seventeen publications evaluated Hospital dermatology consultations (Table 1). Five publications included particular contexts, such as specific populations - kidney- transplanted patients, 10 patients with hematologic malignant neoplasms, 11 oncological patients 12 and elderly people 13 and a female hospital. 14
Concerning prevalence and incidence, there was a predominance of “skin infections”. They were the most frequent group of dermatoses in 12 publications and the second most prevalent one in 9 other studies. Bacterial, fungal and viral infections were also frequently reported singly in many publications, with herpes simplex and herpes zoster, cellulitis and dermatophytosis at the top.
“Drug eruptions” were presented as the most prevalent or incident skin conditions in seven studies, and as the third most prevalent ones in ten other publications, with an emphasis on Stevens-Johnson syndrome in some papers. It is also noteworthy that “eczematous diseases” were frequently reported among the main dermatoses, being the most prevalent in six articles and second most prevalent in six other studies. Cutaneous ulcers, benign and malignant skin neoplastic conditions and erythematous scaling diseases were also presented with significant frequencies in most studies (Fig. 2 and Table 2).
Table 2: Ranking of the most frequent skin disease groups according to included studies’ frequencies.
| Skin diseases groups | Diagnoses ranking* | ||||
| 1º | 2º | 3º | 4º | 5º | |
| Infectious diseases | 12 | 10 | 2 | 3 | 3 |
| Drug eruptions | 7 | 2 | 10 | 1 | 0 |
| Erythematous scaling diseases | 1 | 1 | 3 | 1 | 3 |
| Ulcers | 0 | 3 | 0 | 3 | 3 |
| Bullous diseases | 0 | 1 | 1 | 2 | 3 |
| Eczematous diseases | 6 | 5 | 3 | 0 | 3 |
| Neoplastic diseases | 0 | 2 | 3 | 4 | 3 |
| Vascular and lymphatic diseases | 0 | 1 | 0 | 3 | 3 |
| Non-specified inflammatory and autoimmune diseases | 1 | 1 | 0 | 1 | 0 |
| Connective tissue disorders | 0 | 0 | 2 | 3 | 1 |
| Other diseases | 0 | 1 | 2 | 6 | 3 |
* Ranking based on frequencies of skin diseases as reported by included studies
Discussion
The impact of skin diseases in hospital settings Skin diseases are one of the main elements in the global burden of disease, affecting millions of people all over the world, with an estimated prevalence ranging from 15% to 20% in the general population. 9,33From this perspective, it is evident that inpatients are likely to exhibit several skin conditions, even though they are not the primary cause of hospitalization. 9
The hospital setting increases patient vulnerability, either due to the inherent risks of their primary disease(s) or because of hospital-related conditions - invasive procedures and prolonged decubitus, for example. In this scenario, acute skin diseases represent a potential life-threatening risk, considering their systemic repercussions or impact on patients’ general clinical condition. Moreover, critical and immunocompromised patients have demonstrated higher skin vulnerability to external damage, and therefore face an increased risk of infection and atypical signs and symptoms. 1,2,8
Furthermore, hospital dermatoses can also be potentially life-threatening, due to both the risk of systemic impairment and associated complications 1,6,19A study about hospitalizations in the United States identified dermatological diseases as responsible for 0.47% of hospital mortality in primary dermatological conditions, and 3.29% of mortality as hospital complications associated with other underlying diseases. 4 Regarding the causes of hospitalization, a study on Mexican health services 16 reported that 40% of the deaths associated with skin diseases were caused by cutaneous infections. Such finding is consistent with the results found by Arnold et al, 4 who established bacterial infections as the cause of 51% of skin disease-related deaths. Skin infections are highly frequent in both community (outpatient) and hospital settings, where they appear as complications of community diseases as well as due to hospitalization conditions: invasive procedures and chronic diseases decompensation. 16,30
During hospitalization, skin infectious diseases may present as abscesses, furuncles, impetigo, erysipelas, cellulitis, among others. 16 According to Arnold et al, 4 several factors contribute to increasing skin infectious diseases in hospitals, including: multidrug resistant pathogens, ageing population and higher prevalence of comorbidities among inpatients. Besides, skin infections constitute a considerable risk factor for sepsis and mortality. Drug eruptions have shown a wide prevalence and/or incidence in the publications, which could be related to the variety and number of drugs used during hospitalization. Analgesics, non-steroidal anti-inflammatory drugs, and neuroleptics are among the main drug classes associated with skin eruptions. Tay et al 32 highlighted the importance of dermatologists in early diagnosis in these cases, remarking that only half of the drug eruptions were initially recognized by non-dermatology medical teams.
Erythematous scaling diseases - mainly represented by psoriasis - revealed a prevalence below the expected: only one paper 23pointed psoriasis as the most prevalent dermatosis. Traditionally, severe psoriasis is an important cause of hospitalization in Dermatology. However, these results might be explained by the introduction of immunobiological drugs in the past few years, which contributed to a more effective control of psoriasis cases, avoiding hospitalization. 27
Skin ulcers were also among the most frequent conditions, being mentioned among the five main diagnoses in one third of the articles. Besid es the causes inherent to hospitalization, such as prolonged decubitus and the use of dressings, ulcers represent a challenging diagnosis, with a wide range of differential diagnoses: venous and arterial ulcers, pressure ulcers, vasculitis and other infectious processes. 8 Regarding the countries of origin of these studies, we have found no specific tendencies. For example, infections are frequent both in more economically developed countries - United States, 4,12Germany, 13 Portugal 31 and Spain 29 - and in developing countries - Brasil 10,30and Mexico. 16 Therefore, the relation between socioeconomic context and the risk of hospital- acquired skin infection may be weak, challenging the findings of Cavero-Guardamino, 19 who points out life standards as a risk factor for skin infection in inpatients. This relation deserves to be more thoroughly explored in further studies.
Dermatology contributions in hospitals and its challenges Considering the potential severity of dermatological conditions in the hospital setting, adequate detection and treatment of such conditions become essential components of inpatient management. 7,10,16Dermatologists are the most suited professionals to establish accurate diagnoses, sometimes based on a simple physical exam and clinical history. 2,20
Galimbert et al 20 suggest that hospital dermatology could help to shorten hospitalization periods, reduce costs, and mitigate the need of outpatient care after hospital discharge. From another perspective, outpatient dermatology cannot be disregarded, since dermatological care has the potential to reduce the burden of new and recurrent hospitalizations due to skin diseases, phasing out the use of drugs and unnecessary surgeries. 4,14,20
Among dermatology contributions, we can include the preparation of skin disease management guidelines, the refinement of sample collection techniques for mycological examination, as well as an enhanced consultancy process, guiding non-dermatology specialists to adopt more adequate and accurate descriptions of skin lesions and conditions. 7
Furthermore, dermatology may also contribute with educational support to non-dermatology residents and other healthcare professionals. 7,34Hu et al 14argue that dermatologists could also contribute to nurse education about wounds and bandages.
Regarding medical education in dermatology, general practitioners and non-dermatology specialists frequently struggle to properly diagnose and treat skin diseases, which leads to inaccurate diagnoses and inappropriate therapies, as well as references with poor descriptions of skin lesions. 7,14,34,35This difficulty may be related to the variability in the Dermatology curriculum amongst medical schools, which in some cases may not offer suitable curriculum time to this specialty. 1,35For this reason, Beshay et al 36 stress the importance of structuring hospital dermatology services and referral and counter-referral processes as stimulators of dermatology education.
All these factors point to the crucial role that Dermatology may perform in hospitals, improving diagnosis and treatment, offering specialized knowledge to other healthcare professionals, and reducing hospitalization costs and iatrogenic interventions.
Conclusion
This study demonstrates that dermatological diseases are highly represented among hospitalized patients, and they demand early diagnosis and treatment due to the risk of systemic dissemination, sepsis and mortality. Most studies evaluated corroborate the significance of hospital dermatology services for enhanced inpatient care. With respect to the most frequent dermatoses, ‘skin infections’ was the most cited group, with bacterial, fungal and viral infections being among the main dermatological diseases in hospital settings. Drug eruptions also evidenced a high frequency in many publications.
From this literature review, we emphasize the relevance of dermatology in inpatientcare for its potential to support other medical specialties in optimizing diagnostic and therapeutic procedures.