Introduction
The domain of nasal reconstruction is essential for every dermatologic surgeon, as skin cancer involving the nose is very frequent and its prevalence is increasing. 1 Correct nasal reconstruction should preserve the vital function of the nose, while preserving the integrity of complex facial expression. A variety of flaps have been designed to provide coverage of nasal defects.
Tissue importation flaps comprehend a group of flaps that employ the concept of transferring tissue from a distant reservoir into a defect when other adjacent repair options are unsatisfactory. 2 They can also be called interpolated flaps. Although they represent a powerful tool for reconstruction of large defects, they have the disadvantage of usually being two- or three-stage procedures. The first stage includes the initial planning and implementation of the flap. The vascular pedicle is then left in place for approximately 3 weeks in order to ensure adequate blood supply. The second stage involves the separation of the pedicle and the insetting of the proximal flap. In some cases, a third stage for refinement of the flap is also required.
Tunneled flaps are variants of tissue importation flaps in which a tunnel is created in the deep subcutaneous plane to allow flap transfer from the donor site to the defect. The pedicle of the flap is hidden under the tunnel and, therefore, is unnoticeable. Performing a tunneled flap allow complete reconstruction of a defect in just a single surgery. This can be very useful while repairing a large defect in patients in whom a second surgery would be unadvisable. Although these flaps may require revision due to pincushioning caused by the pedicle along the path of the tunnel, this revision is not na immediate need and can be performed several months after the first surgery.
The main examples of tunneled interpolated flaps that can be used in the reconstruction of nasal defects are the tunneled paramedian forehead flap and the tunneled melolabial flap. This revision will focus on these two flaps.
Anatomy and surgery of the nose
Although the nose is itself an aesthetic region of the face, it can also be divided into several aesthetic subunits. Each subunit can be proportionally over-or underdeveloped relative to other noses, but there is a consistent general configuration from nose to nose. The nine aesthetic subunits of the nose include: nasal tip, dorsum, paired sidewalls, paired alae, paired soft tissue
facets and columella. 3 Five of these nine units are convex (tip, dorsum, alae and columella) and four are concave (sidewalls and soft tissue facets). 4
Reconstruction of nasal skin defects after tumor excision is not limited to simply filling a defect. Basic rules in nasal restorative surgery include:
The need of replacing surgically ablated tissue with similar looking
Placing of incisions for local flaps along borders of aesthetic regions 3-7;
Ablating the skin of an entire unit when > 50% of this unit is missing 3,4;
Designing local flaps so that they are not transferred across the borders
of aesthetic regions, especially if the border has a concave topography 3,8 ;
Using the contralateral unit as a template for the flap design when
reconstructing a paired nasal unit;
Keeping concave what is concave and convex what is convex. 5
It is important to notice that nasal reconstruction might also need reconstruction of the structural support of the nose, i.e. bones, nasal cartilages and mucosal lining, but these aspects will not be revised on this article.
Tunneled interpolated paramedian forehead flap
The forehead has served as a donor site of tissue for nasal reconstruction for centuries and many different flaps have been developed. 9
One of the first to be described was the median forehead flap, which was based on a wide pedicle capturing one or both supratrochlear arteries. 9Later, it was shown that the forehead flap could be based on a single supratrochlear artery and this paramedian design enhanced the versatility of this flap. 9 Furthermore, Skaria et al shown that these arteries are not included in most of forehead flaps, with no impact on flap survival. 10 The midline forehead flap combined features of both flaps by being based on a narrow, oblique, unilateral pedicle but with the skin of the remaining flap located vertically in the precise center of the forehead. 9 All these three flaps are interpolated and require a second-stage procedure for pedicle division. To overcome this issue, in 1963, Converse and Wood-Smith described for the first time a single-stage tunneled forehead flap. 9 However, because this flap was of a median design, it created problems with inadequate reach and marked bulkiness along the glabella. 9 Therefore, more recently, a tunneled paramedian forehead flap has been designed.
The paramedian forehead flap is classically an axial flap based on a single supratrochlear artery. It is the most useful flap for reconstruction of subtotal and total nasal defects that are too large to be repaired with full-thickness skin grafts, nasal local flaps, composite auricular grafts or interpolated melolabial flaps (Fig. 1). 3,6In general, nasal defects larger than 2 cm in width in the horizontal axis are best repaired with a paramedian forehead flap. 3 In addition, this flap is best for reconstruction of nasal defects with exposed bone or cartilage and in instances in which the central face has been irradiated. 3
Procedure
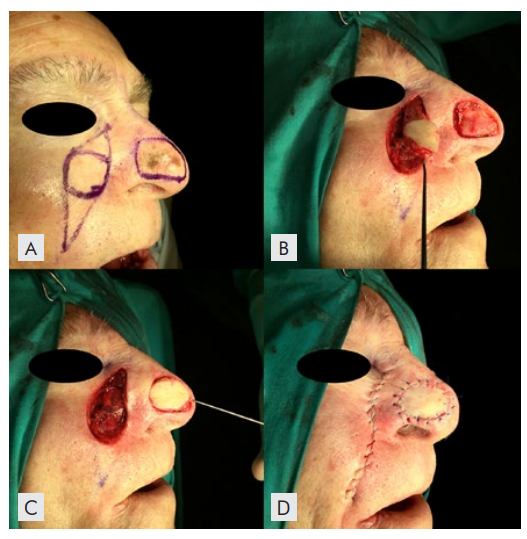
Reconstruction of a nasal defect with a tunneled paramedian forehead flap requires especial planning and preparation (Fig. 1). The design is similar to that of a classic two-stage paramedian forehead flap. Preoperative assessment includes measurement of the defect and consideration of the required length and width of the flap. 3 It is necessary to measure correctly the pedicle and to compensate the shortening caused while mobilizing and tunneling the flap. 11 Attention must also be payed to the height of the anterior hairline and degree of forehead skin laxity. 3
The origin of the supratrochlear artery is consistently found to be 1.7 to 2.2 cm lateral to the midline, and the artery exits the orbit by piercing the orbital septum. 3 At the level of the eyebrow, the artery passes through orbicularis and frontalis muscles and continues vertically upward in a subcutaneous tissue plane. 3 The flap should be designed in a way to be centered on the suptratrochlear artery and its ramifications. 6 The pedicle should be around 1.5cm wide to allow transfer of the flap with less rotation at the pedicle base, without compromising the vascularity. 6,9
Once the markings have been placed, anesthetic blocking of the infratrochlear, supratrochlear and supraorbital branches of the ophthalmic branch of the trigeminal nerve is recommended. 6 After the excision of the primary tumor, the flap procedure begins by incising the distal portion of the flap (on the upper forehead) through skin until the muscular fascia. 6 The incision is made on the inside of the line drawn to slightly undersize the flap. Dissection progresses inferiorly in the subgaleal plane and it is gradually deepened until it reaches just above the periosteum in the proximal third of the flap (just above the brow) - that will constitute the pedicle. 2 The pedicle is then deepithelialized with a scalpel.
Next, a tunnel under the glabella is bluntly dissected in two planes: just above periosteum and in the subcutaneous plane. 12 The width of the tunnel should be 2-3 cm (twice that of the pedicle) and the dissection is made from the supraorbital rim toward the nasal defect. A portion of the procerus muscle may be resected to create adequate space for the deepithelialized pedicle. 9,12The flap is then passed through the tunnel and stitched into place. The distal end of the flap is thinned to match the thickness of the remaining nasal skin before its inset. 2 Flap thinning may be accomplished without concern for compromise of the flap’s vasculature because the supratrochlear artery travels superiorly in the subcutaneous/subdermal tissue plane from a point 1 cm superior to the level of the eyebrow. 3,12
Bilaterally, the forehead donor site is undermined in the subgaleal plane and then closed in a layered fashion. 2 The widest part of the forehead defect may not close directly, but can heal well by second intention. 2,3
For patients with a low anterior hairline, it may not be possible to design the flap with adequate length to reach the columella or tip without transferring hair-bearing skin to the nose. In these cases, hair follicles can be cauterized at the time of transfer or later in a post-operative scar revision. 3
Advantages
The interpolated paramedian forehead flap provides the best color and texture match to the nasal skin, and is, therefore, the gold standard for nasal reconstruction. 6 The superficial axial blood supply of the flap provides ample nourishment, making distal flap necrosis unlikely. 12 The risk of wound infection is also reduced. Because the tissue to be imported is not immediately adjacent to the surgical wound, this flap offers the advantages of not crossing aesthetic subunits or distorting free margins associated with flap harvest, thus following one reconstructive surgery basic rule. 12
The most significant advantage of the tunneled interpolated paramedian forehead flap is the ability to bury the pedicle, obviating the need for a second surgery for pedicle division and all the inconveniences of having a visible pedicle during 3 weeks. Some people suffer significantly during the interim period with the interpolated pedicle, because of the obvious unaesthetic effect and the need for careful wound care due to common hemorrhage and drainage from the undersurface of the pedicle. By obviating the need for a second surgery, the tunneled flap will also reduce surgery-associated costs and will fasten patient recovery.
Disadvantages
In general, complications arising from the use of paramedian forehead flaps are rare. Because of the great vascularity of this flap, one of the most common complication is the development of small hematomas under the distal flap, so an adequate hemostasis is essential.3
Another minor disadvantage is the donor site scar and the donor site scar and the necessity for a two-stage procedure. Fortunately, the donor site scar is rarely unsightly, and the two-stage procedure can be overcome by performing a tunneled flap.
There are some disadvantages of the single-stage tunneled forehead flap.
First, the procedure is technically more challenging. Deepithelializing the pedicle and creating a subcutaneous tunnel under intact glabellar skin can be tedious, and inadvertently dissecting in the wrong plane runs the risk of amputating the flap.
Second, passing flaps through a subcutaneous tunnel may compromise the vascularity of the pedicle if the tunnel is not wide enough. These flaps should be used with caution in settings of increased operative risk such as smokers or in fields of previous radiation therapy. 12
Third, tunneled flaps can create a contour deformity along the path of the pedicle, 3 with a slight bulging of the glabella. However, this effect usually improves with time and rarely needs correction. 11,12Injections of triamcinolone acetonide may accelerate this natural regression. 9
Fourth, tunneled flaps are also prone to trapdoor effect, 11particularly when they are relatively bulky with round borders 12 (Fig. 2D). However, a subtle trapdoor effect does not always require a revision, as massaging the scar might be enough to flatten the region.
Reducing the flap size in 20% to 25% as compared with the primary defect, suturing in a way as to lower the flap below the surrounding skin and undermining extensively the borders of the receptor area are techniques to help minimizing this problem. 11,12Intralesional steroid injection can also help to correct this deformity.
Tunneled interpolated melolabial flap
Melolabial cutaneous flaps are skin flaps harvested from the melolabial fold lateral to the melolabial crease that separates the cheek from the caudal nose, upper and lower lips. 3 There is usually sufficient skin to enable transferring sizable flaps for reconstruction and allowing primary closure of the donor site. 3,5The suture line of the donor defect can be positioned in or parallel to the melolabial crease to provide optimal scar camouflage. 3
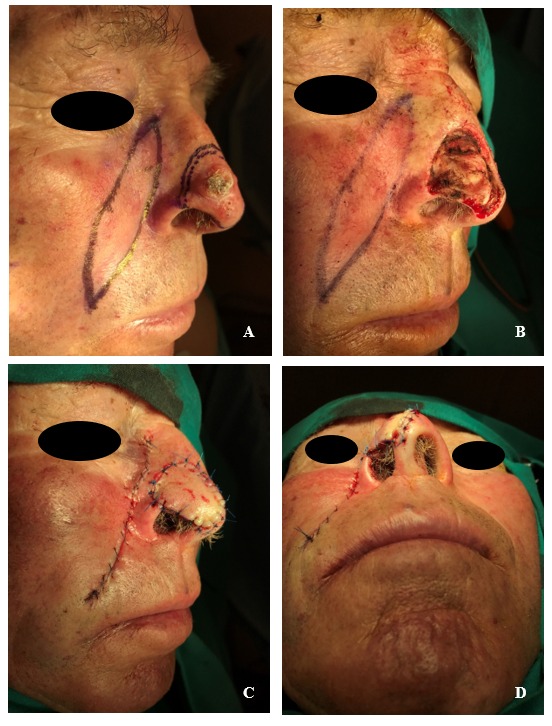
The melolabial interpolation flap has been used mainly for defects of the nasal ala (Fig. 3), especially for complex (including full-thickness defects) or large defects with maximal width of 2.5 cm affecting the alar rim. 2,13According to Krishnan and colleagues, only deep alar defects located entirely on the ala can be appropriately repaired with this flap, and superficial defects or tumors involving the ala but also other nasal subunits should better be treated with other techniques. 14 In practice, however, this flap offers a good aesthetic outcome even on tumors extending beyond the ala, and on moderate-sized nasal tips tumors when a paramedian forehead flap is less optimal (Fig.s 4 and 5). 2,5The interpolated melolabial flap is classicaly a two-stage procedure, but it can be converted into a single-stage procedure if a subcutaneous tunnel is created.
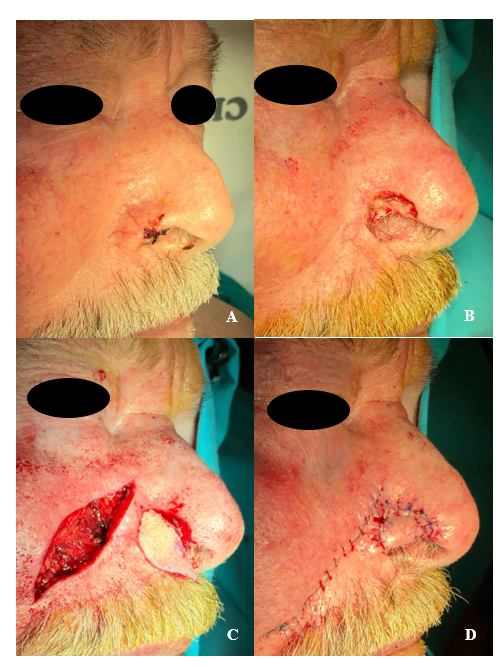
Figure 3 Tunneled interpolated melolabial flap for a defect of the right nasal ala. (A) primary tumor; (B) tumor excision; (C) flap movement; (D) flap suture.
Procedure
The first step is planning (Fig.s 4 and 5). A gauze can be utilized to ensure proper flap length that will allow tension-free transfer of the flap from the donor site to the defect. An additional length of the flap will be required to compensate for the curvature of the flap as it is passed through the tunnel. 14
The flap pedicle should be designed as close to the nasal pyramid as possible to reduce the length of the tunnel and increase its viability. 5 The pedicle is designed as a Burow’s triangle extending superiorly from the flap along the curvature of the melolabial fold and will incorporate branches of the angular artery. 12Another Burow’s triangle is designed to extend inferiorly from the flap along the melolabial fold to facilitate linear closure of the donor site. 12
The procedure begins by incising the flap’s inferior border on the cheek to the midsubcutaneous plane. 2 Deepithelialization of the proximal part of the flap is performed through scalpel removal of the epidermis overlying the vascular pedicle. 12 Dissection continues superiorly beyond the flap beneath the deepithelialized region, where the plane is gradually deepened to generate a vascular pedicle containing superficial portions of the facial musculature.12,15
The most distal portion of the pedicle should be no thicker than 3 to 4 mm to avoid bulkiness in the nasal-facial sulcus after the tunneling process.14On the contrary, the more proximal portion of the pedicle should be thicker than 3 to 4 mm to ensure a robust blood supply.14
Once the pedicle dissection is complete, both donor and recipient sites need to be widely undermined.14A short tunnel between the primary and the secondary defects is created by blunt undermining in the deep subcutaneous plane just above the muscle.12The flap and its pedicle then pass through this tunnel. A tunnel width of 75% of the width of the widest point of the donor flap shall be sufficient.16
Unlike the forehead flap, the melolabial flap has a random blood supply and cannot safely be thinned of as much of its subcutaneous fat.3The flap is then sutured into the wound without tension, slightly sinking the flap below the surrounding edges.12The donor defect is closed up primarily to the base of the pedicle.
Kearney and colleagues published a tunneled interpolated melolabial flap similar to the one described above, but they performed a flap turnover technique (based on the classic Spear flap17) to reconstruct a full-thickness defect of the internal portion of the alar rim.16Their technique includes:
Passing the flap through the tunnel so that the adipose tissue of the flap is facing anteriorly;
Suturing the proximal apex of the flap to the internal nasal mucosa
Suturing the distal apex of the flap to the external skin of the ala nasi.16
Advantages
Melolabial interpolation flaps have the great advantage of crossing over rather than through the intervening tissue between flap donor site and the defect, so they preserve the lateral alar groove and the alar-facial sulcus, which are very difficult to reconstruct.3,16Another advantage is that this flap can be harvested in regions of redundant tissue that are not immediately juxtaposed to the defect.3The flap also offers an excellent color and texture match, because the skin of the melolabial fold is particularly similar in sebaceous glandularity and texture to the skin of the ala.3
This technique also minimizes flattening of the upper melolabial fold because the majority of skin removed from the cheek is from the middle and lower portions of the fold.3 Another advantage over the more conventional transposition flap is evident when necrosis of the distal flap occurs.3 In this case, the interpolated flap may be dissected away from the defect, trimmed of devitalized tissue and reattached to the nose, as long as there is sufficient remaining tissue.3 The advantages of the tunneled interpolated melolabial flap over the non-tunneled design are related to the fact that the former is a single-stage procedure (see above - Advantages of tunneled interpolated paramedian forehead flap).
Disadvantages
A disadvantage of all cheek flaps in men is the transfer of hair- -bearing skin to the nose. This is particularly true for the interpolated flap because it is harvested in the hair-bearing midportion of the melolabial fold.
The disadvantages of passing a flap through a subcutaneous tunnel were already described (see above - Disadvantages of tunneled interpolated paramedian forehead flap). Of note, the risk of trapdoor effect of tunneled flaps can actually be beneficial when recreating the round shape of the ala nasi.11,15
Conclusion
When addressing more complex nasal defects that are not amenable to local flaps, interpolation flaps may offer contour restoration, flap viability and a final cosmetic result surpassing that provided by other repair options. The inconvenience of being a two-staged surgery can be overcome by creating a subcutaneous tunnel through which the flap and its pedicle are passed. However, the most optimal outcomes will not arise from following a “cookbook” approach, but rather from developing conceptual awareness of the potential benefits of single-staged tunneled flaps in a variety of surgical defects.