Introduction
Pigmented epithelioid melanocytoma (PEM) is a rare melanocytic tumor composed of pigmented epithelioid and dendritic melanocytes with large nuclei.1This histologic entity encompasses tumors previously described as epithelioid blue nevus of the Carney complex2,3and "animal-type melanomas". 2,4
Clinically, it presents as a slowly growing, densely pigmented papule or nodule on extremities, trunk and head.1This tumor is more common in young adults and children but can occur at any age.2
Most cases are sporadic1 and a small subset of cases is associated with the Carney complex.2 Carney’s complex is a familial syndrome characterized by blue naevi, lentigines, myxomas and rare tumors such as psammomatous melanotic schwannoma.3
Histological findings of PEM include: wedge-shaped symmetrical configuration; central increased cellularity; epithelioid cells, dendritic cells and melanophages.1 Clusters of large multinucleated cells with vesicular nuclei and macronucleoli (Reed-Sternberg-like) are the most distinct finding in PEM.1
The treatment comprises of simple excision. Although Ludgate et al and Zembowics et al reported a positive sentinel lymph node biopsy (SLNB), respectively in 47%5 and 46%,2 there is no evidence to recommend that sentinel lymph node sampling in primary cutaneous PEM has therapeutic or prognostic value.1
This case report describes the diagnosis of PEM in a 5-year-old patient presenting with classic clinical features and compatible histological findings.
Case Report
The patient is a female 5-year-old from Campo Grande in the state of Mato Grosso do Sul, Brazil. At a Dermatology consultation her mother expressed concern over a dark papule that had appeared on her daughter's right thigh 2 years prior and was slowly growing in size. The lesion was asymptomatic. No palpable lymph node was noted. There was no history of frequent sun exposure.
The patient had no prior medical conditions, was not using any medication and had never undergone any skin biopsy procedures. There was no personal or family history of skin cancer.
A 7 mm hyperpigmented bluish papule was observed on the posterior right thigh. On dermoscopy the lesion showed a continuous blue-gray blotch of pigment with no other visible structures.
The lesion was promptly excised. Histopathology showed a circumscribed, symmetrical, wedge-shaped dermal proliferation composed predominantly of pigmented epithelioid cells and dendritic cells. The cells had large nuclei and prominent nucleoli. In some areas multinucleated cells were found. No mitotic figures were identified.
The clinical and histological findings were compatible with PEM.
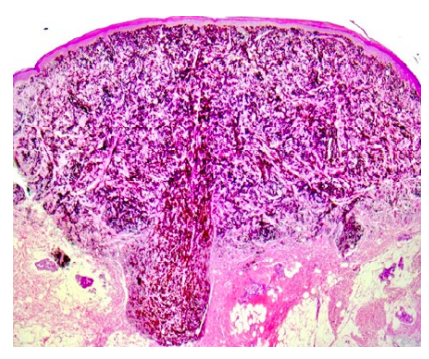
Figure 2: Symmetrical, wedge-shaped dermal proliferation composed predominantly of pigmented epithelioid and dendritic cells (H&E x100).
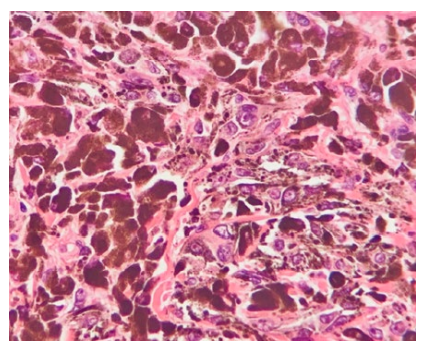
Figure 3: Pigmented epithelioid and dendritic cells with large nuclei and prominent nucleoli (H&E x400).
Discussion
Sentinel lymph node (SLN) involvement observed in the majority of PEMs6 along with the tumor once being categorized as an "animal-type" melanoma2 prompted most previous reports to include SLN sampling as a diagnostic procedure. However, the frequent SLN involvement in PEMs does not have the same adverse prognostic significance as in conventional melanoma2,6-8and the positive rate in cases undergoing SNLB may be over-estimated due to a more progressive clinical course or deeper tumor cell invasion.9
Another theory is that PEMs may be part of the neoplasms known as "benign metastasizing” tumors.8 These particular kinds of tumors include both cutaneous and non-cutaneous lesions such as benign melanocytic naevi, endometriosis and metastasizing leiomyomas.8
Additionally, based on current studies, a positive sentinel lymph node sampling appears to present little important evidence of the lesion's biological potential and its risk of developing clinically significant metastatic disease.10Taking that into consideration it can be argued that SLN sampling should not be performed in every patient with PEM.8
There are no clearly established criteria for performing SLNB in PEM patients9 and no histological criteria predictive of potential metastatic behavior of the tumor.2,10Current studies suggest that PEM is an indolent melanocytic tumor and long-term follow-ups have not revealed disease-specific lethal cases regardless of tumor deposits in sentinel lymph node sampling.1
Sentinel lymph node sampling was not performed in this case due to lack of evidence proving diagnostic or prognostic value of this practice on this kind of tumor.1A complementary wide surgical excision was performed and the patient will go through a long follow-up period.
In conclusion, while it is considered to be an indolent tumor, PEM patients should undergo a long follow-up period and further studies are needed on whether SLNB should be performed as a staging procedure in every case of PEM.
















