Introduction
Cutaneous tuberculosis is a rare form of extrapulmonary infection caused by the Mycobacterium tuberculosis complex, Mycobacterium bovis and Bacillus Calmette-Guerin.1,2There are various clinical forms of this condition depending both on individual immunological factors, characteristics of the bacillus, environmental factors and the inoculation pathway.3 Although considered the most common subtype of cutaneous tuberculosis in studies conducted in Spain, China, Indian, Japan and Pakistan, it is known that lupus vulgaris is underestimated and its diagnosis can be neglected.4,5We present an immunocompetent patient with lupus vulgaris whose clinical and histopathological features were challenging in establishing the diagnosis.
Case Report
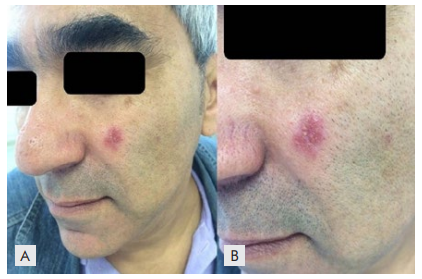
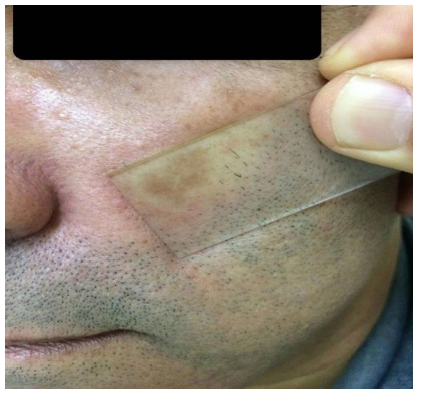
A 35-year-old male patient, a former truck driver, immunocompetent and without relevant pathological antecedents, sought medical care in December 2015, with an asymptomatic erythematous papule presenting a bright surface, half a centimeter in diameter, in the left malar region, with 6 months of evolution. With the diagnosis of an acneiform lesion, topical erythromycin 2% was prescribed. The lesion progressed and within approximately six months it presented as an asymptomatic erythematous-infiltrated oval plate with well-defined limits, 1 cm in diameter. Histopathology of 2 incisional biopsies was consistent with granulomatous rosacea, and a topical immunomodulator was instituted (tacrolimus ointment). When the patient was observed again after four months there was persistence of the plaque, but with a few pustules (Fig. 1). On diascopy it presented the apple jelly sign (Fig. 2). New diagnostic hypotheses were suggested, including sarcoidosis. A new biopsy showed a granulomatous inflammatory process (tuberculoid granuloma), without necrosis (Fig. 3). Histochemical studies for fungi (GMS and PAS) and BAAR (FITE-FARACO) were negative as well as the immunohistochemical study with antibody anti BCG (Dako B 0124, Copenhagen). Culture and IGRA (interferon gama releasing assay) Quantiferon TB Gold were not performed. The close correlation of the histopathological findings with the clinical data directed the investigation towards lupus vulgaris. A PPD (tuberculin test) revealed an eleven millimeter papule and chest X-ray was normal.
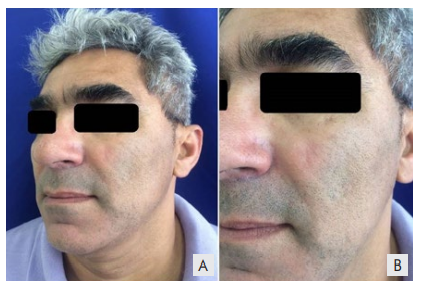
Treatment was initiated with rifampicin 600 mg, isoniazid 300 mg, pirazinamide 1600 mg and etambutol 1100 mg daily (RHZE) for two months followed by rifampicin 600 mg and isoniazid 300 mg daily for the next 4 months. There was a significant improvement of the lesion in the first months with resolution by the end of the treatment with a slight atrophy. No recurrence of the condition was observed after three years (Fig. 4).
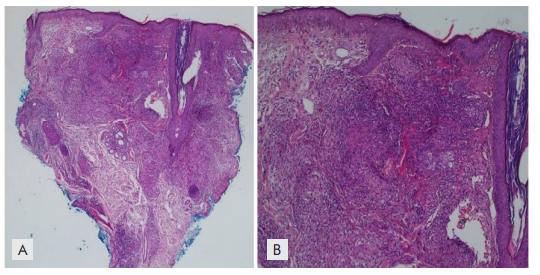
Figure 3: A and B: Dermal inflammatory infiltrate consisting of lymphocytes and histiocytes forming epithelioid granulomas without central necrosis. H&E 100X and 200X respectively
Discussion
Current data from the literature indicate that cutaneous tuberculosis accounts for 1%-2% of all extrapulmonary forms of tuberculosis in the world, therefore a rare condition, especially in industrialized countries.1,6In Europe, the predominant form of cutaneous tuberculosis is lupus vulgaris, which may represent 61.1% of the cases,7 whereas scrofuloderma is the most common presentation in some developing countries such as Brazil.5 According to the WHO, Brazil is one of the twenty countries in the ranking with the highest incidence of tuberculosis,8 and 40% of patients over 45 years of age with typical cutaneous lesions may have coexistent pulmonary tuberculosis, 9 which was not apparently the case of this patient.
Cutaneous manifestations of tuberculosis are classified into true cutaneous tuberculosis or tuberculids.3 Cutaneous tuberculosis includes a continuous spectrum according to the degree of immunity and the route of infection. Some authors further define the infection according to the amount of bacilli found in skin lesions as paucibacillary or multibacillary, the latter being associated with more deficient degrees of immunity.2,4,9
In lupus vulgaris, it is known that individuals have moderate to high degrees of cell-mediated immunity, with adequate immune activation and normal serum immunoglobulin levels. The number of bacilli in the skin is small, and they are not detected in special staining in histopathology or PCR and most will not be able to grow in culture.2,4
Lupus vulgaris is secondary to a pre-existing focus, especially in the joints, bones or lymph nodes, and lesions depend mainly on the hematogenous and lymphatic spread of the microorganism.10 In rare cases, the disease may develop after inoculation or an exogenous source.11 When it is not possible to find the focus, it is postulated that the picture may have been triggered by reactivation of latent cutaneous focus secondary to silent bacteremia.10
In western countries lupus vulgaris occurs most commonly in the head and cervical region. and presents in discrete and varied forms, having four predominant types: hypertrophic, ulcerative, vegetative and plaque-type, which is the form in this patient. In this clinical presentation, lesions consist mostly on a brownish red papule or plaque, with progressive infiltration, an “apple jelly” appearance on diascopy (Fig.s 1 and 2) and tendency to centrifugal growth with central atrophy.3,4
In general, cutaneous tuberculosis may have no systemic symptoms and the skin lesion is not specific, which can make the diagnosis a great challenge for dermatologists in daily practice.6,12Lesional characteristics in this patient associated with the high level of immunity precluded an early diagnosis. At this stage lupus vulgaris may mimic other dermatoses such as sporotrichosis, cutaneous leishmaniasis, discoid lupus erythematosus, sarcoidosis, acne rosacea, nummular dermatitis, psoriasis, lichen simplex chronicus, dermatophytosis and erythema annulare centrifugum.4,10,12
If untreated, lupus vulgaris lesions persist for years, gradually growing in size up to tens of centimeters, with ulcerations and tissue destruction, leading to significant aesthetic disfigurement. Malignant transformation into squamous cell carcinoma can occur in 0.5% to 10.5% usually after 25-30 years of untreated disease.13
The diagnosis is based on clinic and histopathological findings, bacterial cultures and PCR.6 As lupus tuberculosis tends to occur in previously sensitized patients, PPD is usually positive, as in this patient, but its diagnostic value is considered controversial. Culture of the collected material may or may not show Koch's bacillus.2,9
Common histopathological findings are pseudoepitheliomatous hyperplasia associated with multiple and well developed tuberculoid granulomas, with or without caseous necrosis in the upper dermis. Non-specific inflammatory infiltrate and absence of bacillus are other striking features.2,3
Negative culture implies searching for bacillus identification through PCR or other technique. Although these tests are the gold standard for the diagnosis, they have a low sensitivity: 50% a 72% for PCR and 80% for culture in samples with BAAR negatives.6 In the absence of such examination, a therapeutic test can be used, as corroborated by Pinho A et al and Thomas S et al.10,14,15In this patient after a two months treatment with rifampicin, isoniazid, pyrazinamide and etambutol followed by four months of rifampicin and isoniazid there was a complete regression of the lesion (Fig. 4).
We conclude from this case report the importance of thinking of lupus vulgaris in immunocompetent patients who present indolent cutaneous lesions with various clinical presentations, with or without an obvious primary focus of tuberculosis in a patient with a positive PPD or IGRA, particularly in endemic areas.