INTRODUCTION
Is one of the most common skin manifestations in patients with systemic lupus erythematosus (SLE), occurring in about 50% of cases at some time during the course of the disease. Distinct subtypes with specific or non-specific histological changes can be observed with both scarring (lichen planopilaris, pseudopelade, traction alopecia) and non-scarring forms of alopecia (androgenetic, alopecia areata, telogen effluvium).2
Discoid lupus erythematosus (DLE) of the scalp is a typical form of scarring alopecia, characterized by well-defined erythematous plaques with scales, atrophy, follicular plugging, central hypopigmentation, and peripheral hyperpigmentation.1 Lesions develop progressively from a non-cicatricial alopecia to a late scarring phase.
Patients with SLE develop DLE in 11.2% to 17.6% of cases. An early identification of the type of alopecia associated with SLE is very important for proper management to prevent irreversible follicular loss.
This case demonstrates a good evolution of multifocal alopecia, clinically compatible with DLE in a SLE patient. Interestingly, histopathology showed a leukocytoclastic vasculitis which is not a usual finding in DLE.
CASE REPORT
A 44-years-old female patient complaining of hair loss for 1 month had been diagnosed with SLE 4 years ago by the following criteria: antinuclear antibodies (ANA), (1:320), anti-double strand-DNA
antibody (1:320), arthritis, malar rash and low C4 serum levels. The disease was controlled under regular treatment with prednisone 20 mg/day and hydroxychloroquine 400 mg/day.
Dermatological examination revealed lesions only on the scalp with multiple areas of alopecia in the occipitoparietal region with erythematous plaques either with oedema or slight atrophy, some with central crusts, but no desquamation or hyperpigmentation (Fig. 1). Trichoscopy showed follicular red dots, large yellow dots, thick arboriform vessels, whitish areas with atrichia and grayish blue dots forming a dotted pattern (Fig. 2).
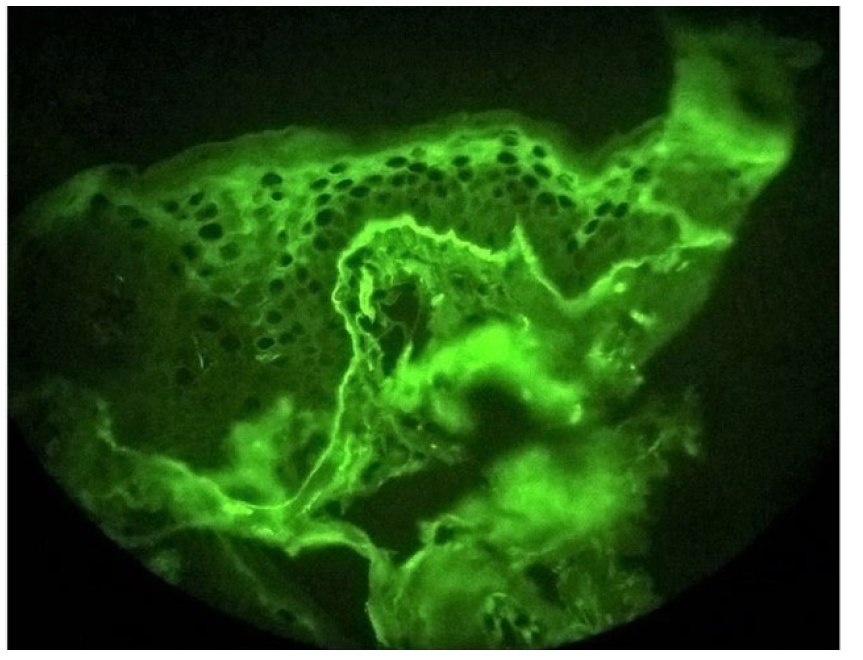
Histopathology of the scalp showed thickening of the follicular basement membrane, mucin accumulation in the dermis and a perifollicular and perivascular inflammatory infiltrate consisting of histiocytes, lymphocytes, and neutrophils, many in karyorrhexis, and fibrinoid necrosis of the vascular wall (Fig. 3). Direct immunofluorescence showed linear deposition of immunoglobulin M in the basement membrane zone (Fig. 4).
Due to the clinical presentation, thalidomide 100 mg/day and topical clobetasol propionate 0.05% cream twice a day were introduced, and the dose of prednisone was increased to 60 mg/day for two months. After nine months using thalidomide 100 mg and topical and oral corticosteroid, there was total hair regrowth and thalidomide could be stopped. After nine months of follow-up no further alopecia developed.

Figure 1 Multiple foci of occipitoparietal alopecia with erythematous, edemamatous plaques, hematic crust and atrophic areas.
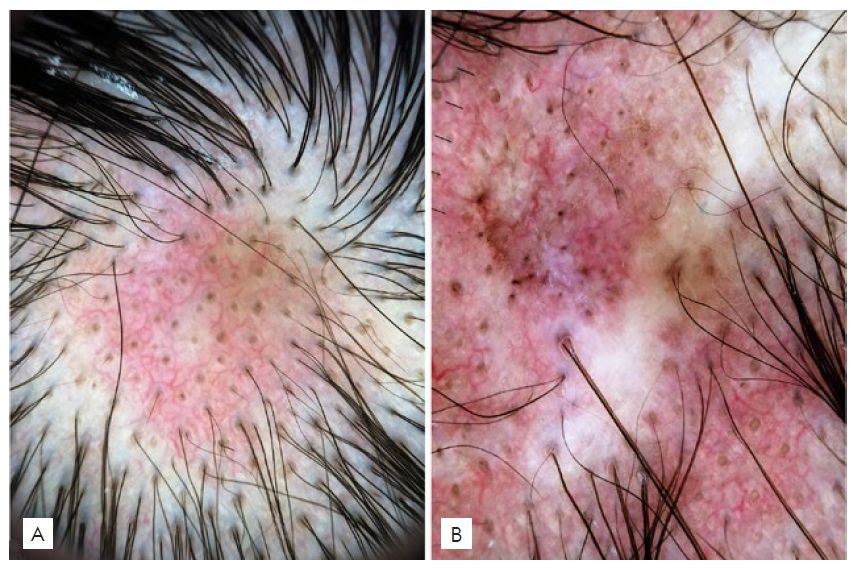
Figure 2 - A) Area of alopecia with follicular diameter variability, telangiectasia, reduction in the number of hairs per follicular unit. B) Atrophic hypochromic area, follicular red dots, brownish spots, tortuous blood vessels, follicular keratotic plugging and miniaturized hairs.
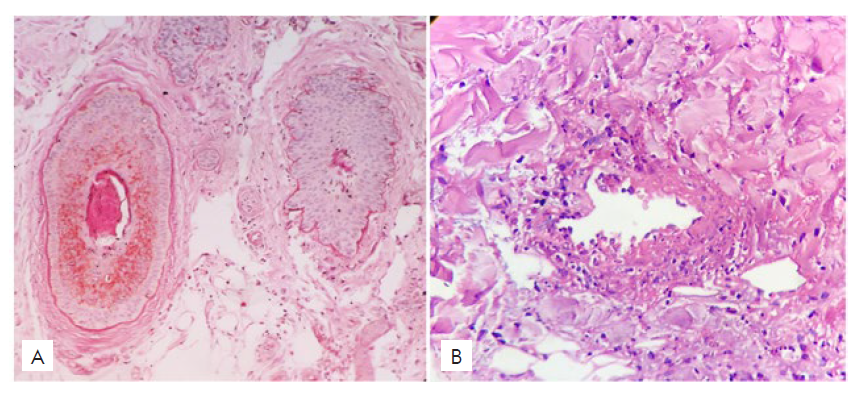
Figure 3 - Histopathology from two biopsies performed in the parietal area with 4mm punch. A) Perifollicular thickening of the basement membrane stained with periodic acid-Schiff stain (PAS 400x); B) Fibrinoid necrosis and perivascular infiltrate with cellular debris (H&E 400x)
DISCUSSION
SLE may be associated with localized and well-defined areas of partial alopecia on the scalp as the initial presentation as well as at the time of exacerbations. Irregular non-cicatricial alopecia in SLE has histopathological and direct immunofluorescence findings similar to those of DLE, and the clinical history and trichoscopy are important in the differential diagnosis of these cases.
Trichoscopy in DLE is characterized by follicular red dots, yellow dots, tortuous blood vessels, dark brown dots, and greyish blue dots that form a speckled pattern,1,2most of them observed in this case report and, therefore, corroborating the diagnosis of DLE.
In other forms of non-scarring alopecia associated with SLE, large yellow dots and prominent tortuous vessels usually are not observed on trichoscopy, whereas a small perifollicular erythema and thin hypopigmented hairs are frequently present. This form of alopecia represents about 15% of cases of alopecia observed in SLE, but so far has received little attention in the literature.5
In the early stages of the DLE, there is a vacuolar change of the basal layer with necrotic keratinocytes, thickening of the follicular basement membrane, perivascular and periadnexial lymphocytic infiltrate, and increased dermal mucin.2,3Many of these findings were seen in this case, confirming the diagnosis of DLE, with the additional finding of leukocytoclastic vasculitis which is not usually observed in the setting of DLE.6 However, Udompanich et al suggest that polymorphic telangiectasia in the interfollicular area are caused by vasculitis and the local inflammation of the hair follicles leads to consequent hair loss.5
The choice of thalidomide is justified by the appearance of alopecia, when the patient was already under treatment with hydroxychloroquine 400 mg/day and prednisolone. Thalidomide is indicated at a dosage of 50-100 mg/day, with good response within two weeks.3 It reduces keratinocyte apoptosis by stabilizing lysosomal membranes and decreasing free radicals, and by inhibiting the synthesis and deposition of immunoglobulin M in the basement membrane.4 In this case updosing corticosteroids may also have contributed to reduce inflammation and enhance hair regrowth.
Due to the different patterns of alopecia in SLE, most of which are non-scarring forms, this case report demonstrates the importance of early diagnosis and treatment of SLE in order to avoid permanent hair loss.