We report the case of 10-year-old Caucasian child with no relevant personal history living in a farm with basic sanitation conditions, where pigs were bred. She reported a nodule on her right occipital region that, within 24-48 hours, turned erythematous with a small opening on the top in association with multiple adenopathies in the right cervical region. Oral amoxicillin/clavulanic acid and topical fusidic acid were prescribed, but within the edematous furunculoid nodule the central opening enlarged, and two larvae could be seen moving inside the hole (Fig. 1). The diagnosis of furuncular myiasis was considered and mechanical extraction of larvae was performed, leaving the cavity apparently clean. An oral dose of ivermectin (150 μg/kg) was prescribed and one month later, the wound was completely healed.
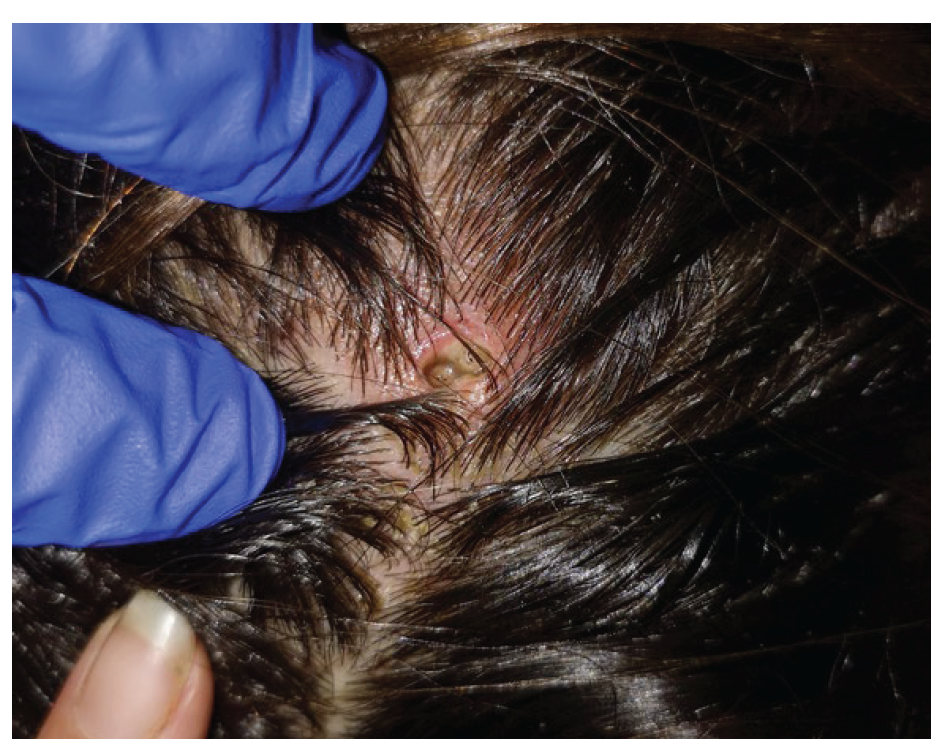
Figure 1 Inflammatory nodule on the scalp with a central ulcer where two larvae could be seen moving.
Myiasis is an infestation of the skin and mucous membranes by dipterous maggots, namely Dermatobia hominis, the human botfly, which can produce furuncular (the most common), creeping, or traumatic lesions.1-5Human myiasis is a worldwide infection, mostly related to warm and humid environment and frequently related to previous travel history, but other risk factors including poor hygiene and low socioeconomic status may favour the disease,3-5as in this case.
Lesions are normally single and usually harbour only one larva, with the breathing tube visible within the skin hole. Lesions occur most commonly on exposed areas, so scalp lesions are uncommon.3-5
Myiasis' diagnosis is clinical, but dermoscopy can be helpful.3,5
Treatment consists on the mechanic removal of the larva usually after application of a toxic substance.4,5 If larvae are not accessible, skin occlusion may be necessary to promote localized hypoxia and consequent larval migration to skin surface.4,5Surgical excision may be needed when dead larvae remain inside the skin. Oral treatment of human myiasis is not consensual, but ivermectin (single oral dose 150-200 μg/kg) is the main choice.6
This case of furuncular myiasis highlights some atypical findings, particularly the location on the scalp, and the rural and poor socioeconomic condition as another risk factor in the absence of previous travelling.















