INTRODUCTION
During December of 2019, a series of patients with pneumo-nia of unknown cause occurred in Wuhan, province Hubei, China. Those were later confirmed to be caused by the novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and the disease was called coronavirus disease of 2019 (COVID-19).1,2In the ensuing months, COVID-19 has quickly spread across the world and the World Health Organization (WHO) categorized the outbreak as a pandemic on 11th March 2020.1
This new virus is very contagious, spreading via droplets by coughing and sneezing. Prevention of COVID-19 is challenging because many infected individuals without or with mild symptoms have viral shedding.3 To halt the transmission, countries around the world have implemented social distancing and community containment strategies.3,4Social distancing measures could have a positive impact on other transmissible infections such as sexually transmitted infections (STI). However, COVID-19 pandemic has also interrupted the provision of clinical services for STI and undetected STI transmission will only lead to further increases. In this article we review the current available data on sexual behavioural changes among high-risk communities, STI testing services capacity during the pandemic and the effect of both these variables on STI incidence rates. The combined impact of these factors on STI epidemic trajectory is yet unknown.
THE IMPACT OF COVID-19 ON SEXUAL BEHAVIOURS
Common sense suggests that confinement measures focusing on physical distancing may help reduce the number of sexual contacts or at least the number of individuals with whom these contacts occur,5-7depending on the extent and nature of the changes in sexual behaviour.8,9
A cross sectional online survey to examine changes in the occurrence of physical sex with non-steady partners among men who have sex with men (MSM) in Belgium during the first weeks of the lockdown showed a substantial reduction of sexual contacts suggesting a low risk for STI during this period. The proportion of participants reporting physical sex with casual partners decreased from 53% to 7%, and with anonymous sex partners from 47% to 4%. Nine percent reported physical sex with non-steady partners, among these, 71% were either HIV positive or taking preexposure prophylaxis (PrEP) in the 6 months before.7 Among MSM using PrEP before the lockdown period, 47% stopped its use and only 8% reported concerns about not having pills so, the likely reason for this was a perceived reduced risk for HIV infection.7
A similar survey among MSM in Amsterdam found a 73% reduction in the number of casual sexual partners. Thirty eight percent of the participants reported casual sexual partners during the restrictions, which was related to prior sexual behaviour and low perceived importance of avoiding COVID-19.10 These results are in line with other studies from Australia, USA and China.8,9,11In Australia, MSM reported an 84% reduction in sex with other men between April 4 and April 29, 2020. This reduction occurred across all partner types outside a committed relationship.8An online survey involving MSM in USA showed that half of the participants had fewer sex partners, while 48% reported no change.9 This highlights that although a considerable decline was observed, a significant proportion of patients still engages on risky sexual behaviours.
In fact, a more recent cross-sectional survey of MSM in USA, reported a mean increase of 2.3 sex partners during COVID-19, a mean increase of 2.1 anal sex partners and a very small increase in the number of unprotected anal sex partners.12Increases in sexual behaviour were associated with increases in substance use during the same period. The authors argue that stay home orders may create more opportunities for sexual activities.12 Provisional data from Spain indicate that sexual frequency in homossexual contacts has increased but this statement covers all types of sexual activity including masturbation and online sex, which has increased in people of all sexual orientations.6 However, a higher percentage of people who engage in same sex relations say they have skipped confinement to meet sex partners.6
These somewhat contradictory results emphasize that there is a clear need to continue to provide STI prevention and care services.
THE IMPACT OF COVID-19 ON STI TESTING FACILITIES
The coronavirus containment measures have dramatically affected the health care system of countries worldwide, including STI screening. An online survey directed to the provision of STI testing services in the WHO European Region found a 95% decrease of testing volumes during March-May and 58% during June-August 2020 when compared to pre-COVID-19. These findings were con-sistent across all the surveyed infections (HIV, hepatitis B, hepatitis C, chlamydia, syphilis, and gonorrhoea). Reasons for these declines included firstly testing site closure during lockdown, reduced staff, reduced attendance and fewer appointment schedule, fewer serological samples dawn, laboratories overburden with SARS-CoV-2 testing and fewer referral to the facilities.13
The New York City Sexually Transmitted Diseases Prevention Training Centre at Columbia University administered an online provider survey to understand how the COVID-19 pandemic has been affecting the availability of sexual health care services. The survey assessed the services offered before March 1, 2020, and after April 1, 2020.14 Seventy-three individuals responded to the survey. Fourteen (19%) of the respondents stated that their clinics had been closed due to the COVID-19 outbreak, and 40 (56%) were functioning on an appointment only basis.14 Overall, 80% of respondents stated that since the beginning of the COVID-19 out-break, their clinic providers had restricted to treating STI presumptively based on symptomology, before testing. PrEP prescriptions were refilled without quarterly STI and HIV screening.14
From the patient’s perspective, one-third of USA MSM reported that COVID-19 epidemic has prevented them from HIV or STI testing.12 In their survey involving MSM in USA, Sanchez et al also found a considerable proportion of MSM who reported problems accessing HIV or STI testing and STI treatment.9
With most healthcare resources directed toward COVID-19, the pandemic resulted in a significant reduction on STI testing,13,14and a consequent potential for STI proliferation.14 Recommendations were released for STI clinical settings that have been disrupted or offering telehealth15 as well as for STI facilities still working but requiring a rapid adaption to the COVID-19 pandemic.16 When in-person clinical evaluation was not possible the main focus were on prioritizing patients with STI symptoms, those reporting a STI contact, and individuals at risk for complications and on oral treatment options for symptomatic patients and their partners.15 Syndromic treatment and expedited partner therapy are encouraged as a way to mitigate some of the effects produced by the decline in widespread testing.14-16Security recommendations for healthcare providers and patients for walk-in visits are also offered.16 The importance of maintaining access to STI care during the pandemic is reinforced despite the challenges. If STI services are suspended due to COVID-19, clinicians risk not detecting and treating as-ymptomatic STI, which could lead to increased diagnoses once the pandemic is over.16
THE IMPACT OF COVID-19 ON STI INCIDENCE RATES
Reported incidence rates of STI from most countries are not yet available but, considering the available data so far, an overall decline is expected. A study by Darcis et al, found a dramatically decrease on the number of HIV screening tests and diagnosis in Liege AIDS Reference Centre, Belgium. While a reduction of high-risk sexual behaviours has possibly contributed to the decrease of new HIV diagnoses, the authors argue that the rapid decline of HIV diagnoses, right after the beginning of the pandemic, is most likely caused by missed diagnoses of individuals infected before the establishment of containment measures.17 Similar results were reported by Latini et al, regarding the STI/HIV Unit of the San Gallicano Dermatological Institute in Rome, which has remained open during the pandemic, and where a reduction is STI diagnoses, particularly of early syphilis was observed.18 The STI service of Dermatology, Bologna, reported an 80% decline on medical appointments when comparing the 4 weeks before and after the lockdown. While the proportion of visits for syphilis, gonococcal pharyngitis and inflammatory genital diseases increased, the overall absolute registered numbers were considerable reduced.19 On the other hand, data from the STI clinic in the Provincia Autonoma di Trento, the Italian district most affected by COVID-19, revealed a comparable incidence of chlamydia, gonorrhoea and syphilis infections during the lockdown (9 March - 4 May).20
Notification data from the Federal Office of Public Health from Switzerland found a substantial reduction in almost all recorded infectious diseases in the 2020 period as compared to earlier years.21This decline was however less pronounced for STI which continued to occur. Gonorrhoeae and chlamydia cases were reduced by less than 20%, and infection in MSM accounted for more than half of the cases. On the other hand, there was a marked reduction of syphilis (85%) and HIV (57%). The authors state that this divergence may illustrate different high risk networks of transmission for these diseases.21
Statistics from the Health Protection Surveillance Centre in Ireland from the beginning of the year 2020 to 23 May indicate that chlamydia infections decreased by 21%, gonorrhoea by 18%, syphilis by 25% and genital herpes by 21% when compared with the same period of 2019.22
The US Centres for Disease Control (CDC) provisional data during weeks 12-40 of 2020, revealed a 20% decrease in the mean weekly count of chlamydia cases when compared to the first eleven weeks of the year. This effect was less pronounced for gonorrhoea (3% decrease) and an opposing trend was found for syphilis (5.5% increase).23
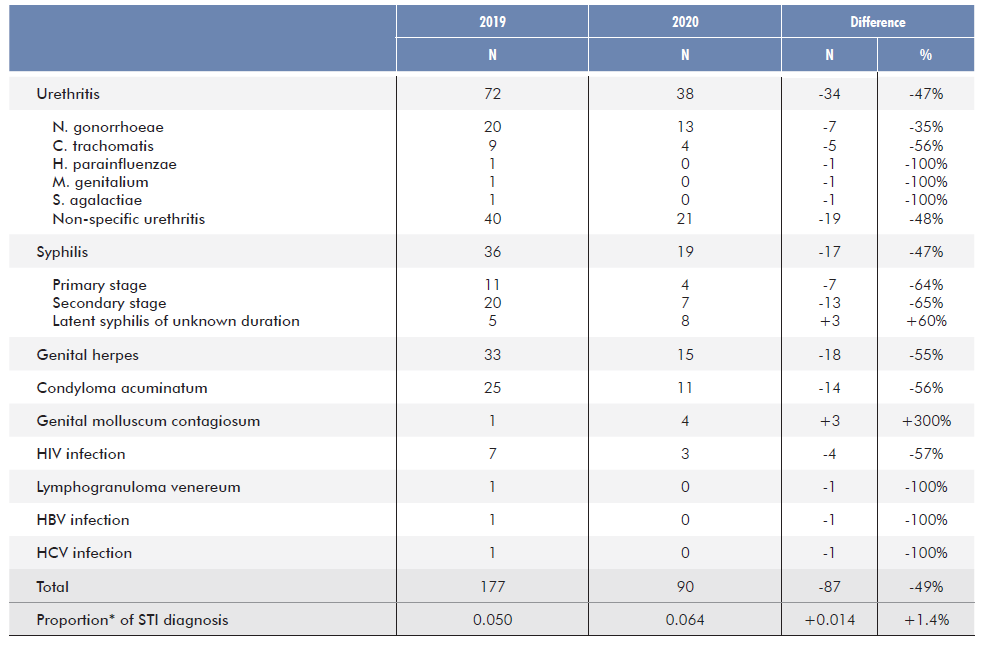
In our institution, Dermatology Emergency Services remained opened during the entire lockdown period. We reported a 60% decline on overall emergency visits and a 53% decline on STI-related visits between 15 March to 30 June 2020, comparing with the same period of 2019 (Table 1). When considering the total number of confirmed STI diagnosis, a 49% decrease was recorded. While the proportion of STI diagnosis has increased from 5% to 6.4%, the overall absolute registered numbers were considerably reduced. The only exception was genital molluscum contagiosum and latent syphilis of unknown duration, with an absolute increase in the number of identified cases (Table 2).
Table 1 EOverall and STI-related emergency visits between 15 March and 30 June of 2019 and 2020 in the Dermatology Emergency Department of Centro Hospitalar e Universitário Lisboa Norte, Portugal.
| Emergency visits | 2019 | 2020 |
|---|---|---|
| Total (N) | 3563 | 1415 |
| STI-related visits (N) | 171 | 80 |
| Men (N) | 150 | 67 |
| Women (N) | 21 | 13 |
| Mean age [Min-Max] (Years) | 32 [13-70] | 30 [18-65] |
Table 2 STI diagnosis between 15 March and 30 June of 2019 and 2020 in the Dermatology Emergency Department of Centro Hospitalar e Universitário Lisboa Norte, Portugal. (*Considering the total number of emergency visits (TE): TE, 2019=3563; TE, 2020=1415)
Overall, SARS-CoV-2 infection pandemic seems to result in a transient decrease of STI incidence, but it also favours late diagnosis which may result in further long-term consequences including sequelae for individual patients.13 It is not known whether this de crease represents reduced transmission or, more likely, a decrease in testing and reporting of cases.23
DISCUSSION
The disruption of sexual contacts due to physical distancing imposed by the pandemic may reduce opportunities for STI spreading.8 The incidence data on reported STI for 2020 are not yet available in many countries, even though, an overall decline is expected. As well as decreased exposure to infections as a consequence of social distancing, the apparent decrease on STI incidence rates may also be explained by less attendance at STI clinics and by a delay in reporting new cases. Only time and careful monitorization will clarify if it reflects a true decline in STI or delayed diagnosis. Jeness et al have adapted a network-based model of co-circulating HIV, gonorrhoea, and chlamydia for a population of 103 000 MSM in the Atlanta area. Their model shows that a 50% relative decrease in sexual partnerships and interruption of all services, both lasting 18 months, would generally offset each other for HIV, but have a net protective effect for other STI. Greater relative reductions and longer durations of STI Healthcare Services interruption would increase HIV and STI incidence.24
Although the apparent reduction in sexual contacts reported by most studies has the potential to reduce new STI diagnoses in short term, such reductions are likely to be transient. While sexual behaviour change may counterbalance STI Healthcare Services interruption, this will depend on overlap in timing of these changes.24 Both behavioural and testing data will need to be closely examined to assess the impact of the COVID-19 pandemic on STI notifications.8 Besides, a substantial number of MSM are already reporting that they are not strictly adhering to COVID-19 mitigation recommendations. If we maintain a sustained interruption in STI and HIV healthcare services, an increase in STI and HIV incidence rates will be expected.9 Early diagnosis and linkage to care for STI are key factors in controlling these infections and improving health outcomes. It is important to ensure that the response to STI is not compromised even during a pandemic lockdown.13,14,17,23
CONCLUSION
COVID-19 may have an impact on STI incidence with two im-portant factors playing a role. While behavioural changes may halt their transmission, STI specific healthcare service interruption may lead to an invisible spreading. Despite the social distancing measures, an overall conclusion is that STI are still occurring and although a transient decline in STI reported rates is expected it will have no substantive long-term impact for STI.
We highlight the need for effective STI prevention programmes during the pandemic as well as the critical importance of maintaining these clinics available amidst the COVID-19 and other pandemic responses.















