INTRODUCTION
Paracoccidioidomycosis (PCM) is a systemic granulomatous mycosis, endemic in Latin America.1 In Brazil, it is the leading cause of hospitalizations and death among all systemic mycoses in immunocompetent patients and an important cause of morbidity.2 The prevalence of infection by P. brasiliensis in endemic areas can reach 50%-75% of the adult population but only about 2% develop clinical manifestations.3 It presents in two major forms: acute/subacute (varying from 5% to 25% of the cases), affecting mostly children and young adults, frequently compromising the reticuloendothelial system, with enlarged lymph nodes in superficial and deep chains, associated with liver, spleen and bone involvement; and a chronic form (74% to 96% of the cases), involving predominantly adult males, which can be unifocal or multifocal, affecting usually lungs, oropharyngeal mucosa and skin.4 We report an unusual case of subacute paracoccidioidomycosis in an elderly patient with abdominal involvement mimicking cholangiocarcinoma.
CASE REPORT
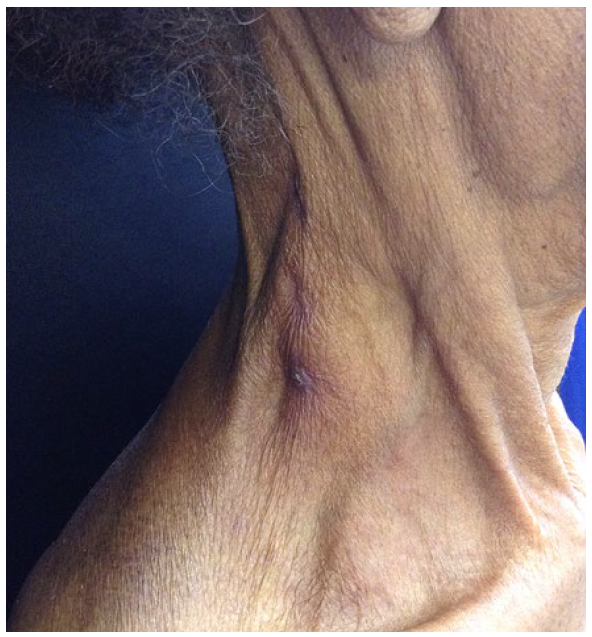
A 77 year-old female patient, resident in an urban area, smoker, with no known comorbidities, reported a cutaneous facial lesion for 4 months, associated with weight loss (10 kg), afternoon fever, weakness, anorexia, nausea, abdominal discomfort and, for the preceding two weeks also choluria, fecal acolia and jaundice, with no respiratory symptoms. Dermatological examination revealed a plaque with irregular erythematous verrucous borders and central atrophy occupying almost the entire forehead (Fig.s 1-2), plaques with a verrucous surface on the right supercilium and paranasal region, measuring about 2 cm each, and grouped erythematoous and violaceous papules in the left zygomatic region (Fig. 3). No mucosal lesions were observed. On physical examination, the patient was emaciated (28 kg), jaundiced, with painless, mobile and fibroelastic enlarged lymph nodes on the cervical and left supraclavicular regions, one of them with spontaneous fistulization of one cervical area (Fig. 4), but no masses or visceromegaly on abdominal palpation.

Figure 2 Plaque with irregular erythematous scaly edges with central atrophy occupying almost the entire forehead, extending to the scalp.
The hypotheses of paracoccidioidomycosis, lupus vulgaris, sarcoidosis and paraneoplastic syndrome were raised, and the patient was admitted for diagnostic investigation. Laboratory tests showed anemia, hypoalbuminemia, high total bilirubin (9.02 mg/dL), alkaline phos-phatase (2517 mg/dL) and gammaglutamyl transferase (889 mg/dL), configuring cholestatic jaundice. Serologies for HIV, syphilis and hepatitis B and C were negative and eosinophilia was not found. Chest and abdominal tomography revealed centrilobular emphysema and enlarged axillary and left clavicular lymph nodes, solid tissue thickening and marked dilation of intrahepatic bile ducts, in addition to lymph node enlargement affecting the porto-cavo-aortic space, periceliac and left ileocolic chains, some with necrotic centers. Tumor markers CEA and CA 19.9 were both negative, and cholangioresonance performed with the support of gastroenterology, showed a marked dilation of intrahe-patic bile ducts due to a poorly delimited stenosing tissue formation occupying the lumen of the common hepatic duct and extending to the right and left hepatic ducts, suggesting the possibility of cholangiocarcinoma.
Mycological examination (direct and culture) of a skin lesion fragment was negative and cutaneous histopathology revealed pseudoepitheliomatous hyperplasia, with neutrophilic intraepi-dermal microabscesses and intense mixed and diffuse dermal inflammatory infiltrate (Fig. 5A), permeated by round structures with a double refringent wall with single or multiple peripheral buds, some located inside multinucleated giant cells (Fig.s 5B and C), compatible with paracoccidioidomycosis. Serology for Paracoccidioides spp. was negative with the double immunodiffusion test.
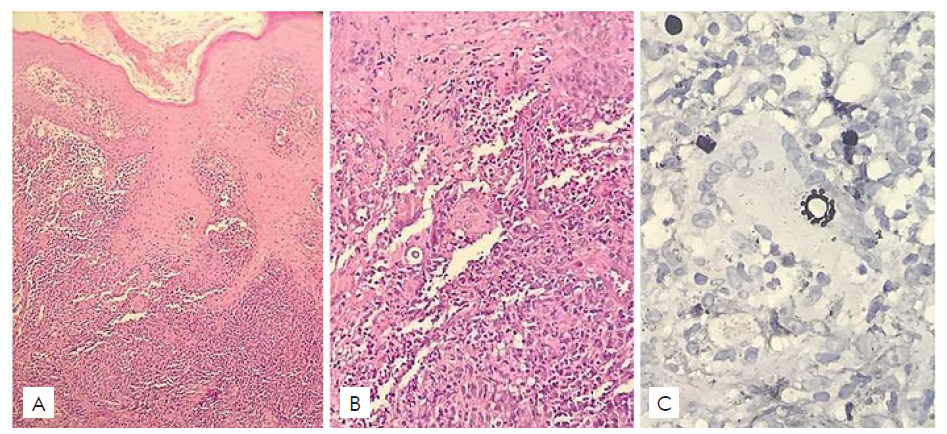
Figure 5 (A) Pseudoepitheliomatous hyperplasia with microabscess intraepidermal and intense mixed and diffuse dermal inflammatory infiltrate (HE 200x); (B): Presence of rounded structures with refringent and thick walls, giving the appearance of a double contour (HE 400x); (C) Inside a multinucleated giant cell is a fungal cell exhibiting multiple peripheral budding distributed over the whole surface, an appearance known as "marine pilot’s wheel" (Grocott 400x).
Treatment with amphotericin B deoxycholate (0.7 mg/kg/day) was started, but suspended after 4 days due to worsening renal function. Itraconazole was then introduced at a dose of 400 mg/day. Despite the suspicion of neoplasia of the biliary tract, after 15 days of itraconazole, the patient progressed with a weight gain of 3 kg, clinical and laboratory improvement, significant involution of adenopathies and skin lesions, corroborating the diagnosis of paracoccidioidomycosis. Due to the excellent response to antifungal treatment, an intra-abdominal biopsy, although indicated, was suspended.
After 30 days of hospitalization, the patient was discharged for outpatient follow-up, with sulfamethoxazole-trimethoprim (800/160 mg) twice daily for 12 months. There was full weight gain and complete regression of skin lesions three months after starting treatment (Fig. 6). Chest radiography and abdominal ultrasound were performed at the end of treatment, which were within normal limits, whereas the serological test for Paracoccidioides spp infection remained negative.
DISCUSSION
PCM is one of the most important deep mycoses in Latin America originally described by Adolfo Lutz in 1908.5 It affects mostly male individuals during their most productive age, between 30-50 years,3,6with higher prevalence among rural workers and gardeners.7,8In addition, alcoholics, smokers and immunosuppressed people have a higher risk of developing the disease, mainly in its severe forms.9,10
The disease is caused by the dimorphic fungi Paracoccidioides brasiliensis and P. lutzii, which at room temperature (4ºC to 28ºC) present the mycelial form and at 37ºC develop as a yeast.7 The infection is acquired via the inhalation of infective propagules, present in the soil of endemic areas.2,4In the lungs, they are transformed into yeast cells that cause infection and can spread to other tissues through the lymphatic and hematogenous routes.8 The higher prevalence among men seems associated the presence of estrogen receptors in the fungus wall, capable of blocking the transformation of mycelia into the infecting yeast form, which explains similar prevalence between genders in the first and after the sixth decades of life.7,8
Acute/subacute paracoccidioidomycosis classically occurs in young patients of both sexes, predominantly in children and adolescents. Eventually it may affect individuals up to 35 years old.6,11It is characterized by compromising the reticuloendothelial system, generating adenomegaly and hepatosplenomegaly, and by causing osteoarticular and cutaneous lesions.5 Lymph node involvement affects predominantly the cervical, axillary and inguinal chains, and fistulization may occur.3 In the literature, the frequency of organs involved is as follows: lymph nodes, digestive tract, liver, spleen, bones, joints and the skin.2 Pulmonary involvement is rare. Constitutional symptoms like fever, anorexia and weight loss occur frequently.4
Skin lesions include papules, plaques, crusts and acneiform lesions, affecting mainly the cephalic segment.6,8Nodular and verrucous lesions with or without ulceration may occur.6 Multiple lesions of the papularacneiform type suggest hematogenous dissemination of fungus and reflect the severity of the disease.8 In the acute/subacute type, mucosal lesions are rare, but papuloerosive lesions with hemorrhagic dots (mulberry-like appearance) may be present in oral and nasal mucosa.3,9,11
Abdominal involvement in PCM is normally seen in the suba-cute form, with a wide variety of clinical manifestations, including nausea, vomiting, weight loss, weakness, pruritus, jaundice, choluria, fecal acholia, ascites, abdominal pain and hepatosplenomegaly.5,12,13Jaundice in PCM is reported as a severe and late manifestation of the disease, which is associated with a poor prognosis.13It is normally caused by extrinsecal compression of the common bile duct by lymph nodes.7 The enlarged intra-abdominal lymph nodes may coalesce, producing solid masses, which mimic intra-abdominal tumors, as in our case.4,13Although not endemic in Northern hemisphere, it should be included in the differential diagnosis of abdominal masses, mainly in patients that have had previous exposure in an endemic area.13
The gold standard for the diagnosis of PCM is the finding of fungal elements suggestive of Paracoccidioides spp. through the examination of fresh sputum or other clinical specimens (lesion sample, lymph node aspiration), culture or biopsy fragment from affected organs.3,4,6According to Moreto et al, sensitivity for direct tissue exam is 74.5%,14 while Marques suggests that sensitivity of culture from biopsy fragments is about 37.5%.10 Both describe the higher diagnostic accuracy of histopathology (positive in 96% to 100% of the cases).10,14These facts may explain the negative mycological examination of our patient, while the fungus visualization was positive in histopathology.
Common histopathological cutaneous findings are epidermal pseudoepitheliomatous hyperplasia with intraepidermal microabscesses. The dermis shows a suppurative granulomatous infiltrate with epithelioid and multinucleated giant cells in association with a mixed acute inflammatory infiltrate. Spores can be found inside giant cells or free in the infiltrate.3,15In the direct mycological and histopathological examinations, P. brasiliensis is observed in its yeast form as a rounded structure, with a double contour and thick wall with single or multiple budding, presenting a pilot’s wheel appearance.3,9
Serological tests can be used in the diagnosis and in the evaluation of response to treatment. Double immunodiffusion is the most recommended method,4 due to its high specificity (about 100%), but false-negative results are not rare due to a sensitivity of 85% to 90%.16 In the reported case, serologies were negative, demonstrating the superiority of the fungus detection in histopathology in relation to serological tests.10
Paracoccidioides spp are susceptible to most systemic antifungal agents. Itraconazole at a dose of 200 mg daily is the treatment of choice for patients with mild to moderate forms of PCM, for 9-18 months. As an alternative, sulfamethoxazoletrimethoprim is the most used drug. For severe forms amphotericin B is recommended, but requires maintenance treatment with itraconazole or sulfamethoxazole/trimethoprim.4,9Cure criteria are based on clinical, radiological and laboratory improvement.3,4
Thus, we report a case of PCM with an exuberant presentation at an unusual age and gender, in which the abdominal involvement simulated a neoplasia of the biliary tract. The importance of the dermatologist is highlighted, who conducted the investigation based on clinical suspicion, in a minimally invasive way, obtaining the conclusive diagnosis of a serious systemic disease through the histopathological study of skin biopsy.