INTRODUCTION
Syphilis is an infectious disease caused by the bacteria Treponema pallidum that is transmitted through direct contact with infected mucosal lesions. It is most commonly transmitted by sexual contact, but it can also be spread congenitally.1-4Thirty percent of sexual partners of recently infected patients develop syphilis.3,5In infected individuals, T. pallidum disseminates within days after infection resulting in early invasion of distant tissues.6 Clinical manifestations are the result of inflammatory responses elicited by the replicating bacteria within the tissues1,4and are highly variable often mimicking those of other diseases.1,4,5If left untreated the disease can progress over years through four stages (primary, secondary, latent, and tertiary) and lead to serious cardiovascular or neurological complications.2-4The primary stage of the infection is classically defined by an asymptomatic, indurated genital ulcer at the inoculation site.3,7Secondary stage usually occurs 6 to 8 weeks after the onset of the primary phase8 and it is the most florid and clinical diverse stage of the disease.5,9It classically features a symmetric, copper-coloured, maculopapular skin rash of any morphology, presenting typically on the palmar and plantar surfaces.3 Verrucous lesions, appearing as moist exophytic plaques, especially on mucus surfaces, referred as condylomata lata, have also been described.7 Syphilis remains a worldwide problem and incidence rates have increased substantially around the world especially in men who have sex with men (MSM) and in human immunodeficiency virus (HIV) infected individuals.3,6,8
CASE REPORT
A 24-year-old Caucasian male patient was observed in our Dermatology Department for a one-month history of mildly pruritic and painful growing perianal skin lesions. The patient was HIV-seropositive, and he was on antiretroviral therapy with regular appointments (CD4 cell count was normal and viral load was undetectable). He referred one sexual male partner in the last 6-months and reported no history of genital ulcer nor other previous skin lesions.
Physical examination revealed multi-lobulated masses in the perianal area forming rubbery, skin-coloured, plaques and masses with a smooth and moist surface (Fig. 1A). Broad-based papillomatous whitish plaques were also observed in the oral mucosa (Fig. 1B). There were no abnormal cutaneous findings on his palms, soles, trunk or extremities, or any sign of concomitant systemic disease.
A 4-mm punch skin biopsy of the perianal lesions and serological tests were performed. T. pallidum antibodies in the patient’s serum were reactive, T. pallidum hemagglutination (TPHA) assay was positive. In addition, rapid plasma reagin (RPR) titer was positive and the Veneral Disease Research Laboratory (VDRL) test was reactive (128 dil). Hepatitis C virus, and hepatitis B virus serology results were negative. Histopathology of the skin biopsy showed irregular acanthosis and papillomatosis, along with endothelial cell swelling and a prominent dermal infiltrate, rich in lymphocytes and plasma cells (Fig. 2A & B). Immunohistochemical stains using antibodies to treponemal antigens allowed the direct detection of the spirochetes (Fig. 2C). A diagnosis of secondary syphilis, presenting as perianal and oral mucous condylomata lata, was made. The patient was treated with a single dose of 2.4 million units IM of penicillin G benzathine and advised to inform the partner for testing and treatment. Lesions resolved completed in 3 months.
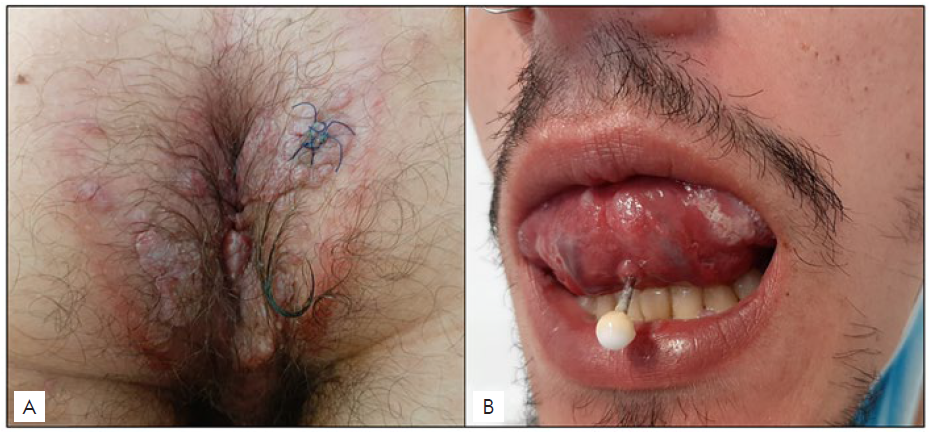
Figure 1 Condylomata lata, clinical picture: (A) Multi-lobulated masses in the perianal area forming rubbery, skin-colored, plaques and masses with a smooth and moist surface; (B) Broad-based papillomatous whitish plaques in the oral mucosa.
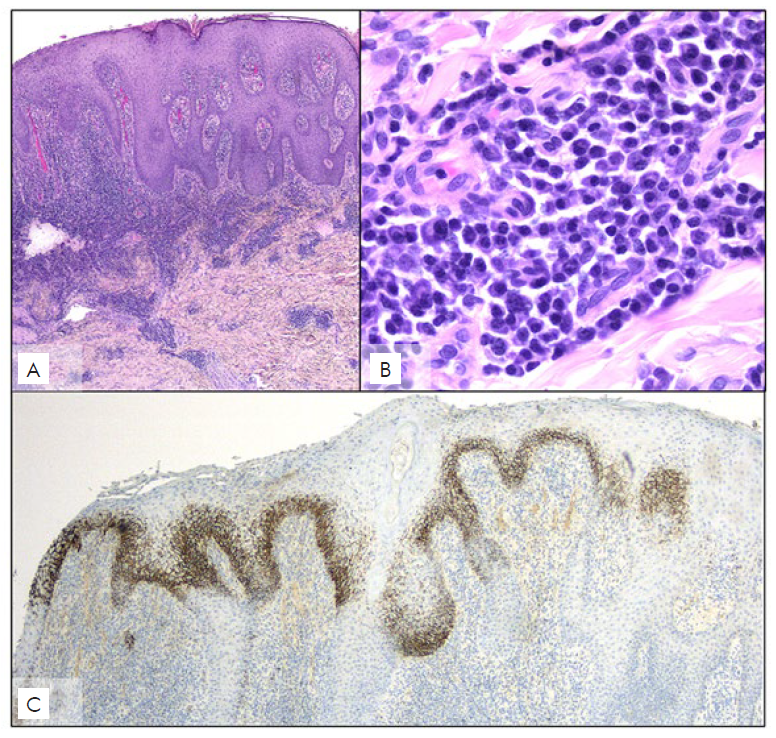
Figure 2 Condylomata lata, histopathological picture: (A) irregular acanthosis and papillomatosis, along with endothelial cell swelling and prominent dermal infiltrate rich in lymphocytes and plasma cells (H&E, x25); (B) Plasma cells are clearly observed within the dermal infiltrate (H&E, x400); (C) Section of the skin biopsy tissue stained with antibodies against treponemal antigens, showing the direct detection of the spirochetes (x40).
DISCUSSION
We reported a case of secondary syphilis presenting solely as extensive condylomata lata lesions in a young male patient with HIV coinfection. Concomitant HIV and syphilis infection is becoming increasingly common since the presence of one infection facilitates the acquisition of the other and both conditions have the same route of infection.5 Besides, preexposure HIV prophylaxis is also contributing to syphilis dissemination among this community, due to decreased condom use.6 This is important because many atypical and, well-characterized but less frequent syphilis presentations have been described in patients with HIV coinfection. This diversity of clinical signs is more common during the secondary stage of syphilis.5,7,9Since syphilis is more common in MSM, a population with also high rates of HIV infection, awareness of these less common presentations that may lead to delayed diagnosis and treatment is important. In our case, the clinical presentation and the sexual history could be suggestive of condylomata lata, although extensive lesions with no other accompanying symptoms are not commonly described.10Condylomata lata, are highly infectious, intertriginous moist papules, typically associated with secondary syphilis, but less frequently observed, reported in 9%-44% of cases.11 They occur mainly on the perianal area and the vulva although atypical locations (palms, face, ankle, umbilicus and toe webs) have been described.12 Differential diagnosis includes verruca vulgaris, condylomata acuminatum, Hailey-Hailey10 and Buschke-Löwenstein tumor.13 Condylomata lata histopathology is variable but a skin biopsy revealing a dense plasma cell infiltrate and spirochetes visualized by silver or immunohistochemical stains confirms the diagnosis.14,15Direct detection of T. pallidum may be used in patients presenting with chancre, condylomata lata or lesions of congenital syphilis however, secondary syphilis diagnosis does not necessarily require histopatholo-gical examination of a skin biopsy.4,15,16In fact, the diagnosis is usually based on the patient’s history, physical examination, and serologic testing that involve treponemal and nontreponemal tests.4,6,15
Treatment recommendations do not depend on HIV status or non-treponemal test titer.15 Patients should be monitored at 6 and 12 months after treatment.
Syphilis remains an important public health and clinical problem with increasing rates among MSM. Besides, frequent co-infection of HIV and syphilis in this population is frequent. Clinicians should keep in mind that in HIV infected patients severe, persistent, and atypical manifestation are more common. The present case shows extensive condylomata lata lesions as the only manifestation of secondary syphilis in an HIV infected patient. A high index of suspicion is essential not to miss the diagnosis.















