WHAT DOES THE STUDY ADD?
This case series shows different acral cutaneous manifestations associated with SARS-CoV-2, including comparison with classical erythema pernio. The recognition and distinction of all these dermatological entities is of paramount importance in the midst of the COVID-19 pandemic.
O QUE O ESTUDO ACRESCENTA?
Esta série de casos apresenta diferentes manifestações cutâneas acrais associadas ao SARS-CoV-2, incluindo comparação com o eritema pérnio clássico. O reconhecimento e distinção de todas estas entidades dermatológicas são de suma importância na fase de pandemia da COVID-19.
INTRODUCTION
In March 2020, coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization. It is widely known that the respiratory system is predominantly affected by COVID-19; however, skin involvement has also frequently been reported.1
Several types of cutaneous manifestations have been identified, such as exanthematous rash, vesiculobullous skin eruptions, urticaria-like rashes, pernio-like lesions, livedo reticularis-like lesions, cutaneous small-vessel vasculitis, and non-inflammatory retiform purpura.2,3The most widely cited mechanisms include overexpression of inflammatory mediators, which releases a large amount of cytokines, damaging the endothelium, formation of multiple microvascular thrombi and changes in the cellular components of the immune system infiltrating vessels by complement activation. Also, SARS-CoV-2 can enter into human endothelial cells via angiotensin converting enzyme 2 (ACE2) receptor and transmembrane serine protease 2 (TMPRSS2) in dermal blood vessels.4
Viral infections are associated with human innate and adaptive im-mune responses that produce inflammation. The activation of mast cells and basophils, either by direct or indirect effect of the virus, is a possible event and it is important to be keenly observant of cutaneous manifestations and hypercoagulable states (e.g., acral ischemia). It seems plausible that the described cutaneous manifestations could be caused by effects on endothelial dermal blood vessels or stimulated by cytokines in arterioles and capillaries due to cytopathic damage associated with SARS-CoV-2 infection. The direct cytopathic effect of SARS-CoV-2 can be present in cases of vesicular or papulovesicular lesions, which resemble those produced by the family Herpesviridae. Skin rashes can also be paraviral owing to cytokines or to drugs used during COVID-19 treatment.4
The cutaneous lesions associated with SARS-CoV-2 can appear before, during, or after systemic symptoms have resolved and they can also occur in asymptomatic patients.1 The acral pattern of pernio-like lesions - acral, erythematous, and edematous lesions, with formation of blisters and pustules - are perhaps the most characteristic cutaneous lesions of COVID-19.5
Most cases of acral lesions have been associated with milder disease, resolving disease, or negative laboratory tests. In addition, acral lesions have also been detected in many close contacts of patients.6
Familiarity with cutaneous manifestations can aid in the early diagnosis and even act as prognostic and epidemiological markers of COVID-19.5,6It is crucial that all health care professionals be aware of these increasingly common cutaneous manifestations of COVID-19.7
The objective of the study was to characterize acral cutaneous manifestations seen in a dermatology outpatient clinic during the COVID-19 pandemic.
METHODS
This is a descriptive study from an outpatient practice in Porto Alegre, Rio Grande do Sul, Brazil, during the COVID-19 pandemic, including patients diagnosed with COVID-19 who presented with cutaneous lesions in the acute infection stage. The diagnosis of COVID-19 was confirmed by real-time polymerase chain reaction (RT-PCR) and also by serologic tests.
A whole-body examination of the patients’ body surfaces was conducted to look for other cutaneous manifestations possibly related to COVID-19. The following data were collected: age, sex, photo-type, place of origin, occupation (healthcare sector or other), aspects associated with COVID-19 (general health status, overweight, comorbidities, fever, general symptoms, need for hospital treatment, and hospital admission), characteristics of the skin lesions (affected topographic area, onset before or after signs/symptoms described for COVID-19, climatic condition at onset, time to progression, related symptoms, semiologic aspects, treatment, investigation method, and first-time manifestation of that type of lesion on that site). The following tests were also included in the investigation: RT-PCR; IgG and IgM for SARS-CoV-2; serologic screening for herpes simplex virus (HSV) with IgG and IgM HSV-1 and HSV-2 antibodies; screening for lupus erythe-matosus with serum markers antinuclear antibody (ANA), anti-double-stranded-DNA-antibody (anti-ds-DNA), anti-SS-A and anti-SS-B antibodies; skin biopsy and lung imaging.
RESULTS
This descriptive case series included eight patients diagnosed with COVID-19 all female, mean age 43.6, all from Rio Grande do Sul, three working in the healthcare sector, who presented with acral cutaneous lesions in the acute stage of COVID-19, with no other associated disease.
In general, the patients had a good health status, with overweight and hypertension reported respectively in one and two patients.
Cutaneous manifestations occurred for the first time and concomitantly with the acute stage of SARS-CoV-2 infection. Lesions appeared after the initial signs and symptoms associated with COVID-19 (the most frequently cited signs and symptoms were: fever, coughing, dyspnea, diarrhea, anosmia, and ageusia). Although all the eight patients seeked hospital care only two had to be admitted to hospital (Table 1).
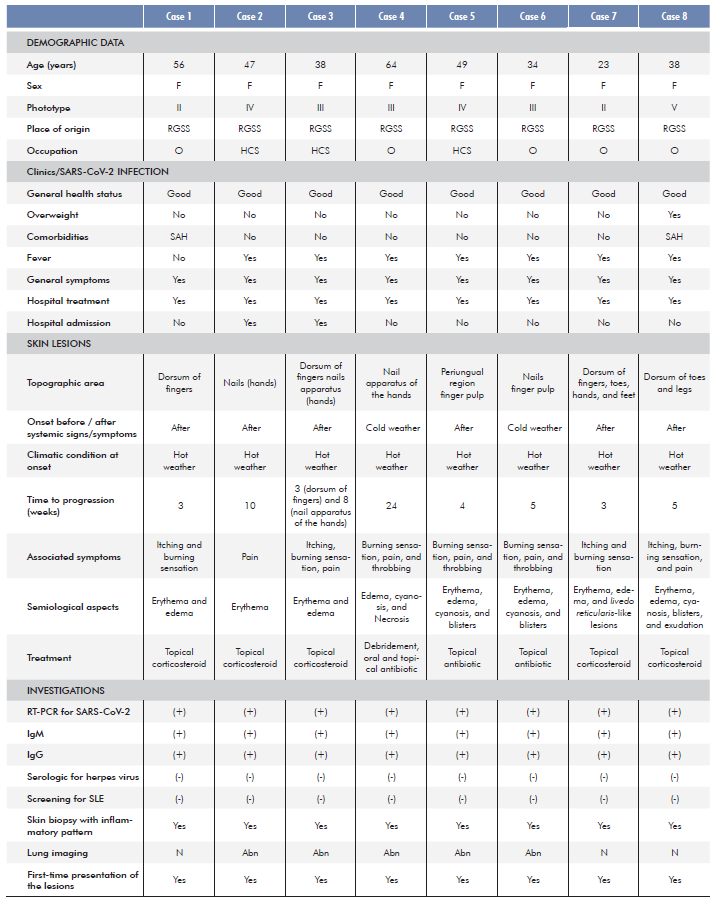
Assessed acral lesions affected different topographic areas, including fingers (dorsum, pulps or periungual), toes, and the nail apparatus. Semiologically, there were mild manifestations such as erythema, livedo reticularis-like lesions, and edema, and in four also more severe lesions with blister formation, cyanosis, vasculitis and necrosis (Fig. 1). Symptoms included burning sensation, itching, and throbbing pain.
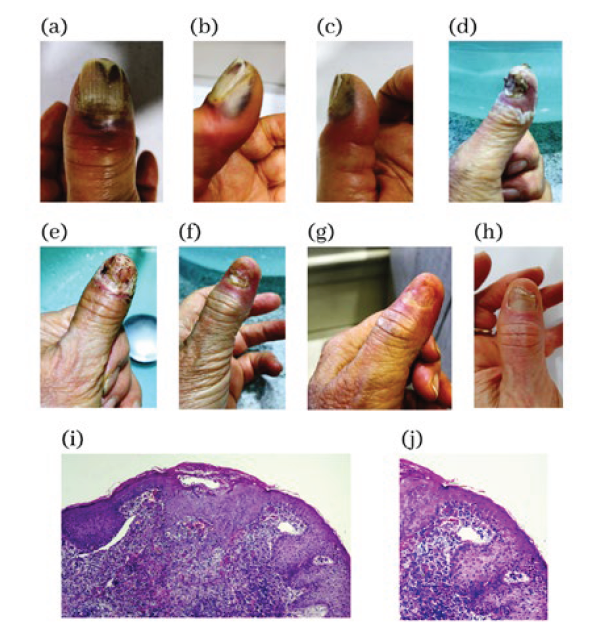
Figure 1 Manifestations of ischemia and necrosis in the fingers that appeared during the infection by SARS-CoV-2. Sequence of photos (a), (b), (c), (d), (e), (f), (g) and (h) from the beginning to the recovery phase. Histological images of nonspecific lymphocytic inflamma-tory infiltrate (i) 100x and (j) 400x, both in H/E stain.
Those patients who presented with pernio-like lesions reported that the lesions developed in periods of hot weather and denied having had those or similar lesions before (Fig. 2). Patients with lupus erythematous-like lesions and herpetic whitlow-like lesions tested negative for these conditions. Among nail disorders, half-moon shaped erythematous bands around the distal margin of the lunula were a peculiar finding (Fig. 3). The most severe skin lesions were not necessarily associated with more severe respiratory infections caused by SARS-CoV-2.
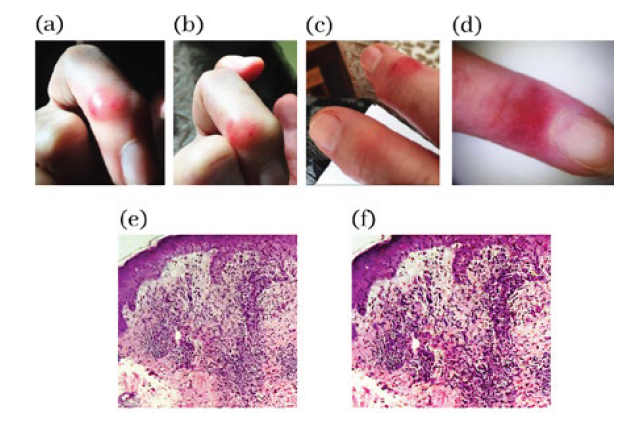
Figure 2 Finger lesions with violaceous erythema and edema that occurred during the infection by SARS-CoV-2 (a), (b), (c) and (d). Histological images of nonspecific lymphocytic inflammatory infiltrate (e) 100x and (f) 400x, both in H/E stain.
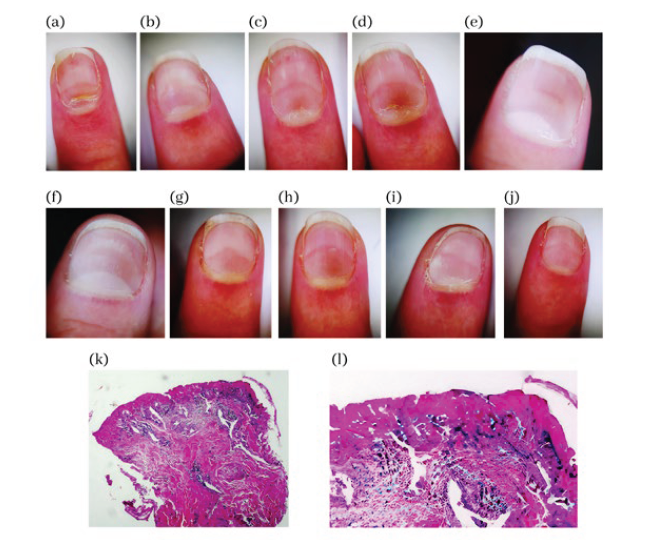
Figure 3 Unusual manifestations in nails with erythematous arches that appeared during SARS-CoV-2 infection. Left hand fingers: (a) = fifth, (b) = fourth, (c) = third, (d) = second and (e) = first. Right hand fingers: (f) = first, (g) = second, (h) = third, (i) = fourth and (j) = fifth. Histological images of nonspecific lymphocytic inflammatory infiltrate (k) 100x and (l) 400x, both in H/E stain.
The lesions were biopsied and revealed lymphocytic infiltrate in the perivascular papillary dermis and reticular dermis, edema, and signs of endothelial activation, and necrotic keratinocytes. Among patients with abnormal lung imaging findings, some had normal chest radiographs, but computed tomography (CT) revealed ground-glass opacity in 5 patients, leading to the diagnosis of interstitial pneumonia. No fatality occurred in this group and COVID-19 resolved within 30 to 90 days.
DISCUSSION
Clinically, pernio-like erythematous lesions consist of macules, papules, plaques or blisters, and usually show a clearly defined border in the metatarsophalangeal and interphalangeal region, generally affecting the feet and, to a lesser extent, the hands. Lesions look purplish or bluish at first but can develop into blisters or crusts in the course of disease, and they sometimes look like vasculitis or erythema multiforme,8 as in our cases 7 and 8 (Fig. 4).
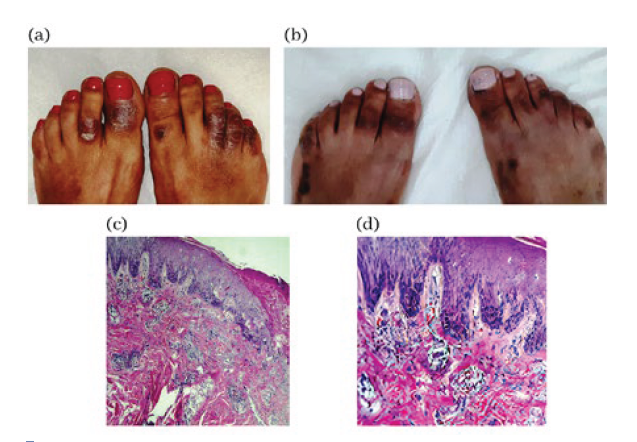
Figure 4 Acral inflammatory lesions with violaceous erythema, ede-ma and blisters that appeared during the SARS-CoV-2 infection. (a) = initial condition, (b) = evolution with residual hyperchromic areas. Histological images of nonspecific lymphocytic inflammatory infiltrate (c) 100x and (d) 400x, both in H/E stain.
Skin rashes often present as purplish erythematous papules, macules, or nodules, and their pathogenesis is not fully understood. An underlying mechanism could be cold-induced vasoconstriction and vasospasm, resulting in hypoxemia and inflammation. Other hypotheses suggest hyperviscosity or autoantibody-induced endothelial damage. A study suggests that “immune dysregulation, vasculitis, vascular thrombosis, or neoangiogenesis”9play a role in the pathophysiology of skin rashes.
Treatment modalities include heat, nonsteroidal anti-inflammatory drugs (NSAIDs), topical corticosteroids, and vasodilators.10
Our case series is in line with literature findings, as several studies consider acral cutaneous lesions as probably the most characteristic skin lesions of SARS-CoV-2 infection. Our study also supports that pernio-like erythematous lesions are associated with COVID-19, given that acral cutaneous lesions occurred at hot temperatures rather than in wintertime, which is more usual.6 Erythema pernio usually occurs only in winter at low temperatures in the State of Rio Grande do Sul, but that was not the case because cutaneous lesions developed during the pandemic in hot weather. Furthermore, no patient reported a previous history of pernio-like erythema during cold weather and SARS-CoV-2 infection was confirmed in all of the patients by PCR.
The prevalence of acral lesions varied considerably among stu-dies. An international case series with 505 patients with skin conditions showed a 63% prevalence for pernio-like lesions.11 As in our study, pain and itching were the dermatologic symptoms more frequently associated with the lesions.11-15
Moreover, as we described (Fig. 3), convex erythematous half-moon bands around the distal margin of the lunula associated with pain were also reported in the literature in a 60-year-old female patient who had a similar clinical course 2 weeks after the onset of symptoms. Nonetheless, she denied having any associated symptoms and no other cutaneous manifestation was observed. After follow-up of 1 month, the bands were still present and they were wider. The pathogenesis of this half-moon-shaped lesion after SARS-CoV-2 infection is unknown, and it had not been previously described in other systemic diseases. A localized microvascular lesion secondary to an inflammatory immune response and a procoagulant state may play a key role. Considering the anatomic site, possible damage to the capillary network of the distal subungual arcade was inferred.16
Livedo reticularis-like lesions appear to be one of the least common cutaneous manifestations during the COVID-19 pandemic and we described an acral case in association with erythema pernio-like lesions (Fig. 5). In a study of 375 patients with cutaneous manifestations who had tested positive for COVID-19, only 6% showed variable degrees of livedo reticularis-like lesions and necrosis.6The anatomic site of those lesions includes the trunk, forearms, and dorsal hands and feet.6,9The lesions occurred concomitantly with other COVID-19 symptoms and affected mainly older patients with more severe infections. A Spanish case series demonstrated a 10% mortality rate (the highest rate among all cutaneous manifestations) in patients with livedo reticularis-like lesions.6
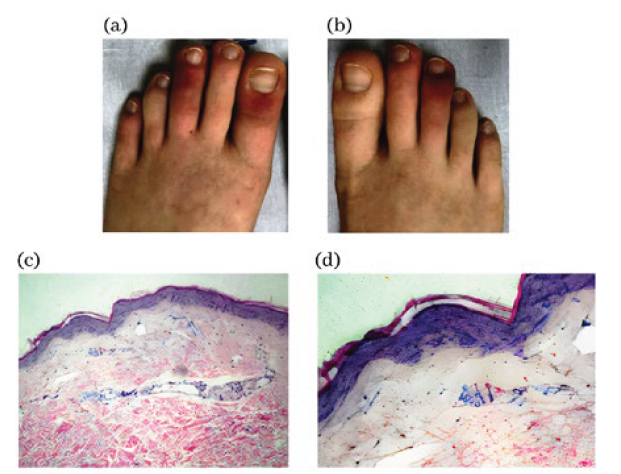
Figure 5 Acral lesions with cyanosis and livedo arising during infec-tion by SARS-CoV-2. (a) = left foot and (b) = right foot. Histological images of nonspecific lymphocytic inflammatory infiltrate (c) 100x and (d) 400x, both in H/E stain.
The histopathological findings of skin lesions showed varied and nonspecific inflammatory aspects. However, the clinical features of the acute dermatological lesions occurring in patients with COVID-19 support this association reported since the beginning of the pandemic. Nevertheless, despite the lack of specific histologic markers for SARS-CoV-2 and the need to determine a cause and effect relationship, investigation plays an important role in differential diagnosis (in the present study, our investigation ruled out other acral disorders such as seen in systemic lupus erythematosus and herpes virus infection).
According to the literature, the histopathologic analysis of skin lesions in COVID-19 cases may reveal different patterns. In cases of SLE-like acral lesions and herpetic whitlow-like, the histologic analysis showed focal vacuolar degeneration of the basal layer. Degenerative changes were also observed within the epidermis with perivascular lymphocyte cuffs. The histologic analysis of another sample revealed the presence of perivascular neutrophil cuffs with clear endothelium inflammation and areas of epidermal necrosis.8 In another study, whose findings were consistent with ours, there was lymphocytic infiltrate (predominantly perivascular) in the papillary dermis and reticular dermis, occasionally associated with edema and signs of endothelial activation.17
Other studies found granular positivity of spike protein in dermal endothelial cells and epithelial cells of eccrine glands of a patient with chilblain-like lesions and SARS-CoV-2. Therefore, the detection of SARS-CoV-2 components in eccrine glands - corroborated by the notion that the closely related SARS-CoV is also present in sweat glands - indicates sweat as a possible source of contagion.18,19
CONCLUSION
Cutaneous manifestations associated with COVID-19 have been increasingly described in the literature, but their actual incidence has not been estimated so far and their pathophysiological mechanisms re-main largely unknown; furthermore, the direct or indirect role of SARS-CoV-2 in their pathogenesis is still under discussion. Evidence shows that cutaneous manifestations associated with COVID-19 are extremely polymorphic, but there are some attempts to classify them into groups according to their patterns, and possibly according to the severity of COVID-19.15
Even though there are no specific histologic markers for SARS-CoV-2, nor a well-established cause and effect relationship between this new virus and cutaneous manifestations, we believe that, after history taking and thorough physical examination, laboratory tests, and imaging exams, the acral lesions reported herein might have occurred as a consequence of SARS-CoV-2 infection. Theoretically, the mechanism of induction of cutaneous lesions could also be related to hyper-sensitivity reaction to the virus determining the emergence of the lesions is a reasonable possibility.20
Anyway, cutaneous manifestations and their pathogenesis in COVID-19 patients need further evidence and investigation.4 We be-lieve the investigation into these lesions and their accurate identification could even help with the diagnosis of COVID-19 and maybe, in some cases, allow an earlier diagnosis, thereby improving patient manage-ment and reduction of viral spread.