INTRODUCTION
Zoon balanitis (ZB) is a benign chronic inflammatory mucositis of the genital mucosa that usually presents in middle-aged to elderly men. It is characterized by a solitary well-circumscribed erythematous plaque affecting the glans penis and prepuce.1
ZB etiology is still unclear, but poor hygiene and chronic irritation from warmth or rubbing have been proposed. Therefore, it may complicate other affections of the glans penis or foreskin in uncircumcised men such as lichen sclerosus (LS).2
Herein, we report a case of synchronous presentation of ZB and LS.
CASE REPORT
A 70-year-old uncircumcised male with a past medical history of hypertension presented with a six-month history of pruritic lesions on the glans penis. He complained of difficulty in retracting the prepuce. There was no clinical improvement with topical fusidic acid, mid-strength potency corticosteroids and oral antibiotics.
On physical examination, a well-demarcated erythematous shiny plaque involving the glans, coronal groove and proximal foreskin was observed (Fig. 1-A). The remaining glans mucosa was hypopigmented, thin and wrinkled, with focal erosions and purpu-ric macules (Fig. 1-B). Foreskin was thickened leading to phimosis.
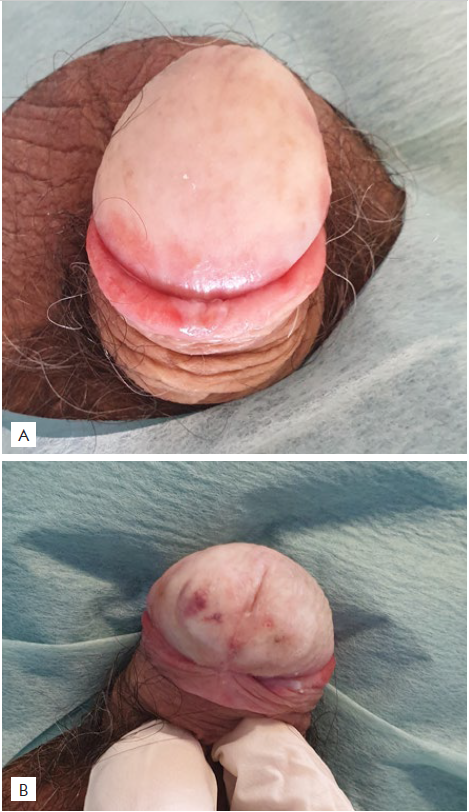
Figure 1 (A, B) - Hypopigmented, thin and wrinkled glans with focal erosions and purpuric macules associated with a well-demarcated erythematous shiny plaque involving the glans, coronal groove and proximal foreskin
Histopathological examination of a biopsy of the erythematous plaque showed a dense band-like infiltrate of plasma cells in the submucosa, extravasation of erythrocytes and hemosiderin pigment laden macrophages (Fig. 2 A-C). In contrast, a biopsy of the remaining glans revealed orthokeratotic hyperkeratosis, acanthosis, focal basal cell vacuolar degeneration, submucosal edema and a superficial, dense, band-like lymphocytic infiltrate (Fig. 3 A-B). The diagnosis of ZB associated with LS was established.
The patient was treated with topical clobetasol propionate 0.05% once daily for three months without clinical improvement. He was then circumcised with significant improvement of both conditions after six months.
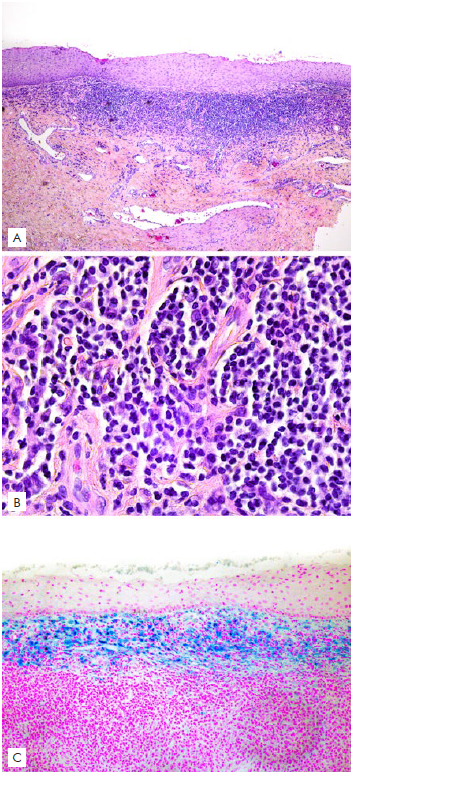
Figure 2 (A, B, C) - Histopathology of the erythematous plaque. A) A dense band-like infiltrate of plasma cells in the submucosa, vaso-dilatation /ectactic vessels in the deeper dermis and extravasation of erythrocytes (H&E- 40x) B) Detail of the inflammatory infiltrate in the upper dermis, which has almost only plasma cells (H&E- 400x); C) hemosiderin deposits in the submucosa (Perls' Prussian blue iron stain- 100x).
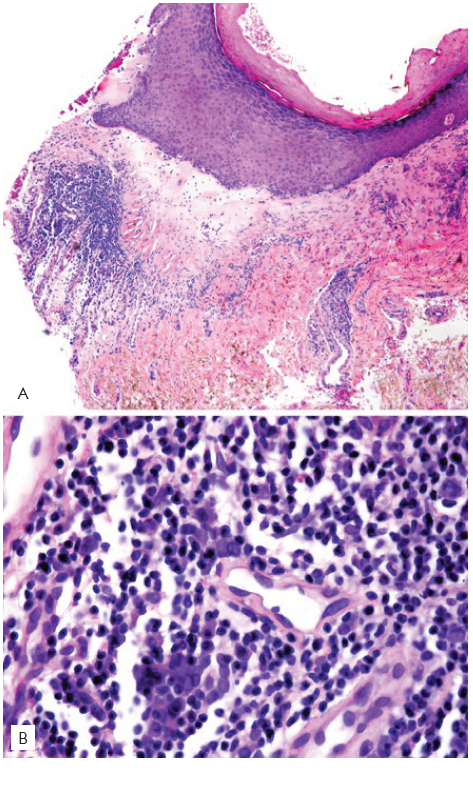
Figure 3 (A, B) - Histopathology of the glans biopsy in a hipopigmented area. A and B: orthokeratotic hyperkeratosis, acanthosis, focal basal cell vacuolar degeneration, submucosal edema and a superficial, dense, band-like lymphocytic infiltrate (A-B: Hematoxylineosin stain; original magnifications: x40, x400).
DISCUSSION
ZB and LS are both chronic inflammatory disorders of the genital mucosa, usually affecting middle-aged or elderly uncircumcised men. Both conditions can cause sexual and urinary dysfunction in men and have a significant impact on the quality of life.1 ZB usually presents as erythematous discrete shiny moist plaques on the glans mucosa and, less commonly, on the foreskin or on the coronal groove. Multiple pinpoint, brighter red spots may be speckled on the background of these plaques with a “cayenne pepper” appearance. When both glans and opposing foreskin are involved the lesion can acquire a “kissing” aspect. Sometimes patients report pruritus, dysuria, pain or a burning sensation.2In contrast, male genital LS presents as atrophic and pale or violaceous plaques with telangiectasia and purpura often involving the glans mucosa, coronal sulcus and foreskin. Patients usually report dyspareunia and painful erections. Tightening of the foreskin may lead to phimosis. Involvement of the perimeatal area and meatus may cause scarring leading to stenosis and urinary obstruction.3
The differential diagnosis in this case included ZB, LS, erythro-plasia of Queyrat, psoriasis and lichen planus. Glans biopsies in two different sites showed typical features of both ZB and LS.
First-line treatment of male genital LS is a course of topical clobetasol propionate 0.05% once daily for up to three months. Topical steroids are also the mainstay of treatment for ZB. Promotion of good hygiene is an important adjuvant measure in ZB. In selected cases, intralesional steroids, topical calcineurin inhibitors, CO2 laser and photodynamic therapy can be used in the treatment of both conditions. Surgical treatment with circumcision is reserved for refractory cases or complications such as phimosis and is usually curative for both disorders.3,4
The association of ZB and LS is scarcely reported in the literature. To the best of our knowledge, only three cases with clinical and histopathologic features consistent with synchronous presentation of both disorders have been published.5
Several authors have suggested a pathogenic role of irritant and mechanical triggers in ZB pathogenesis. The improvement after circumcision supports a pathogenic role of poor genital hygiene.2 Foreskin sclerosis and phimosis caused by male genital LS may be responsible for urine retention between glans and foreskin, with local maceration and humidity, which can trigger ZB.5
In conclusion, dermatologists should be aware of the possible association between ZB and LS. Skin biopsies from different topographies may be required to establish both diagnoses.















