INTRODUCTION
Trichilemmal horn or trichilemmal keratinization is considered a benign and very rare neoplasm,1 characterized in the histopathology by an abrupt maturation of keratinocytes in lamellar keratin without the formation of the granular layer, occurring in the outer sheath of the hair follicle root and in the trichilemmal sac of the catagen and telogen wires.2 The prevalence is higher in women and in the age groups older than 50 years, with a predominance in extremities followed by the cephalic region.1-3Its etiopathogenesis remains uncertain,3 however there are reports of its occurrence secondary to the rupture of a previous trichilemmal cyst.3 The diagnosis is confirmed after excision and histopathological analysis, showing specific characteristics of this pathology.
CASE REPORT
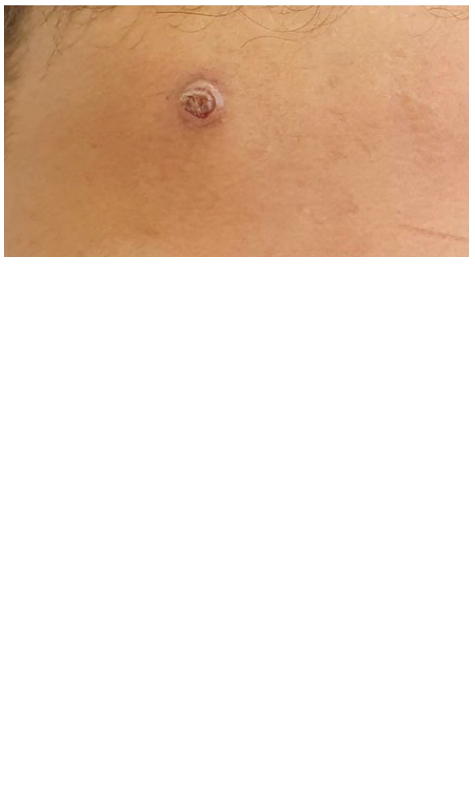
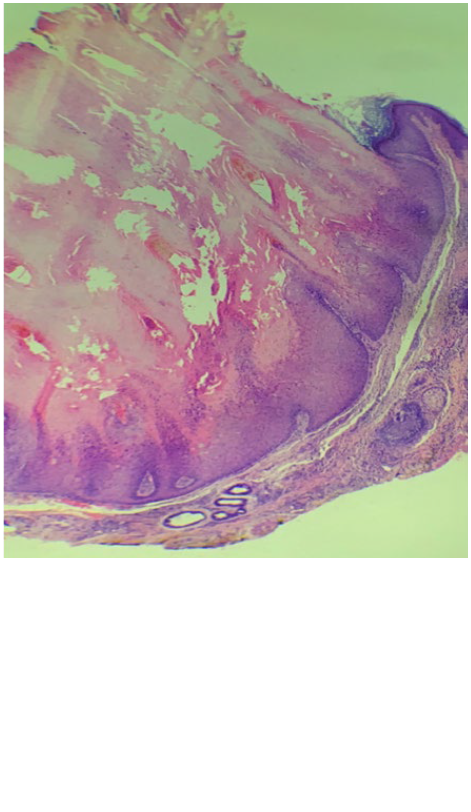
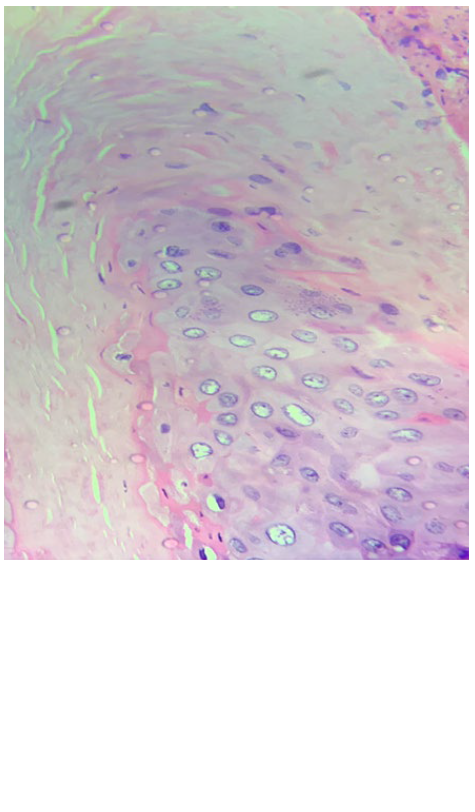
A 14-years-old male, attended the dermatology clinic at Heliópolis Hospital Complex, São Paulo, referring the appearance eight months before of an asymptomatic papular lesion on the forehead without association with trauma or local procedures. He reported progressive growth with no change in the characteristics of the lesion. On dermatological examination, there was a well-defined papule with an exophytic keratotic center, measuring approximately 1 cm (Fig. 1). Initially, keratoacanthoma, traumatized verruca vulgaris and cutaneous horn were considered as possible diagnoses. After surgical excision the anatomopathological analysis stained by the hematoxylineosin (HE) showed a well-limited lesion where the epidermis had thick hyperortokeratosis and papillomatosis, with compact keratinization without the presence of a granular layer. The more superficial keratinocytes, unlike what would be expected in the more superficial layers, had bulky and vesicular nuclei (Fig.s 2,3 and 4), but no atypia, which is consistent with the diagnosis of a trichilemmal horn. In the dermis, vascular ectasias and fibrosis are observed with no significant inflammatory infiltrate.
The patient returned 45 days after the excision for reassessment, showing complete resolution of the condition.
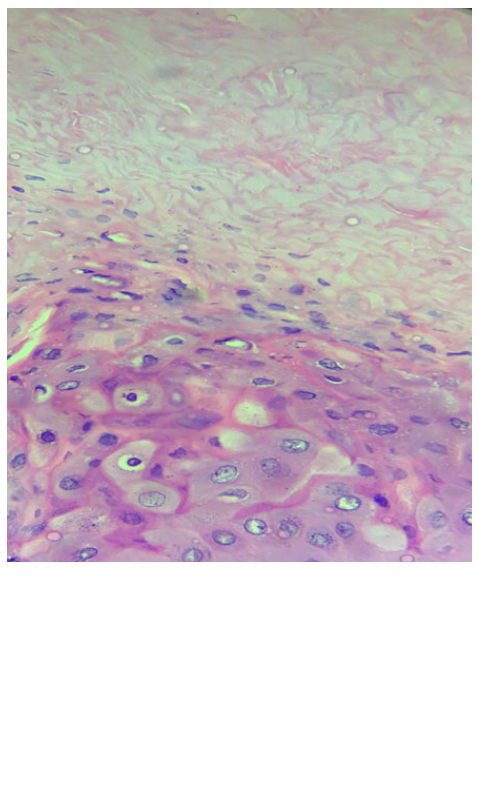
Figure 3 HE 200x. Hyperortokeratosis compact, without interposition of the granular layer. Superficial keratinocytes with large nucleus.
DISCUSSION
Trichilemmal horn is an uncommon lesion with a unique histology, characterized by an area of papilomatous epidermis with the absence of the granular zone, giving rise to a compact, eosinophilic and orthokeratotic keratin, thus characterizing trichilemmal keratinization. There may be nodular extension to the dermis, but inflammation in this location is usually absent,1,2as in the present case.
The etiopathogenesis remains uncertain and the participation of the human papilloma virus (HPV) in this process has been suggested, as previous microscopy studies showed intranuclear particles with morphology similar to HPV, however immunohistochemical studies with anti-HPV antibodies were negative.1 The CD34 antigen is a specific marker for external sheath of the hair follicle and tumors derived or differentiated for this type of epithelium are positive, as in the cases described as trichilemmal horn.2,3
Some cases reported the appearance of trichilemal horn after rupture of trichilemal cysts,3 which was not the case of our patient.
Macroscopically, the lesion is characterized by an exophytic and keratotic lesion, measuring approximately 1 to 2 cm in diameter.1 The prevalence is higher in women and in the age group after 50 years, however cases have been described in ages ranging from 16 to 72 years. Lower limbs, followed by the head and back are the most affected regions.1-3As there is a higher prevalence in body extremities and cephalic region (photoexpo-sed areas), the direct or indirect contribution of ultraviolet (UV) radiation to the disease pathogenesis in some patients has been discussed.2
The diagnosis is made through macroscopic analysis and microscopic examination of the lesion, through excision and anatomopathological analysis.3 Possible differential histological diagnoses of the trichilemmal horn are hypertrophic actinic keratosis, keratoacanthoma, seborrheic keratosis, trichilemal cyst, trichilemoma and verruca vulgaris,2 among others.
In the case of the aforementioned patient, both the macroscopic lesion and the anatomopathological characteristics were con-sistent with the changes described in trichilemmal horns, as well as the location of the lesion, however it diverged from the literature data in relation to age (14 years) and sex.
We decided to report this case as the trichilemmal horn is an uncommon lesion, having as differential diagnosis frequent lesions in the daily dermatological routine and there is very little data in literature about this pathology.