Introduction
Benzodiazepines (BDZ) are widely used to control symptoms in insomnia and anxiety disorders both in primary and secondary healthcare,1-4 and it is estimated that only 20-30% of the prescription of these drugs in the elderly is adequate.5-6
Despite being effective and generally well-tolerated,5 BDZ chronic use is controversial because they have long-term additive potential6 and because of some chronic use has been associated with side effects.7 In geriatric patients, in addition to the concern with daytime hypersomnolence, there is also evidence of association with increased risk of falls, cognitive decline, and delirium1,8 and may be responsible for important restrictions on mobility and daily living activities.9-10
The chronic use of BDZ was also associated with a significant increase in mortality from all causes in the general population,11-12 which brings relevance to all the strategies developed to reduce its inadequate chronic prescription.
In 2015 the Canadian Agency for Drugs and Technologies in Health issued recommendations to implement strategies to the deprescribe chronic prescription of BDZ.13 Current knowledge points to short-term use of BDZ3 and these recommendations are also addressed by rule 005/2011, updated on 01/21/2015 by the Portuguese Directorate-General of Health.14
In this context, there is a need to test and evaluate strategies to promote the rational prescription and deprescription of BDZ, avoiding its prolonged use, as well as the development of algorithms to guide these therapeutic interventions.15 Within the scope of prescription, there are several guidelines and recommendations,15-19 however, chronic/long-term use remains a common practice, even in the elderly population.4,17
Some scientific papers present success rates for interventions to deprescribe BDZ in the elderly reaching 27-80%, but the sustainability of the benefits remains unclear.20 Thus, strategies that involve training and education of health care professionals can be an important contribution to improving the quality of prescription and deprescription.
The primary outcome of this study is to evaluate the effectiveness of a structured intervention in the rational prescription/deprescription of BDZ among the geriatric population.
Methods
A randomized controlled clinical trial involving family physicians (FP) from two Family Health Units (FHU) was developed.
Before starting the trial, FHU C had 2,892 patients above 65 years, 57.9% female, 26% with chronic prescription of BDZ.
FHU I had 2,510 patients above 65 years, 58.6% female, 27.24% with chronic prescription of BZD.
The structured intervention was defined as:
I. Two training sessions on rational prescription and deprescription of sedatives and hypnotics in the elderly.
II. Presentation and introduction to the use of a benzodiazepine description algorithm.
III. Bi-monthly meetings to discuss clinical cases.
Two FHU from the same health centre were randomized (FHU I and FHU C) and the FP working on each FHU received the structured intervention or were selected to be in the control group. A simple drawing was carried out, using computer software, with the supervision of an external element to the investigation.
FHU I’s doctors received the structured intervention.
FHU C’s doctors were allocated to the control group, receiving only two training sessions on rational prescription and deprescription of sedatives and hypnotics in the elderly.
I. Training sessions on rational prescription and deprescription of sedatives and hypnotics
Two training sessions were planned side by side, both for a FP and a psychiatrist. Each training session lasted approximately one hour. In the first one, it was explained the pathophysiology of insomnia in the elderly and the basis for the rational prescription of sedatives and hypnotics. In the second one, some strategies for the prescription and deprescription of sedatives and hypnotic drugs in the elderly were addressed. FP, either from the intervention group or the control group, took part in each training session at the same time. Although there is also a chronic prescription of BDZ for the treatment of symptoms of anxiety disorders, it was decided to focus training on insomnia because it represented a highly frequent reason for BDZ prescription in elderly patients.
II. BDZ’s deprescription algorithm
Based on the “Annex I of Therapeutic Bulletin no. 1/2018, Strategies for the Discontinuation of Benzodiazepines - Pharmacy and Therapeutics Commission from Lisboa and Vale do Tejo’s Regional Health Administration” (available at https://www.arslvt.min-saude.pt/uploads/document/file/3021/Anexo_I_Set17__Estrat_gias_para_a_descontinuacao_de_benzodiazepinas.pdf) and the flowchart adaptation of the previous document (available at https://www.mgfamiliar.net/wp-content/uploads/benzodiazepinas-2.pdf) a BDZ’s deprescription algorithm was presented and discussed at the FHU I.
III. Meetings to discuss clinical cases
In collaboration with a psychiatrist, four meetings were held during the study period. Each session lasted about one hour and a half and there were discussed elderly patients’ daily clinical cases referring to BD. They took place in February, April, June, and August 2019.
FHU I’s FP were instructed to collect situations that appeared to be challenging, either due to the need to introduce hypnotic/sedative drugs or to difficulties in the application of deprescription strategies. Every two months maintaining collaboration with the psychiatrist, FP gathered around and discussed their clinical cases in order (to try) to streamline solutions.
The effectiveness of studies’ intervention was accessed by the Portuguese health performance indicator ‘Proportion of elderly people without prolonged prescription of anxiolytics, sedatives and hypnotics’21 obtained from the online platform - BI of Primary Health Care (Bilhete de Identidade dos Cuidados de Saúde Primários) monitored by the Ministry of Health.
This indicator expresses the proportion of registered patients aged 65 or over without prolonged prescription of anxiolytics, sedatives, or hypnotics. The numerator includes: count of registered users without prolonged prescription of anxiolytics, sedatives, or hypnotics. The denominator: count of registered patients aged 65 or over (technical specifics of the indicator calculation available through the link https://sdm.min-saude.pt/bi.aspx?id=297&clusters=S).
The intervention lasted nine months, from January to September 2019.
Statistical analysis was performed using SPSS for Mac v. 24.0. Descriptive analysis of the data from the two FHU was carried out. Data had also been analysed considering each FHU as a sample by clusters of the population of elderly users of the Regional Health Administration Centre (the institution responsible for the surveillance of health care delivered to patients managed by all Health Centres from the central region of Portugal), thus determining the odds ratio for that same population.
The study was approved by the Regional Health Administration Ethics Committee.
Results
FPs in FHU I was 80% female, with a mean age of 44.0 years (min 38, max 61) and a mean time of practice as FP of 17.6 years.
FPs in FHU C were 40% female, with a mean age of 49.2 years (min 37, max 64) and a mean time of practice as FP of 19.4 years.
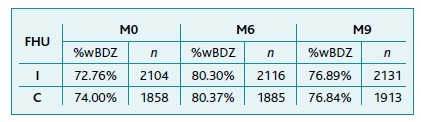
The data obtained refers to the totality of the observations in two FHUs during the nine months of intervention. In Table I it is observed that over the nine months of the study the percentage of elderly users without prescription of BDZ is similar in both FHU I and C with 72.76% and 74.00% respectively. In the evaluation carried out after six months of intervention, both the control and the intervention unit registered an improvement in the indicator (80.3% and 80.37% respectively), and at the end of the ninth month, despite a slight decrease in the indicator, both units have a higher value than what was recorded at the beginning of the study (76.89% and 76.84%).
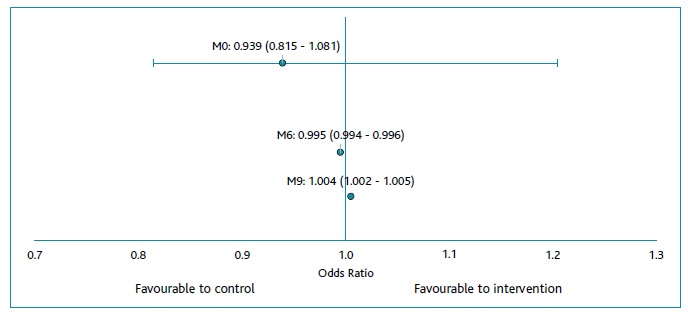
Considering that these data constitute a cluster sample of the elderly population of elderly users of the Regional Health Administration Centre in the Centro Region, it is possible to determine the confidence interval for that same population. Thus, it appears that the probability of an elderly person not having a benzodiazepine prescription was initially similar in the two FHUs (OR [0.815, 1.081, IC95) (Figure 1). After six months of intervention, the probability of not having a BDZ prescription was higher (0.5% more likely) in FHU C (OR [0.994, 0.996], IC95). After nine months, the probability of not having a BDZ prescription was higher in FHU I (OR [1.002, 1.005], IC95). The probability of not having a prescription for BDZ was, on average, 1.004 times higher (about 0.4%) in the FHU I than in the control FHU C.
Discussion
It has been shown that a structured intervention based on the training of health professionals (tool to deprescribe and clinical meetings) can be beneficial in improving the profile of chronic BDZ prescription in elderly users. As far as the authors are aware, there are no studies that have used the same type of intervention, however, when we compare the results in the literature for other BDZ deprescription interventions, the result we obtained was modest.22 Nevertheless, unlike other interventions analysed, this one was structured to integrate the usual routine of family physicians, having an impact on their day-to-day clinical practice, which leads us to believe that these values, although modest, may be more consistent than others referred to in the literature.
We believe that the allocation of research to solve everyday problems must be highlighted. The chronic benzodiazepine prescription is a problem that causes great concern, especially when considering the geriatric population. Secondly, the singular role of multidisciplinary collaboration in the attempt to solve clinical problems must also be emphasised. This intervention proved to be feasible and, although it has a modest impact, it was considered by professionals as an engine for improving clinical practice and allowed the empowerment of clinicians in a demanding and difficult to handle the topic.
This study has some limitations that should be described, starting with its methodology. The samples are not paired, but they are also not independent at different times. For statistical analysis, the two samples were treated as independent, however, it should be noted that, as the sample is extremely high, the confidence intervals obtained are extremely small, thus it is easily obtained a statistical significance that may not correspond to reality.
Another important limitation concerns the lack of data about patients who were deprescribed. In fact, we collect no information about the diagnosis responsible for BDZs’ chronic prescription, mean age, gender prevalence, meantime of BDZ use, and other relevant demographic or clinical variables of patients deprescribed. This information would allow an eventual analysis by cluster, making the interpretation of the results obtained clearer.
Efforts should be performed to create better and more reproducible study methodologies since this is the main reason for the lack of reliability of the results in studies on this topic.22 In this study, instead of analysing the listed indicator, we believe that we improve the quality of the collected data by calculating a sample of elderly individuals and analyse, at each evaluation moment, whether they have or have not BDZ prescription. It would also be interesting to consider a qualitative analysis with the professionals in order to understand if there are other difficulties/barriers to the deprescription of BDZ, thus contributing to improving the complex intervention and, eventually, maximising its impact.
Finally, the analysed indicator refers to the prescription of hypnotics and not just BDZ, however, considering the predominance of BDZ’s prescription when compared to other drugs, we believe that the error associated is small enough not to change the validity of our findings.
Conclusion
After a nine-month structured intervention, the probability of not having a prescription for BDZ is, on average, 1.004 times higher in the FHU I where there was an intervention, Therefore, it demonstrates that this intervention can be beneficial in reducing the prescription of BDZ in elderly patients managed in primary care. Bearing in mind the limitations of the work, the values must be analysed with caution, however, considering the importance of the topic and the apparent positive sense of the results, we believe that other studies, methodologically optimized, can deliver an important contribution to address this problem.
Authors contribution
Conceptualization, C.S.C., A.R-M. and C.F.R.; methodology, C.S.C., A.R-M., B.O. and C.F.R.; formal analysis, C.S.C. and B.O.; investigation, C.S.C., P.O., M.L.; writing-original draft preparation, C.S.C.; writing-review and editing, C.S.C., A.R-M, P.O., M.L., B.O. and C.F.R. All authors have read and agreed to the published version of the manuscript.