Background
Onychomadesis is characterised by a proximal separation of the nail plate from the matrix as a consequence of temporary cessation of nail growth, ultimately leading to nail shedding. Matrix arrest may result from multiple varieties of aetiologies, namely, autoimmune diseases, medications (chemotherapy, carbamazepine, valproic acid, penicillin, azithromycin, tetracycline, fluoroquinolone, chlorpromazine), major medical illness, trauma, exposure to chemicals, iron and vitamin deficiencies, skin affections such as psoriasis, infections (fungal, viral), among others.1-2
One of the most studied viral infections associated with onychomadesis is a hand-foot-and-mouth disease (HFMD), which is a common infection mainly affecting children. HFMD classically presents as a self-limited febrile illness with malaise, oral ulcerations, and a vesicular exanthema, typically on the hands and feet. Delayed manifestations following HFMD may be seen in the form of Beau’s lines and onychomadesis. 1-2 In the year 2000, the association between onychomadesis and HFMD was first described in Chicago, 3 and since then reports on the latter association have been described in other countries or regions.
In childhood, it is not common to observe nail abnormalities. In such instances, it may result in inadequate treatments, unnecessary investigations, and referrals. Therefore, it is of extreme importance that clinicians invest in a detailed patient’s anamnesis, including the assessment of previous viral infections.
To the authors’ knowledge, this is the first case in the literature reporting the association between onychomadesis and hand-foot-and-mouth disease in the context of primary health care in Portugal.
Case description
A 21-month-old male, living with his parents in a town with optimal sanitary conditions, belongs to a nuclear family in Duvall’s family life cycle stage II and class II in Graffar’s socioeconomic status scale. The child was previously healthy, with a regular length and weight and adequate psychomotor development. He had an updated vaccination schedule, and no allergies were known.
The child was brought to the primary-health-care unit, complaining of fingernail alterations, with no other noticed signs or symptoms. The mother reported the child had developed a ‘white line that crossed the left index fingernail’ eight days before the appointment that began to shed six days later. The parents associated these findings as a result of an unnoticed trauma. As another ‘white line appeared on the middle-left fingernail’, the mother decided to seek medical observation and counselling. Perceived trauma, pain, pruritus, oedema, signs or symptoms of systemic illness, recent medications, or dietary restrictions were denied. Contact with animals and similar manifestations in the household or the nursery was also denied. While exploring previous infections and verifying the information available regarding recent appointments, it was found that the child had a history of HFMD (light form, three to four lesions in the anterior portion of the tongue and rare vesicles on the hands, feet, and perianal areas) four weeks before.
Clinical examination was unremarkable, apart from the alterations observed on the second and third left fingernails (Figure 1).
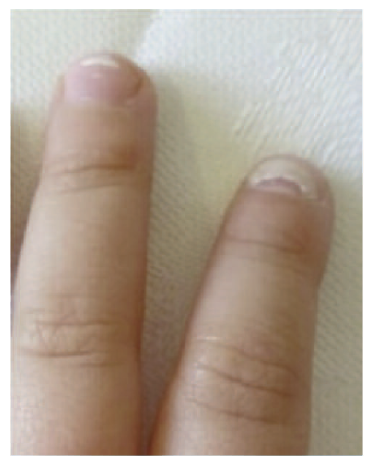
Figure 1 A transverse white ridge, called Beau’s line, is present distally on the third fingernail, and proximal shedding, called onychomadesis, is evident on the second fingernail.
In cases of children with onychomadesis, a history of viral infections should be sought in the months before its onset, being HFMD the most frequently reported aetiology. According to this, onychomadesis associated with HFMD was diagnosed. Therefore, as no nutritional deficits were suspected, it was decided in conjunction with the mother, to adopt an expectant attitude instead of performing further investigations.
The benign nature of the process and expected evolution were explained and reassurance was given to the mother.
In a month, the affected nails had fully shed and were spontaneously replaced by healthy thinner nails.
Patient’s perspective (child’s mother)
The child’s mother reported relief and satisfaction with the reassurance given, as she was anxious that the nail alterations could be related to a serious irreversible condition. Moreover, it was added that understanding parents’ concerns, providing medical information explaining it simply, and meeting their expectations, was extremely important.
Comment
Hand-foot-and-mouth disease is a contagious disease that can be caused by different non-polio Enterovirus infections (Enterovirus 71 and Coxsackie virus A16 mostly involved, whereas Coxsackie A6 has been implicated in sporadic HFMD cases and outbreaks and associated with onychomadesis), which commonly affects young children (average: five to seven years of age). 4-5 The virus spreading occurs by oral ingestion of the shed virus from the gastrointestinal tract, through airborne particles (coughing and sneezing), or via vesicle fluids or oral secretions of infected hosts. 5-6 Symptoms include low-grade fever, anorexia, general malaise associated with maculopapular rash (typically non-painful, non-pruritic) or vesicles on hands and feet (including palms and soles), buttocks, legs, arms, perioral and perianal areas, and painful ulcerative lesions over mouth, tongue, and throat. Rarely it can cause neurologic involvement, such as polio-like syndrome, aseptic meningitis, encephalitis, encephalomyelitis, acute cerebellar ataxia, acute transverse myelitis, Guillain-Barré syndrome, opsomyoclonus syndrome or benign intracranial hypertension. 2,5-7 However, some infections are asymptomatic. 7
Although HFMD is a highly contagious infection, it is usually limited, lasting seven to ten days. 6-7
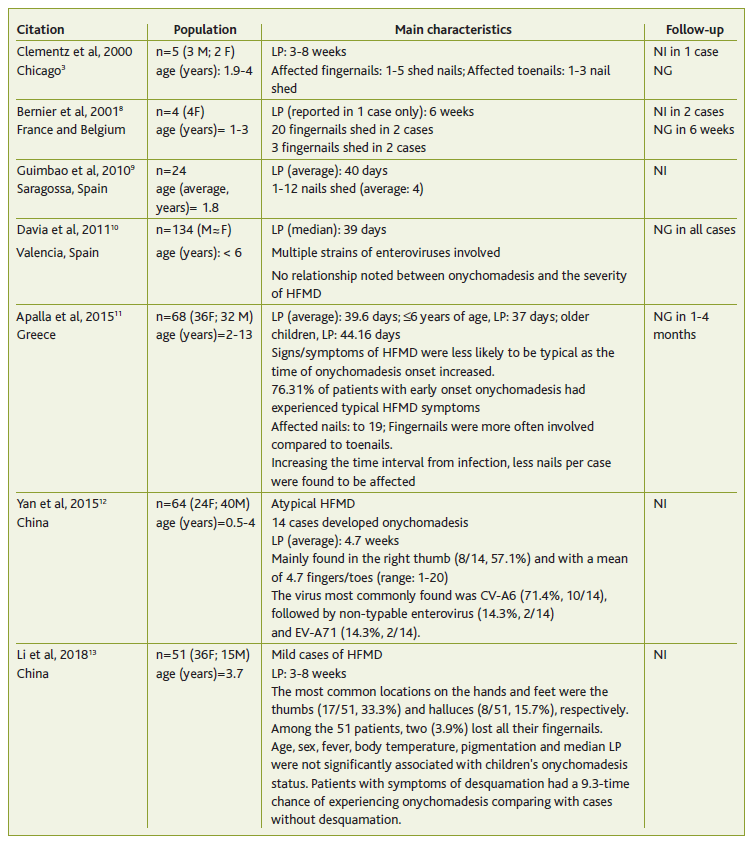
A late complication of HFMD involves nails. Since the first published cases mentioned the association between HFMD and onychomadesis, other reports can be found in the literature, some of these in the context of HFMD-enteroviruses causing outbreaks (Table 1). 3,8-13
Table 1 Summary of the main characteristics found in studies reporting on onychomadesis associated with HFMD
On average, up to 40 days after the onset of HFMD’s usual manifestations, nail alterations can develop. 7,9,11 Beau’s lines (nail plate white transverse ridging) and onychomadesis are the associated conditions. 3,14
The exact mechanism of onychomadesis is not well established, but it is probably related to a post-inflammatory periungual localized reaction or a direct viral infection of the nail’s matrix. 5,14 HFMD-causing viruses were detected in shed nail fragments of patients affected by onychomadesis following the infection. It was therefore suggested that virus replication damaged the nail matrix resulting in nail dystrophy. 7,15 Transient nail matrix arrest was the main reason for this phenomenon. 7 After the inhibition process which usually takes at least one to two weeks, 2 a new nail forms after the resumption of the nail’s matrix function and starts to grow proximally, extending under and pushing the previous nail outward. The cycle may take one to three months, is typically painless, and leaves no scars. 14 A new healthy nail forms, 14 as the nail’s basement remains intact. 10 Beau’s lines may appear in less severe cases of nail matrix arrest. 10
To diagnose HFMD-related onychomadesis, there are some conditions to consider. It was suggested that enteroviral co-infections or infections with more virulent strains might predispose to this phenomenon. Additionally, in the event of a period with a higher prevalence of this manifestation and/or if nail complaints occur three to twelve weeks (on average approximately six weeks) after HFMD infection, the index of suspicion should be raised. 14
In this case report, onychomadesis was a consequence of an indolent infection with no major associated symptoms. A case-series study observed no relationship between onychomadesis and the severity of the preceding HFMD, 10 which is consistent with the case.
The authors reinforce the existing evidence regarding the temporal association between HFMD and onychomadesis. This relationship may suggest that enteroviruses lead to a cascade of molecular alterations, interfering with the nail’s physiologic function.
This clinical scenario should therefore be considered in the differential diagnosis of onychomadesis aetiologies, enabling professionals to provide the correct management. Of great relevance for clinicians is the need to carefully assess and collect a detailed clinical history of viral infections such as HFMD weeks before onychomadesis presentation.
Advising and reassuring patients, parents, or caregivers about possible nail changes weeks after HFMD presentation, which will spontaneously heal with a new nail (at times more fragile), will avoid unnecessary concerns, investigations, referrals, and treatments.
Authors contribution
Conceptualization, JRS, and PV; writing - original draft preparation, JRS; writing - review and editing, JRS and PV. All authors have read and agreed to the published version of the manuscript.















