A 53-year-old patient submitted to a renopancreatic transplant 5 years ago presented progressive asymptomatic renal transplant dysfunction (Creatinine 1.9 → 2.6mg/dL) and increased arterial resistive index (0,88). A transplantbiopsy was performed revealing cellular rejection type IIA and thymoglobulin was initiated. After biopsy the patient presented macroscopic hematuria and Color-Doppler ultrasound revealed an arteriovenous fistula (AVF) in the kidney transplant parenchyma.
Embolization was postponed due to fever and E. Faecalis isolation on hemocultures, treated with ampicillin, with clinical and laboratorial improvement. A new biopsy was performed and showed no signs of cellular rejection. Serum antibodies were also negative for alloimmunization(Figs. 1, 2).
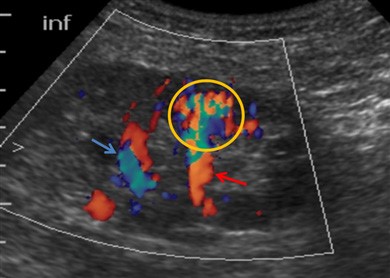
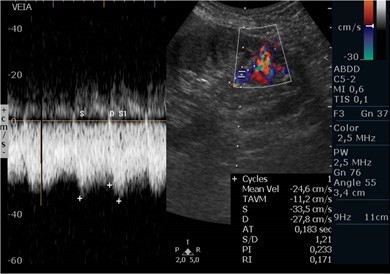
Figure 1: Color Doppler ultrasou- nd depicting an AVF (yellow circle) with aliasing due to turbulent flow and its arterial and venous vessels (red and blue arrows, respectively).
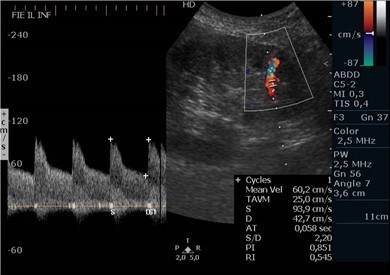
Figure 2: Color and Spectral Doppler from the artery feeding the fistula showing high peak systolic velocity (94cm/s) and a low¬-resistance pattern with increased diastolic velocity (42cm/s).
The patient remained clinically stable after 1 year of biopsy and showed progressive improvement of renal function, despite persistence of a high-debit fistula, therefore embolization was not performed and the patient remains in follow up.
Core needle biopsy remains an important tool in evaluation of renal transplant dysfunction.1 AVF is a common complication following biopsy or percutaneous vascular procedures.1,2 AVF can be asymptomatic or manifest as hematuria, renal failure or hypertension.3 On Color -Doppler, AVF appears as a focal high-velocity flow showing aliasing, that communicates with a feeding artery, with accentuated diastolic flow and a draining vein, with an arterialized venous waveform.2,3 Most small AVFs resolve spontaneously and only larger and symptomatic AVFs may need transcatheter embolization(Fig. 3).1,3