Introduction
Choledochal cysts are rare disorder of the biliary tree, with an incidence of 1 in 100 000 - 150 000 people in the western population and a higher prevalence in women (4:1 or 3:1). There is a strong predominance in Asian populations with a reported incidence of 1 in 1000, for reasons still unclear. The exact origin of choledochal cysts remains ambiguous and several theories have been proposed, ranging from a pure congenital abnormality to a sequelae of a multiorgan disease process. Choledochal cysts predispose to complications, such as cholestasis, choledocholithiasis, pancreatitis and malignant transformation, the latter occurring especially when associated with chronic inflammation. Although this biliary tree malformation may be easily recognised with currently available imaging techniques, classification is necessary for the purposes of risk stratification, proper treatment and management.1,2
Choledochal cysts were originally described in 1723 and since then have been recategorized several times. Currently, the classification proposed by Todani is the most widely accepted, based on location and morphologic characteristics and includes five main subtypes.1,3 Type-I cysts, which account for 50 - 80% of all choledochal cysts, represent a spherical or fusiform enlargement of the entire extrahepatic biliary tract; type-II cysts have a prevalence of 2% and are defined as an extra-hepatic biliary diverticulum; type-III cysts have a prevalence of 1.4 - 4.5% and manifest as a cystic dilation of the intramural duodenal segment of common bile duct, leading to a protruding mass into the duodenum lumen; type-IV cysts have a prevalence of 15% - 35% and are characterized by multiple extra-hepatic biliary cysts, either associated with intra-hepatic biliary cysts (type IVA) or isolated (type IVB); type-V cysts, also known as Caroli disease, have a prevalence of 20% and manifest with multifocal cystic dilation of intra-hepatic bile ducts. When accompanied with congenital hepatic fibrosis, type V cysts are defined as Caroli Syndrome.1,3
Case Report
A 58-years-old female, with no relevant personal history, presented to the emergency department with fever and abdominal pain. Physical examination revealed abdominal palpation tenderness, especially on the right hypochondriac region, without peritoneal reaction. Laboratory workup demonstrated leukocytosis (14.49 x 109/L), neutrophilia (84%), elevated C-reactive protein (177 mg/L) and also increase in total and direct bilirubin (3.48 mg/dL and
2.68 mg/dL, respectively), aspartate transaminase (250 U/L), alanine transaminase (550 U/L), gamma-glutamyl- transferase (573 U/L) and alkaline phosphatase (237 U/L). Abdominal ultrasound (US) (Fig. 1) was performed and demonstrated diffuse dilation of intra and extra-hepatic bile ducts without evidence of an obstructive etiology. An enlarged gallbladder, with lithiasis and sludge, was also perceived, without evidence of wall thickening.
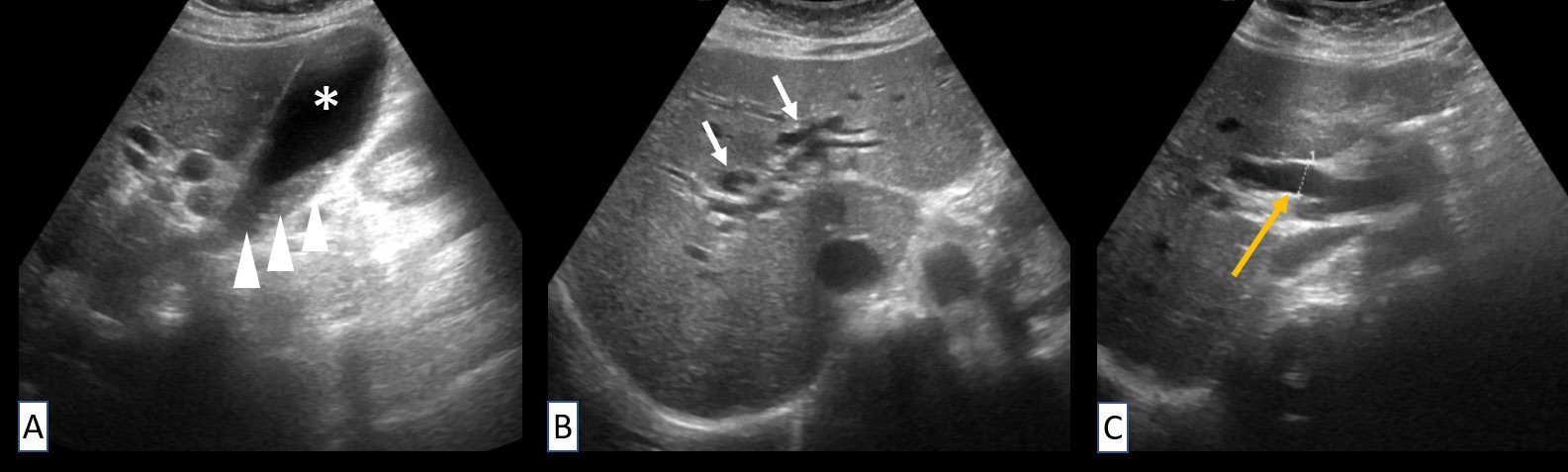
Figure 1: Abdominal US (A-C) demonstrates gallbladder enlargement (asterisk) with luminal sludge (arrowheads). A dilation of intra- hepatic bile ducts (white arrows) and of common bile duct (yellow arrow) is also depicted. No obstructive etiology is detected in this imaging modality.
For further characterization, the patient underwent a contrast-enhanced abdominal computed tomography (CT) (Fig. 2), which confirmed the US findings of diffuse common bile duct dilation and enlarged gallbladder. Additionally, it showed a cystic dilation of the intramural duodenal segment of the common bile duct protruding into the duodenum lumen. There was no evidence of a soft tissue mass adjacent to the common bile duct cystic segment. Mild ectasia of the distal pancreatic main duct was also detected, probably due to extrinsic mass effect of the cystic formation. Taking into account these imaging and clinical findings, a Todani type-III cyst with underlying cholangitis was suspected.
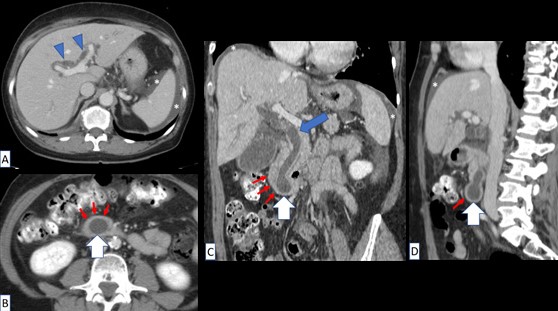
Figure 2: Contrast-enhanced abdominal CT scan (A-D) shows dilation of intra- hepatic bile ducts (arrowheads) and common bile duct (blue arrow). It is noticed a cystic dilation of the intramural duodenal segment of common bile duct (white arrows), with a protruding mass into duodenum lumen (thin red arrows), compatible with Todani type-III choledochal cyst. Small amount of free peritoneal fluid (asterisks) is noticed.
Patient was admitted to the surgery ward and, five days later, endoscopic retrograde cholangiopancreatography (ERCP) was done, confirming Todani type-III choledochal cyst. Sphincterotomy was also performed with drainage of microlithiasis, abundant bile and small amount of pus. In the meantime, the patient completed twelve days of antibiotic therapy with Piperacillin/Tazobactam regimen, with a favourable clinical and laboratory outcome.
Discussion
Todani type-III cyst, also known as choledochocele, is a dilated segment of the common bile duct that protrudes into the duodenal wall. Its pathogenesis remains poorly understood, being the most accepted explanation scarring or inflammation after stone passage. It is very rare, with an incidence less than 1/1 000 000, accounting for 1.4 - 4.5% of choledochal cysts.1
Choledochal cysts can become symptomatic from birth to old age, but are much more frequent in childhood ages, particularly before 10 years-old. The classic symptomatic triad consisting of fever, jaundice and abdominal mass occurs in less than 20% of patients. Symptoms are usually due to associated complications of ascending cholangitis and pancreatitis. Complications result from bile stasis, stone formation, recurrent superinfection and inflammation. Patients with Todani type-III cyst are often asymptomatic,
however, they can suffer from gastric outlet obstruction, either by directly obstructing the duodenal lumen or by intussusception.1,4
The first imaging modality indicated for assessment of the biliary tree is US, including in cases of suspected choledochal cysts, with a sensitivity of 71% - 97%, however the sensitivity is lower in type-III, because cysts are usually too small to visualize and the normal diameter of the common bile duct makes the connection with the biliary tree hard to identify. CT is useful in showing continuity of the cyst with the biliary tree, which was demonstrated in our clinical case. CT is also a good modality for evaluating its relation with surrounding structures and exclude malignancy.4,5 Given the concerns regarding ERCP, which increases the risk of cholangitis and pancreatitis, magnetic resonance cholangiopancreatography (MRCP) is now considered the gold standard to study choledochal cysts, with a reported sensitivity to be high as 90%-100%. However, ERCP allows therapeutic procedures, which was of paramount importance in the management of the patient in our case report. ERCP is also useful for delineation of biliary anatomy and to identify an abnormal pancreaticobiliary duct junction or ductal filling defects, advantages also provided by MRCP, especially with pre- imaging secretin administration, which increases pancreatic secretion and, consequently, duct dilation. In patients with type-III cysts, ERCP reveals smooth bulging of the papilla and cannulation will opacify the dilated intramural common bile duct.4,5,6 Due to their intramural location, type-III cysts tend to manifest with very subtle imaging features and the correct diagnosis preoperatively is made in approximately 30% of the time, with the diagnosis mostly achieved after multiple imaging modalities.4
Differential diagnosis for type-III choledochal cysts includes submucosal duodenal lesions, duodenal diverticulum and duplication cysts. A duodenal diverticulum fails to opacify with ERCP. Duplication cysts may have identical findings to choledochoceles and are consequently difficult to differentiate. Some authors point out that duplication cysts have muscular wall, which is absent in choledochoceles.1,4,7 The risk of malignancy associated with type-III choledochal cysts is very low, approximately 1.6%, therefore excision is not necessary. They often require endoscopic sphincterotomy to allow duodenal drainage of bile and stones, which is suggested by some authors to be performed even in asymptomatic patients. In cases of large choledochoceles with biliary, duodenal or gastric outlet obstruction, duodenotomy and cyst excision is recommended.8
We demonstrate a rare case of complicated of Todani type-III choledochal cyst, in which the correct diagnosis was suggested by imaging findings, further confirmed and managed with ERCP and antibiotic regimen. This condition belongs to the choledochal cyst spectrum of biliary tree malformations and radiologists must be aware about the Todani classification in order to adequately categorize the subtype. Identification of choledochal cyst subtype is crucial for risk stratification and appropriate management.















