Introduction
In developed countries, ENT (ear, nose, and throat) infections are extremely common conditions, typically following a benign course1, due to the impact of antibiotics on their morbidity and mortality.2,3
However, in the last years, there has been an increase in the reported cases of ENT infections that resulted in septic thrombophlebitis of the internal jugular vein followed by systemic embolism in young and previously healthy patients,4,5 a potentially life-threatening condition known as Lemierre Syndrome.4,6,7
Case Report
We present a case of a 24-year-old female patient, with previous adenoidectomy and no other significant past medical history, who presented to the emergency department (ED) after syncope with spontaneous resolution. The patient complained of odynophagia and fever with associated myalgias and headaches over the course of the past three days, which drove her to a primary care facility two days before. There, she was diagnosed with acute tonsillopharyngitis and treated with intramuscular penicillin and anti-inflammatory drugs (ibuprofen), without clinical improvement. At admission to the hospital, she presented leucocytosis (11,86 x 109/L), thrombocytopenia (15 x 109/L), increased C-reactive protein (CRP) (280,4mg/L) and acute kidney injury (serum creatinine of 2,3mg/dL), consistent with sepsis with multiorgan dysfunction.
In the first 24 hours of admission, she underwent clinical deterioration, with severe respiratory insufficiency. Computed Tomography (CT) scan of neck, chest and abdomen (Fig. 1) was performed and showed left thrombophlebitis of the internal jugular vein, associated with an enlarged left tonsil with fluid content and gas bubbles in keeping with an abscess in the left tonsil caused by a gas-producing organism; moreover, there were multiple nodules throughout the lung parenchyma suggestive of septic embolism, that coexisted with wedge- shaped consolidations, suspicious of septic infarcts, and basal consolidations. The first diagnostic hypothesis was Lemierre Syndrome with septic embolization to the lungs. Blood cultures were positive to group C β-hemolytic streptococci (GCBHS), and susceptibility-guided antibiotherapy was initiated (three days of intravenous ceftriaxone and two days of azithromycin, followed by piperacillin-tazobactam).
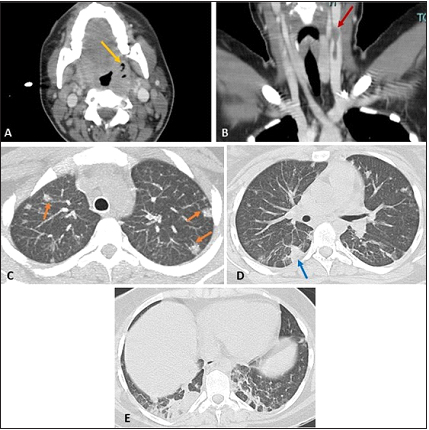
Figure 1: Contrast-enhanced cervicothoracic CT scan, soft tissue window (axial plane - A, coronal reformatted plane - B) and lung window (maximum intensity projection in the axial plane at the level of the aortic arch - C, axial plane at the level of the pulmonary trunk - D, and at the lung bases - E) reveals an enlarged left tonsil with fluid content and gas bubbles, in keeping with tonsillitis complicated with an abscess (yellow arrow - A) associated with a thrombus in the left internal jugular vein (red arrow - B). Chest CT shows scattered lung nodules affecting all pulmonary lobes, mostly in a peripheral location, and some of them with a clearly identifiable feeding vessel (orange arrows - C), suggestive of septic emboli. Wedge-shaped peripheral opacities (blue arrow - D), suspicious of septic infarcts, and basal consolidations are also seen (E).
The clinical status continued to worsen and the patient was intubated and admitted to the intensive care unit (ICU).
A control CT scan after 5 days of admission was obtained (Fig. 2), showing cavitation of the lung nodules, corroborating the previous diagnosis, and additional bilateral pleural effusion and central alveolar consolidations presenting with an anteroposterior density gradient, in line with acute respiratory distress syndrome (ARDS).
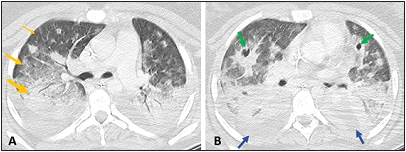
Figure 2: Contrast-enhanced chest CT scan, lung window (axial plane at two different levels - A and B) shows increase in size and cavitation of the previously identified lung nodules (green arrows - B), confirming the hypothesis of pulmonary septic emboli. In contrast to the previous CT scan, bilateral pleural effusion is now seen (blue arrows) and a radiological pattern of acute respiratory distress syndrome (ARDS), with an anteroposterior density gradient, resulting from dense consolidation in the most dependant regions (thick yellow arrow), followed by ground-glass attenuation (medium yellow arrow) and normal lung in the non-dependant regions (thin yellow arrow), in line with the progressive respiratory insufficiency.
During the ICU admission, the patient maintained severe systemic inflammatory response syndrome (SIRS) with fever, high CRP (370 mg/L) and leucocytosis (23 x 109/L), and developed progressive haematologic dysfunction (5 x 109/l platelets) and “de novo” liver dysfunction, presenting with mild cytocholestasis and hepatomegaly. There was also renal and cardiovascular dysfunction requiring vasopressor support.
Due to the need of prolonged and aggressive mechanical ventilation, the patient was placed on extracorporeal membrane oxygenation (ECMO) support, where she remained for 42 days. During this time, the most relevant complication was haemoptysis, requiring right bronchial artery embolization.
After ECMO suspension, the patient was intubated for another 15 days, and a tracheostomy was performed. Following another 64 days of mechanical ventilation, decannulation was tried and succeeded. Doppler evaluation showed no signs of jugular vein thrombosis.
At the 80th day of admission, the patient presented with recurrent tonsillitis and was treated with another course of antibiotics (10 days of intravenous ceftriaxone and clindamycin).
After 86 days of hospitalization, the patient was discharged and follow up was made by Otorhinolaryngology. In the months that followed, the patient had four more episodes of tonsillitis and a tonsillectomy was performed without complications.
Discussion
Lemierre syndrome was extensively described for the first time in 19363,8 and is characterized by septic thrombophlebitis of the internal jugular vein and bacteremia that can result in septic emboli, most often to the lungs.3,9 If pulmonary involvement is present, patients can develop respiratory failure, usually due to ARDS.3,6 Given this, up to 37% of the overall cases of Lemierre syndrome require intubation.6 This clinical picture is seen in association with an ENT infection, arising more frequently in the oropharynx, and affects primarily younger patients that were previously healthy, mostly in the 2nd and 3rd decades of life.3,6,7,10 Its incidence significantly decreased in the postantibiotic era and it is a rare disease nowadays; however, it can be fatal with mortality rates reaching up to 6-15%,4,11 reason why it should be promptly identified and treated.4,10
This infection is most commonly caused by anaerobic bacteria, usually Fusobacterium necrophorum, although polymicrobial bacteremia is reported to happen in up to one third of the cases, with anaerobic streptococci being frequently present,10,12 as in our case.
The first symptoms are usually related to an oropharynx infection and include sore throat, fever, weakness, and malaise.3,11 The presence of neck pain, pleuritic chest pain and/or respiratory distress in a previously healthy young adult with recent history of pharyngitis or tonsillitis should raise the suspicion of Lemierre syndrome, although its initial indolent course, unspecific clinical presentation and rarity often lead to a delayed diagnosis.11
Radiologists have an important role in the diagnostic process, as CT is usually included in the initial workup of a patient whose clinical condition deteriorates, enabling the identification of most of the findings that define this rare condition.3
Given the life-threatening potential of Lemierre syndrome and its typical imagiological findings, this condition should be known and promptly recognized by clinicians and radiologists.3,4,10















