Case Presentation
46-year-old female, referred to our hospital due to a 20-year history of right neck swelling. On physical examination, a pulsating firm painless mass was found on the right side of her neck, near the angle of the mandible. There was no pressure symptom and it was more mobile horizontally than vertically (Fontaine sign). Pulsations were felt on deep palpation and a faint bruit was heard on auscultation.
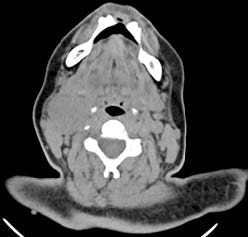
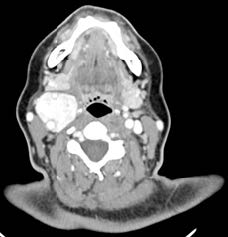
Cervical CT was performed. Non-contrast CT showed a well-circumscribed soft tissue mass (Figure 1). Contrast- enhanced CT showed a heterogeneous, markedly-enhancing mass, measuring 45 x 34 x 32 mm (Figures 2 and 3). It was located at the right carotid artery bifurcation, causing splaying of the internal and external carotid arteries (lyre sign). A diagnosis of a carotid body paraganglioma was reached. Based on imaging findings, it was classified as a Shamblin type II (Figure 2).
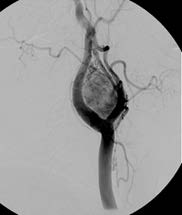
Digital subtraction angiography (DSA) was performed to assess the vessels supplying the mass and to perform preoperative embolization. Carotid angiogram demonstrated a hypervascular mass splaying the internal and external carotid arteries supplied by neovascularization from the external carotid artery (Figure 4). After catheterization with a microcatheter, tumor embolization was performed with 300 μm polyvinyl alcohol (PVA) particles. At the end of the procedure, an almost complete absence of tumor enhancement/vascularization was achieved.
The patient then underwent surgical resection, and the histological analysis of the surgical specimen confirmed the diagnosis of carotid body paraganglioma.
Discussion
Carotid body paragangliomas (CBPs), also known as a chemodectomas, are rare tumorsthat arise from paraganglion cells of the carotid body. Like other paragangliomas of the head and neck, CBPs have a female predilection, and are typically diagnosed in the 4th and 5th decades of life. They account for 60-70% of all paragangliomas of the head and neck. The rate of malignant degeneration of these tumors can be as high as 10%, with metastases most commonly appearing in bone, lung, liver, and lymph nodes.
CBPs can present in sporadic or familial forms (7-10%). They are painless, slow growing tumors that are often present many years before the patient seeks medical attention. On physical examination, they are mobile in the horizontal plane, but with a limited mobility in the vertical plane (Fontaine sign). Occasionally, a carotid pulse, bruit or thrill may be associated. Bilateral involvement is uncommon but occurs more frequently in familial cases. As they grow, CBPs characteristically splay apart the internal (ICA) and external (ECA) carotid arteries and envelop these vessels without narrowing them. After contrast administration, these tumors enhance avidly, in concordance with their vascular nature.
Ultrasound is often the first step in the diagnostic approach to CBP. On ultrasound, CBP typically appears as a solid, well-defined mass, with widening of the carotid bifurcation and splaying of the ICA and ECA. On color Doppler it appears as a hypervascular mass.
Historically, DSA was the “gold standard” diagnostic procedure for CBPs to confirm the diagnosis and provide accurate delineation of the vascular supply. The pathognomonic angiographic finding is widening of the carotid bifurcation by a well-defined tumour blush (lyre sign). However, with improvements in high-resolution imaging, cross-sectional methods are now the preferred modalities for surgical planning because they best define the relationship between the tumor and the carotid artery bifurcation, and the localization of the cranial nerves.
On CT imaging, CBP typically presents as an avidly enhancing soft-tissue mass at the carotid artery bifurcation that causes splaying of the ICA and ECA.
On MR imaging, flow voids from the numerous vessels are typically seen. This finding is part of the classic “salt and pepper” imaging appearance of these lesions seen on T1-weighted images. The “pepper” refers to the low signal flow voids, and the “salt” refers to high signal foci of hemorrhage and/or slow flow. Compared to the muscles, these lesions tend to be isointense to hypointense on T1-weighted images and hyperintense on T2-weighted images. After endovenous gadolinium, CBPs show marked enhancement.
The differential diagnosis includes glomus vagale tumor, vagal schwannoma, vagal neurofibroma, lymphadenopathy and carotid bulb ectasia.
Treatment depends on several factors, including the location and extent of the tumor, patient age and comorbidities.
Surgical excision is the treatment of choice and the only with curative potential. These tumors are very vascular, making resection challenging.
A surgical classification system was developed by Shamblin et al. in order to better predict surgical morbidity, which is related to the relationship of the tumor with the carotid vessels. Shamblin grade I is defined as a small tumor with minimal attachment to carotid vessels. Grade II is defined as a large tumor with some arterial attachment, but which does not entirely encase the carotid vessels. Grade III is defined as a large tumor that encases the carotid vessels.
Due to the highly vascular nature of paragangliomas, endovascular preoperative embolization is often performed. The procedure promotes tumour shrinkage, and reduces blood loss during surgery, operative time and morbidity.
In patients for whom the risk of complications precludes surgery, radiotherapy may be considered as an alternative treatment.