Breast lymphoma (BL) is an uncommon disease, with a prevalence inferior to 0,7%.1 Furthermore, since there are no specific clinical or imaging findings, BL may be difficult to diagnose both clinically and radiologically.2 To be able to consider the diagnosis, it is important to be familiar with the clinical and imaging findings that, although not specific for the disease, may arise suspicion. We present a clinical case of a primary breast lymphoma to review this rare pathology, exploiting the radio-pathologic correlations.
A 92-year-old female patient, without oncologic or hematologic known disease, presented to the breast unit with a large painful right breast mass, noticed for the first time 6 weeks before. The patient had no other complaints, including no other systemic symptoms. She was chronically medicated with antihypertensive, oral antidiabetics and oral anticoagulant drugs.
Clinical evaluation revealed a firm oval mass at the transition of outer quadrants (TOQ), measuring about 7cm. No other masses or nipple discharge were present, bilaterally. No axillary lymphadenopathies were palpable.
Mammographic evaluation revealed a global asymmetry of the right breast caused by a high-density oval lesion at the TOQ with obscured margins. There was concomitant diffuse skin thickening (Figure 1). No clusters of suspicious calcifications were present.
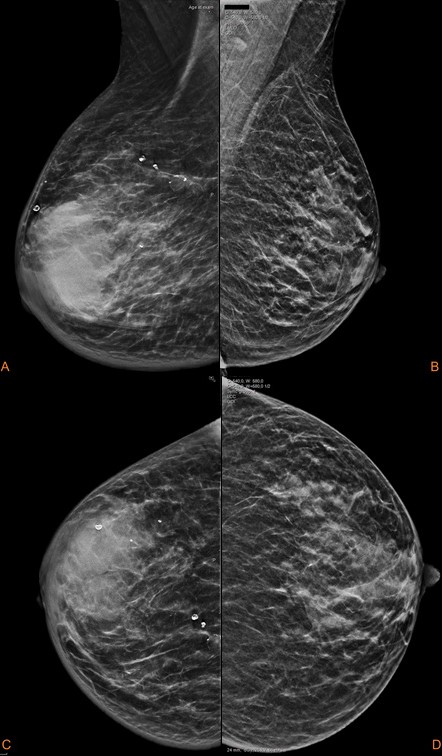
Figure 1: Mammographic evaluation with standard projections shows a global asymmetry caused by a high-density, non-calcified, oval lesion at the TOQ of the right breast, with indistinct and irregular margins. Diffuse skin thickening of the right breast is present.
Ultrasound revealed a single oval mass, with indistinct margins and very heterogenous echo pattern, with echogenic and anechogenic areas. The long axis of the mass was parallel to the skin line and it was highly vascularized (Figure 2). No axillary lymphadenopathies were seen.
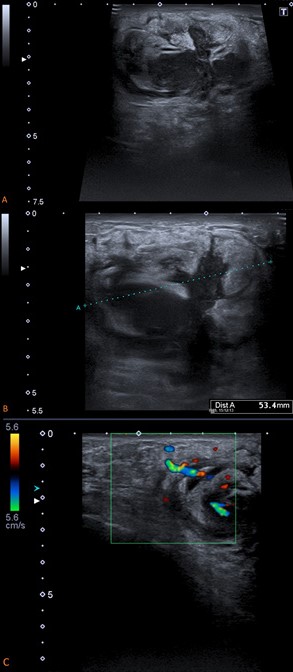
Figure 2: Breast ultrasound reveals (A) a large single oval mass, with indistinct margins and a heterogenous echo pattern, with echogenic and anecoghenic areas. (B) Because of its indistinct margins and large dimension, it was difficult to accurately measure the lesion at sonography, and it was underestimated. (C) The evaluation with colour Doppler shows prominent arteries and veins at the periphery of the lesion.
Giving these findings and considering the absence of other complains, we suspected of a primary breast malignancy. Our first diagnostic options were a poorly differentiated carcinoma, invasive lobular carcinoma or even a breast lymphoma.
To achieve diagnosis, we performed a 14G core needle biopsy of the lesion. The pathologic analysis revealed a large B-cell lymphoma.
Thoraco-abdominal-pelvic computed tomography (CT) was performed to evaluate systemic disease, revealing a large homogenous and well circumscribed lesion at the outer quadrants of the right breast (Figure 3). There weren´t any lymphadenopathies, neither organomegalies.
Patient was proposed to chemotherapy, with good response.
BL can be either primary or secondary, and like other lymphomas, has a bimodal age distribution with peaks in the middle of the 4th and 7th decades of life.2,3,4
According to Wiseman and Liao, the diagnose of primary breast lymphoma (PBL) requires an adequate biopsy demonstrating close anatomic proximity of breast parenchyma and lymphomatous infiltrate, absent history of previous extramammary lymphoma, and no evidence of concurrent widespread disease, except for simultaneously appearing ipsilateral axillary lymph nodes.5 Most PBL are intermediate or high-grade lymphomas, frequently B-cell lineage and, rarely, T-cell or histiocytic lineages.3,6Hodgkin's disease occurs very rarely as a primary tumour of the breast.7
Thus, secondary breast lymphoma (SBL) is diagnosed in the presence of widespread disease as a metastatic lesion, occurring frequently in patients with diffuse large B-cell lymphoma.1
There are no significant imaging differences between PBL and SBL, nor pathognomonic imaging findings. So, BL can be mammographic and sonographically indistinguishable from primary breast carcinoma (BC), fibroadenoma, phyllodes tumour or even metastatic disease.7 Diagnosis relies on adequate tissue biopsy for histopathological evaluation and immunophenotyping.8
PBL frequently presents as a large or rapidly enlarging solitary painless mass, especially in younger patients, clinically mimicking BC.2 On the other hand, multifocal, multicentric or bilateral lesions suggest SBL. Alternatively, BL may present as a painful mass or as breast skin thickening, especially those of high grade.2,3,5Most cases of PBL do not have prominent axillary lymphadenopathy, although this can be present.2 Systemic B-symptoms are infrequent in PBL, but common in SBL.1,3
Histologically features are relevant to understand the imaging findings. The pathological examination shows lymphoma cells infiltrating the breast lobules and ducts, which remain intact and do not show neoplastic changes.5 BL are highly cellular lesions, composed of non-cohesive round lymphoid cells of variable sizes, closely packed, with small extracellular spaces.9 No desmoplastic or fibrotic reaction is usually present.9,10Lymphangitic spread can occur, causing overlying skin changes.11
On mammograms, BL most commonly occurs as a solitary oval or round mass of homogeneous density, uncalcified (Figure 1). Since fibrotic or desmoplastic reaction are absent, BL does not cause stromal distortion of the surrounding breast parenchyma, contrary to BC. 2,3,7,10BL can also be mammographically occult or present as a diffuse increased parenchyma density.7,10Skin thickening can be appreciated on mammograms (Figure 1). This last pattern is predominantly observed with high-grade lymphoma.10 The findings of spiculate borders or calcification should propound another diagnose.7
Ultrasound features are nonspecific, so a wide spectrum of appearances have been described.2,3 Some authors have reported a common presentation as a solitary hypervascular mass (Figure 2), with irregular shape and indistinct margins, homogenous hypoechoic or a heterogeneous (Figure 2) echo pattern, without posterior acoustic phenomena.2,3
MRI features are also nonspecific, often like those of BC.1,5A round or oval mass, with areas of hypointensity or isointensity at T1-weighted imaging (WI), and areas of hyperintensity at T2-WI. The enhancement pattern may be homogeneous or heterogeneous, most commonly with a type II kinetic curve or, less frequently, a type III kinetic curve.1,5Skin thickening is more apparent than at mammography. The essential role of MRI is to evaluate the presence and extent of multicentric and multifocal lesions and stage the disease.1 It is also useful to evaluate treatment efficacy, and diagnose recurrent disease.1 Since these are highly cellular lesions, with small extracellular spaces, they often demonstrate higher restriction and lower ADC values then BC.9
CT is an important tool to stage, restage, and evaluate treatment response, being the modality of choice if Positron Emission Tomography (PET)-CT is not available (Figure 3). As others glucose-avid breast cancers, BL demonstrates high uptake at fluorodeoxyglucose (FDG) at PET-CT.

Figure 3: Computed tomography images demonstrate the mammary lesion as a large homogenous lesion at the outer quadrants of the right breast (circle).
Similarly, to other lymphomas, the treatment of BL is based on chemotherapy and radiation.12 Surgical treatment with lumpectomy is an option in some cases.















