Introduction
Congenital tracheal stenosis (CTS) is a rare condition, representing between 0.3 and 1% of all laryngotracheal stenosis.1,2It is a true embryological abnormality, and it is defined as an intrinsic narrowing of the tracheal lumen, most commonly due to complete or near-complete tracheal cartilage rings.2,3,4The absence of the normal membranous structure in the posterior strand makes the tracheal wall rigid and non-distensible, resulting in a fixed narrowed tracheal lumen.2,3,4,5
Diagnosis is almost always made during childhood due to respiratory obstruction, which can be life-threatening.4 It is usually made by contrast-enhanced computed tomography (CT) imaging or magnetic resonance imaging (MRI), and confirmed by bronchoscopy, which depicts complete cartilaginous tracheal rings.3 The typical imaging findings are circumferential narrowing of the trachea and fusion of the cartilaginous tracheal rings posteriorly, giving an appearance of an O-shaped trachea on axial images.1,3,4
The number of complete tracheal rings, their location, length, and severity of the luminal narrowing are variable.5 For this reason, the symptoms in CTS are also variable and are directly related to the degree of narrowing of the lumen and stenotic length.2
CTS is usually associated with other congenital anomalies, the majority being cardiovascular.2,3,4,5,6The most frequent is the presence of left pulmonary artery sling, which is found in 44% of cases,2 but other anomalies such as patent ductus arteriosus, ventricular septal defect, complex congenital heart diseases (such as Tetralogy of Fallot), and lung hypoplasia/agenesis are also frequent. Isolated CTS is present in 10%-30% of patients.5,6The associated malformations may mask the respiratory symptoms related to CTS, and they can also increase the severity of the symptoms.5
The prognosis of these patients has improved in the last years due to the development of new surgical and endoscopic techniques that allow an early and effective reconstruction of the stenotic trachea.1,6
We report a case of congenital tracheal stenosis diagnosed in a child with a history of corrected Tetralogy of Fallot presenting with severe respiratory distress.
Case Report
A 13-month-old boy with a previous history of colostomy and urethrostomy performed in his first 24 hours of life due to a recto-urethral fistula, and Tetralogy of Fallot repaired at 11 months old, both with an uneventful post-operatory recovery, was admitted to the emergency room due to acute respiratory distress. His mother reported noisy breathing since birth, wich was attributed to the cardiopathy. He had been hospitalized for 5 days one month earlier, with bronchiolitis caused by the respiratory syncytial virus.
On examination, he had biphasic stridor, tachypnea, chest retractions, and a SpO2 of 65% on room air. Due to acute hypercapnic respiratory failure, invasive mechanical ventilation in the Intensive Care Unit was required, with unexpected high pressures. Parainfluenza virus was identified on respiratory samples.
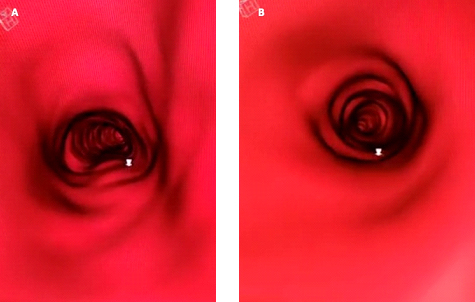
Videobronchoscopy revealed narrowing of the lower third of the trachea, with complete tracheal rings. A CT scan was performed to assess the airway, namely, to determine the extent and severity of the stenotic segment due to the tracheal rings. It showed normal morphology in the upper two-thirds of the trachea and a round O-shaped trachea in the lower third, with reduction in lumen caliber of approximately 50% (figure 1 and figure 2).
He was discharged after 11 days of hospitalization and referred for sliding tracheoplasty.
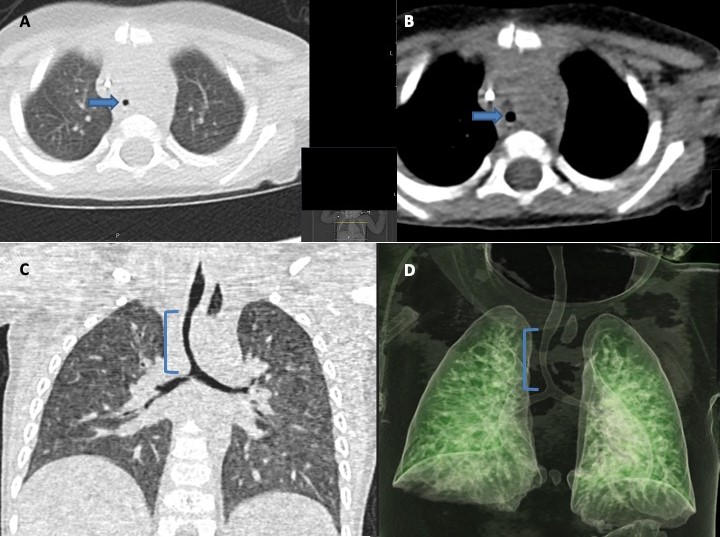
Figure 1: Computed tomography performed after extubation. Images in the axial plane at the level of the distal third of the trachea, in the pulmonary window (A) and in the mediastinal window (B) show the trachea with an O-shaped morphology and with reduced caliber (arrows), findings that suggest the presence of congenital tracheal rings and stenosis congenital tracheal. In the coronal plane (C) it is possible to determine the length of the stenotic segment ((), which extends to the bifurcation. 3D reconstruction of CT in the coronal plane (D) clearly shows the stenotic segment of the trachea, allowing to assess its length and characteristics.
Discussion
CTS is a rare and life-threatening condition with a mortality rate of 44%-79%.4,6The true incidence is unclear because many infants with CTS may die without a diagnosis, and mild stenosis may be asymptomatic and undiagnosed.6,7 Airway obstruction in patients with CTS can be exacerbated by infection and inflammation, as in our clinical case, or direct trauma after airway manipulation or surgery.7
The gold standard for diagnosis and assessment of length and diameter of CTS is rigid bronchoscopy under general anesthesia.1,2,6Flexible bronchoscopy is a useful alternative to visualize the narrow segment of the trachea.6 However, these procedures are invasive and have risks. Traumatic edema of the mucosa in the stenotic segment caused by the introduction of the bronchoscope can result in severe airway obstruction.3,6In addition, when CTS is diagnosed by bronchoscopy, CT or MRI are essential to study the associated malformations.1
CT and MRI are very useful in the diagnostic work-up of tracheobronchial anomalies, as they provide a good anatomic delineation of the airway, and enable a full assessment of the vascular structures and their relations to the adjacent trachea.1,2,6Thus, and with the increasing availability of these techniques, bronchoscopy may be avoided in some cases.1 An advantage of CT is the possibility to determine the extent of the stenotic segment, as this information is often difficult to obtain with bronchoscopy due to the inability and risks to bypass the stenosis.1,4The CT appearance of tracheal stenosis usually consists of a perfect circle with a smaller diameter than the immediate subglottic portion of the trachea (O-shaped trachea on an axial section).1,3
Both CT and MRI have advantages and disadvantages. The main disadvantages of CT are the potential risks of radiation exposure (especially in pediatric patients) and adverse reactions to contrast.3,8The major strengths of CT are being faster, requiring sedation less often than MRI and allowing to perform virtual tracheobronchoscopy studies.3,8
MRI provides excellent definition of anatomical structures, without ionizing radiation and without the need for contrast administration.8 However, its disadvantages include the long scan times, respiratory artefacts that degrade image quality, and the need for sedation, which has risks, mainly due to the reduced airway caliber in these patients.8
The radiologist should always perform a systematic review of the airway morphology and caliber, so tracheal anomalies don’t be overlooked, especially if reporting a complex case with other anomalies/malformations and regardless of whether there is clinical doubt about it.
There are morphological and functional classifications for CTS. Cantrell and Guild classified CTS by anatomical criteria into three types: generalized stenosis, funnel-like segmental stenosis, and segmental stenosis.3,5,7Segmental stenosis usually involves the lower trachea,3 as in our case. The functional classification is based on the symptoms: mild (asymptomatic or occasional symptoms), moderate (respiratory symptoms without respiratory embarrassment), and severe (severe symptoms including respiratory embarrassment).7 It is believed that pediatric patients can tolerate 50% tracheal narrowing before becoming symptomatic.7 Our patient was anatomically classified as having segmental stenosis and functionally as severe symptoms (acute hypercapnic respiratory failure, requiring invasive mechanical ventilation).
CTS management depends on the severity of the stenosis, the severity of symptoms, and the presence of other anomalies or airway pathology.2,7A multidisciplinary approach is usually necessary.7
The decision of when to perform the surgical or conservative treatment is controversial.2 Generally, in asymptomatic patients or with mild symptoms, conservative treatment is preferred, as the stenotic trachea may grow, and patients may become free of respiratory symptoms over time.6,7,8However, common viral upper airway infections can aggravate airway obstruction.6
Surgical intervention is the treatment of choice for children with severe symptoms such as respiratory failure, extubation failure, and acute life-threatening events.6,7,9The surgical approach differs according to the surgeon and the symptom severity and may include resection of the stenotic segment and primary anastomosis, patch tracheoplasty with nontracheal autologous tissue, and tracheal dilatation with or without stent insertion.1,6,7,9Most procedures have produced unfavorable results and are associated with high morbidity and mortality rates.9 Slide tracheoplasty has been a revolution in the management of CTS, achieving significantly better results.9
In conclusion, CTS is a rare and life-threatening condition, and early diagnosis and intervention increase the survival rate. CT and MRI play an important role in the diagnosis of CTS, as well as in determining the length of the stenosis and the caliber of the tracheal lumen, which are fundamental elements for the therapeutic decision. It is essential that the radiologist carefully assesses the morphology and caliber of the trachea in children and raises this diagnostic hypothesis.