Clinical Presentation
We present the case of a 64-year-old man with a past medical history of pancreatic neuroendocrine tumor which was being routinely followed up in our department. At the time of the first diagnosis, in 2010, he was submitted to a distal pancreatectomy and splenectomy. Later, in 2017, hepatic metastases were detected and successfully treated with chemotherapy. Besides, in 2020, he was also diagnosed with multiple myeloma (MM) and underwent a treatment with Lenalidomide, Bortezomib and Dexamethasone (VRd). However, the disease continued to progress until May 2021, when at the time a pancreatic focal lesion was detected in a routine abdominal and pelvic computed tomography (CT) and abdominal magnetic resonance imaging (MRI).
Imaging Findings
Abdominal MRI and abdominal CT revealed a well defined focal pancreatic lesion, in the cephalic region, measuring approximately 20 mm x 27 mm, showing important restricted diffusion (Figure 1). It was hypovascular both in the arterial and the late phases, with no associated changes in the bile and pancreatic ducts (Figure 1, 2). There was no evidence of liver metastases, although multiple vertebral lytic lesions in the context of MM were found (Figure 3). A positron emission tomography (PET) was performed revealing the lesion to be hypermetabolic (Figure 4). The endoscopic ultrasonography (EUS) showed a hypoechoic rounded mass and a sample was collected through a fine-needle biopsy. There were no adenopathies or vessel invasion. Tumor markers including CA125, CA19.9, CEA, and AFP were all within the normal limits.
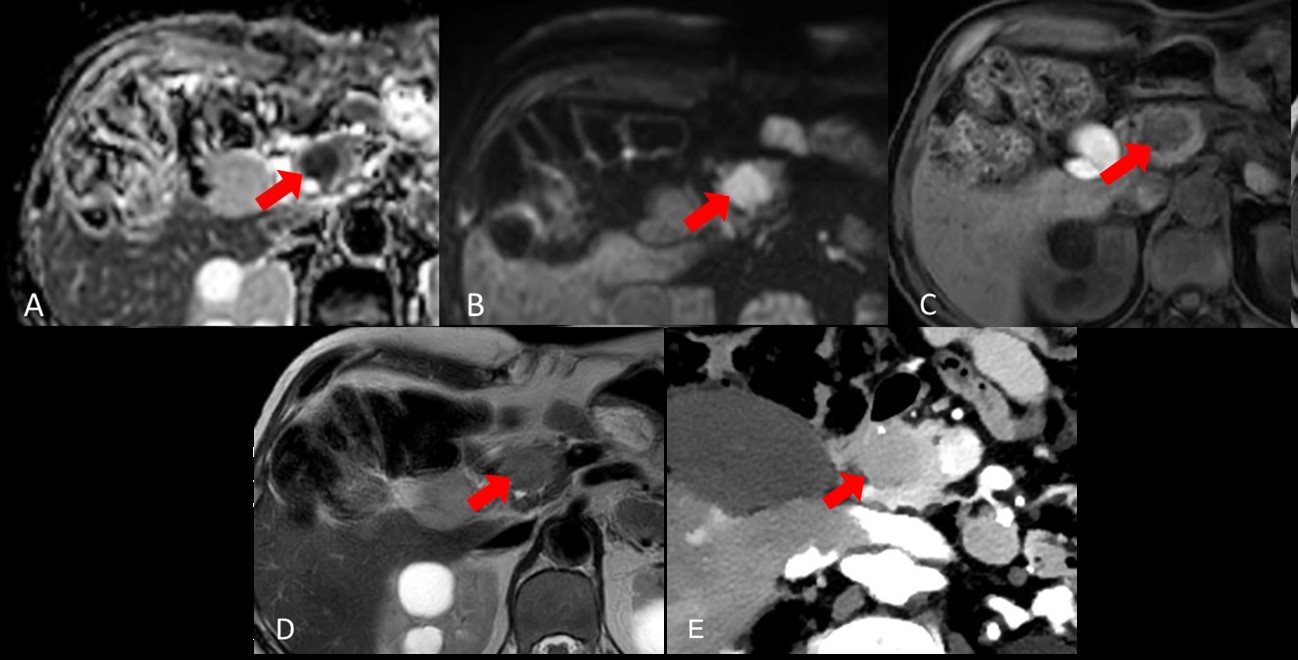
Figure 1: MRI images of the pancreatic focal lesion, showing hyposignal on ADC map (A), hypersignal on b900 (B) and T1WI (C) and slightly hypersignal on T2WI (D). Abdominal enhanced CT (E) showing hypovascular lesion on arterial phase.
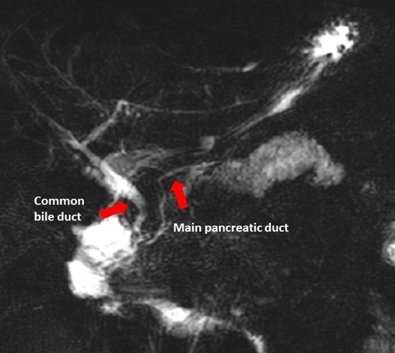
Figure 2: MR Cholangiopancreatography images showing the normal caliber of common bile duct and main pancreatic duct.

Figure 3: CT and MRI images showing multiple vertebral and iliac lytic lesions, in the context of MM.
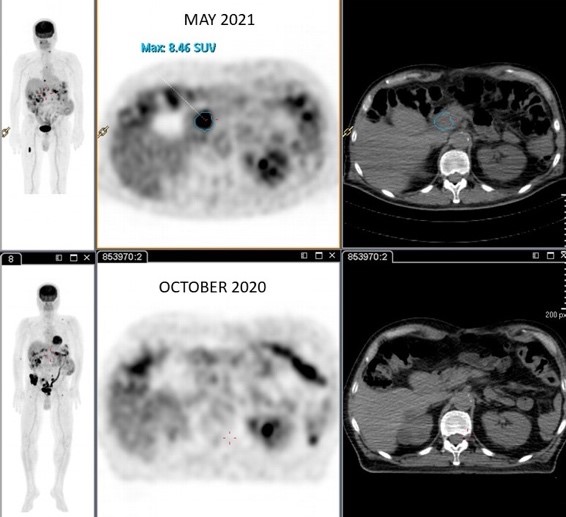
Figure 4: PET-CT image showing a hypermetabolic focal pancreatic lesion in May 2021, that was not present in October 2020.
The morphological pattern of the pancreatic lesion (normal main pancreatic duct) and the normal tumor markers helped to exclude a ductal adenocarcinoma. Considering the medical background of the patient, there were two possible diagnoses: recurrence of neuroendocrine tumor or intrapancreatic extramedullary plasmacytoma. The biopsy confirmed the second diagnostic hypothesis, and the tumor cells demonstrated positivity for plasma cell marker CD138 and kappa light chain, in keeping with the monoclonal nature of myeloma.
The patient completed five days of stereotactic body radiation therapy (SBRT) (median dose 30Gy) and received treatment with PACE (cisplatin, etoposide, doxorubicin and cyclophosphamide), which resulted in a partial response of the disease with complete metabolic response of pancreatic lesion on PET-CT.
Discussion
Extramedullary plasmacytomas are plasma cell tumours that present outside the bone marrow.1 Upper respiratory tract is the most common site for extramedullary involvement (80-90%). However, all the body sites can be affected, including gastrointestinal tract (about 10%), genitourinary tract, reticuloendothelial system, thyroid, lungs, skin and testicles.2,3Pancreatic involvement is rare, being found in approximately 2.3% of autopsies.4
Pancreatic plasmacytoma affects predominantly males and may co-occur with underlying MM, may precede the diagnosis of MM or may be a recurrence sign of MM.1 The most common form of involvement is focal, but diffuse infiltration may also be seen.1,2,3,6,7The head of the pancreas is the most common site to be involved, which explains why the most common clinical findings are obstructive jaundice and abdominal pain.1,2,3,5,6,7,8
Imaging modalities for detecting the disease usually include ultrasound, CT, MRI, EUS and EUS guided fine-needle aspiration (FNA), however, imaging findings are not specific and may resemble typical findings of other pancreatic neoplasms including adenocarcinoma, neuroendocrine tumors, lymphoma and metastases.
Pancreatic adenocarcinoma originates from the ductal epithelium, causing dilatation of the main pancreatic duct. The tumor most often occurs in the pancreatic head and represents the majority of pancreatic tumors. It is usually iso or hypodense on CT scan, and it is hypointense on T1 weighted images (T1WI) and slightly hyperintense on T2 weighted images (T2WI) on MRI scan,5 as in our case. Due to the hypovascularity, the tumor demonstrates only minimal enhancement compared with obvious enhancement of the normal pancreatic parenchyma. Atrophy of the distal pancreas, dilation of the main pancreatic duct and bile duct, invasion of the adjacent vessels, adenopathies, and liver metastases could also be detected in pancreatic adenocarcinoma. Our patient’s tumor was hypovascular but the main pancreatic duct was not dilated, making this diagnosis less probable.
Pancreatic neuroendocrine tumors (NET) are rare tumors that originate from pluripotent stem cells in the ductal epithelium of the pancreas.5,11The tumor is iso to hypodense on CT scan, relatively hypointense on T1WI and generally hyperintense on T2WI. Functional NETs are generally small and manifest as well-defined hypervascular lesions. Non-functioning tumors, on the other hand, are relatively larger in size, often well-defined and encapsulated, and show heterogeneous enhancement. Despite our patient's personal history of neuroendocrine tumor, the mass was hypovascular, making this diagnosis also less probable.
Primary pancreatic lymphoma is also rare and usually an extranodal manifestation of B cell non-Hodgkin’s lymphoma.5 Significant peripancreatic lymph node enlargement with disseminated lymphadenopathy can usually be found, but it was not the case. Pancreas is an unusual site for metastases, and they are typically seen with advanced disease.5,12
Lastly, pancreatic plasmacytoma should be considered in the differential diagnosis of a patient with multiple myeloma and a pancreatic mass, as in our case. For these reasons, biopsy is the standard of care in cases with suspected pancreatic plasmacytoma.
There is no standardized treatment for extramedullary plasmacytoma of the pancreas. The combination of local radiation, chemotherapy, and, in selected cases, surgery is necessary for diagnosis and treatment.2 In our case, the patient was treated with PACE and SBRT with complete metabolic response of pancreatic plasmacytoma on PET-CT and partial response of the disease.
Approximately 70% of patients have isolated pancreatic plasmacytoma and these cases remain disease-free for 10 years, with regional recurrence in as up to 25% of patients.13,14,15The course of the disease is more favorable in cases with primary plasmacytoma compared with those having plasmacytoma accompanying MM.5















