Case report
A 35-year-old man presented to the emergency department with a 12-hour history of pain that started in the epigastric area and then migrated to the right lower quadrant. He did not report vomiting, change in bowel habits or dysuria.
Physical examination showed axillary temperature, 38.10C; tenderness at palpation over McBurney´s point without rebound. The patient had been submitted to appendectomy 8 months earlier.
Blood tests showed leukocytosis (13.1 x 109/ L; N: 4-11) with 76% neutrophilia and a sightly C-reactive protein increase (5.4 mg/dL; N: <3). Urinalysis was normal.
Abdominal ultrasound showed a noncompressible hypoechogenic oval mass, with surrounding hyperechogenic fat and small amount of fluid in the right iliac fossa (figure 1).
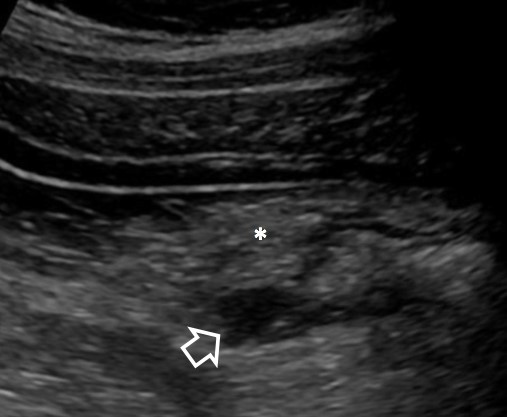
Figure 1: Abdominal ultrasound shows an oval hypoechoic formation arising from the base of the cecum (open arrow) and thickening of the surrounding mesenteric fat (*).
CT scan with intravenous contrast of the abdomen and pelvis was performed, demonstrating a tubular structure with enhancing wall extending from the base of the cecum and stranding of the adjacent fat (figure 2), findings suggestive of stump appendicitis.
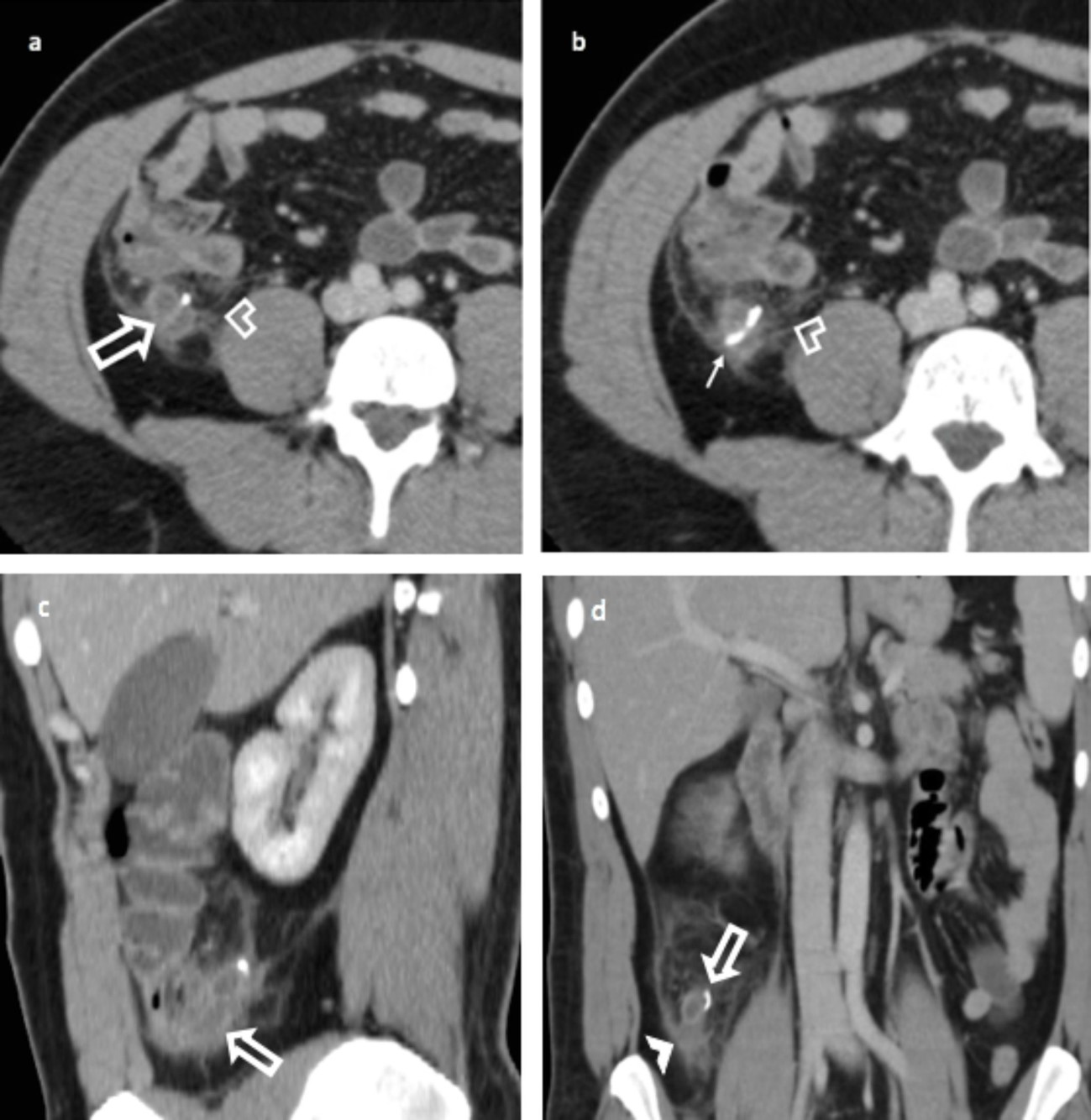
Figure 2: Axial contrast-enhanced CT scan series of abdomen (a, b) show enlarged appendiceal stump with enhancing wall (open arrow); thickening of the peritoneal reflection can also be seen (open arrowhead). Note staple line (b) from initial appendectomy (solid arrow). Sagittal (c) and coronal (d) reformatted images better depict the enlarged appendiceal stump arising from cecum (open arrowhead). There is stranding of adjacent mesenteric fat and local free fluid (solid arrowhead). Imaging also excludes free intraperitoneal air and abscess formation.
The patient underwent exploratory laparotomy and acute inflammation and obstruction of the stump appendix by an appendicolith was confirmed in pathology. There was no perforation or abscess formation.
The patient did well and was discharged home two days after surgery.
Discussion
Appendectomy is the most common surgery worldwide. Stump apendicitis is a rare surgical complication (1/50 000 cases) characterized by inflammation of the appendiceal remnant after incomplete appendectomy. It is reported to have increased since the introduction of laparoscopic appendectomy.1
The remnant appendiceal greater than 5 mm in length is a risk factor for the formation of fecaliths and consequently stump appendicitis.2 The experience of the surgeon, the subserous or retrocecal position of appendix and an inadequate dissection technique are other known risk factors for stump appendicitis.2,3
The time to develop this complication is long, ranging from 9 weeks to 50 years and the signs and symptoms are similar to the classical acute appendicitis, leading to a delay in diagnosis due to the previous history of appendectomy.2
Unrecognition of this entity causes a delay in the diagnosis, leading to severe complications, such as abscess formation, high rates of perforation (70%) and septic shock.4,5
Abdominal ultrasonography and CT are useful tools for attempted diagnosis. Ultrasonography can demonstrate the appendiceal remnant, as a tubular structure extending from the right iliac fossa or retrocecal region to the cecum, the hyperechogenic of periappendiceal fat and free fluid, but it is operator dependent and it is limited by the patient biotype as well.
Abdominal CT scan is more specific than US in depicting the typical findings, being the exam modality of choice to characterize the complications, such abscesses, perforation and peritonitis.
Prompt suspicion and confirmation of the diagnosis with CT is therefore essential to avoid serious complications, improving morbidity and mortality.4















