Introduction
Atraumatic splenic rupture (ASR) is an exceptionally rare pathological condition.1
There have been reports of splenic rupture without trauma in pathological situations like infection, being malaria the single major cause of ASR worldwide.2
Although cocaine-associated splenic pathology has been previously described in reports in the literature,3 ASR can be easily misdiagnosed given its singularity and distracting symptoms, which are typically cardiovascular presentations, such as ischemia or infarction, hypertension, and arrhythmias.4
This is the report of a 51-year-old man presenting to emergency with a cocaine induced American Association for Surgery of Trauma (AAST) grade V splenic rupture that required urgent laparotomy and total splenectomy.
Our report aims to raise awareness of potential splenic rupture in cases of abdominal pain without a history of trauma, but with history of cocaine use.
Case Report
A 51-year-old male with a past medical history of dilated cardiomyopathy, aside from often cocaine and cannabis use, presented to the emergency department with chief complaint of abdominal pain. The pain was constant, sharp, and nonradiating. The patient provided information of intranasal cocaine use at his birthday party on the day prior to his presentation to the hospital. His pain was associated with multiple episodes of vomiting and nausea. The patient denied any trauma, sick contacts, or recent travel.
At the initial evaluation, the patient was awake, alert and oriented to time, place and person (Glasgow Coma Scale of 15). The vital signs were as follows: blood pressure of 105/57 mmHg, heart rate of 80 beats per minute and a peripheral oxygen saturation of 97% on room air.
On physical examination, the patient was found to have signs of peritonitis.
Arterial blood gas (ABG) analysis revealed pH 7.406, partial pressure of carbon dioxide (pCO2) 44 mmHg, partial pressure of oxygen (pO2) 59.9 mmHg, oxygen saturation 97%, bicarbonate (HCO3) 26.4 mEq/L and lactates 0.8 mg/dL. Laboratory studies showed an initial hemoglobin of 12.9 g/dL and urine toxicology was positive for cocaine (500 ng/ml) and opioids.
A non-contrast computed tomography (CT) scan of the thorax, abdomen and pelvis was performed, followed by a subsequent intravenous administration of a radiocontrast agent containing iodine, with imaging acquired during the arterial, venous and delayed phases. In the axial unenhanced acquisition, a fluid with high density (up to 52 Hounsfield units) was observed in the perihepatic and perisplenic regions, revealing higher attenuation around the spleen (Figure 1A). These findings suggested the likely origin of the hemoperitoneum.
In the post-contrast arterial acquisition, the spleen had dimensions within the normal index range, exhibiting compression by the surrounding hemorrhage. Additionally, a distinct blush was identified, highlighting a focal region of active hemorrhage within the hematoma (Figure 1B). Contrast extravasation isoattenuating with enhanced blood vessels that persisted and progressively enlarged in the successive phases was noticed in the post-contrast portal venous and delayed acquisitions (Figure 1C, 1D).
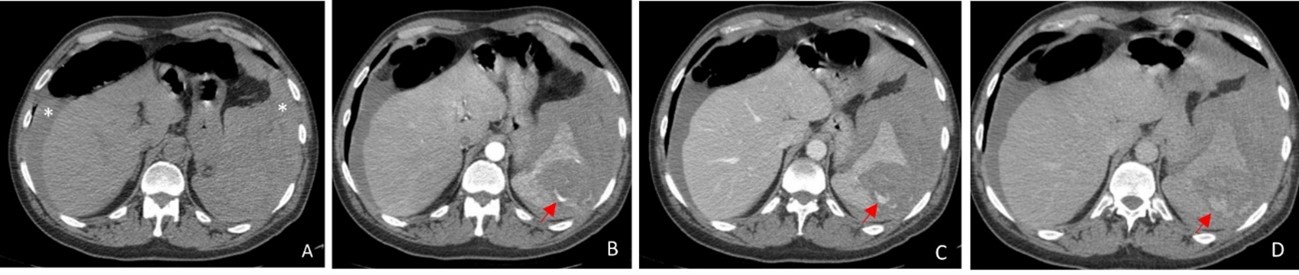
Figure 1: Axial unenhanced (A), arterial (B), portal venous (C) and delayed (D) post-contrast acquisitions showed: High density perihepatic and perisplenic fluid (*), with higher attenuation around the spleen, indicating a probable source of the hemoperitoneum; Normal-sized spleen, surrounded by fresh hyperattenuating (up to 52 Hounsfield units) hemorrhage. Contrast extravasation isoattenuating with enhanced blood vessels (arrows) that persisted and progressively enlarged from the arterial to the delayed acquisition, indicating active extravasation.
Coronal portal venous post-contrast acquisition showed a hemoperitoneum that surrounded a ruptured spleen (Grade V AAST) (Figure 2). There was no evidence of fractures involving the left ribs. Neither signs of pneumoperitoneum nor hollow viscus perforation were observed.

Figure 2: Coronal portal venous post-contrast acquisition showed a hemoperitoneum that surrounded a ruptured spleen.
After a brief explanation of the planned procedure, the patient gave consent and underwent an exploratory laparotomy. After accessing the abdominal cavity through a midline incision, a large amount of blood (~ 1.5L) was identified. After scooping out as much blood as possible, on inspection, we noticed the spleen was ruptured and blood was found oozing from the hilum. We proceeded with a splenectomy and the surgical specimen was sent for histopathological examination.
After an intraoperative peritoneal lavage with saline, the hemostasis was secured. A Blake 19 Fr drain was left in the left subphrenic space and the abdomen was closed.
At the end of the procedure, the patient had a hemoglobin of 8.8 g/dL, prompting the administration of 1 unit of packed red blood cells (PRBCs).
The patient was then taken to an intensive care unit where he would spend the post-operative day 1, being downgraded to a medical-surgical unit at the end of the day.
On post-operative day 2, a hospital-acquired pneumonia was diagnosed. Empiric antibiotic therapy was initiated and the patient completed a 7-day regime of piperacillin/tazobactam. During the remaining hospital stay, we were able to achieve progressive weaning of oxygen supplementation and resolution of respiratory failure, maintaining good oxygen saturation on room air without signs of breathing difficulty. On post-operative day 9, the patient was discharged home following post-splenectomy vaccines. We chose to vaccinate sooner than 14 days, as we believed the risk to miss vaccination was high after hospital discharge.
According to the histopathological examination of the surgical specimen, the spleen was 394-gram, 15 cm × 10 cm × 9 cm and showed rupture of the capsule on the upper surface lateral for an extension of 9 cm, with underlying hematoma of 4 cm of larger diameter. The remaining parenchyma had some small hematomas in the hilar region, the largest measuring 1.5 cm in diameter. Hemorrhagic necrosis lesions were observed at the periphery of the subcapsular hematoma (Figure 3A-C).
Consent for the publication of this case report was obtained from the patient.
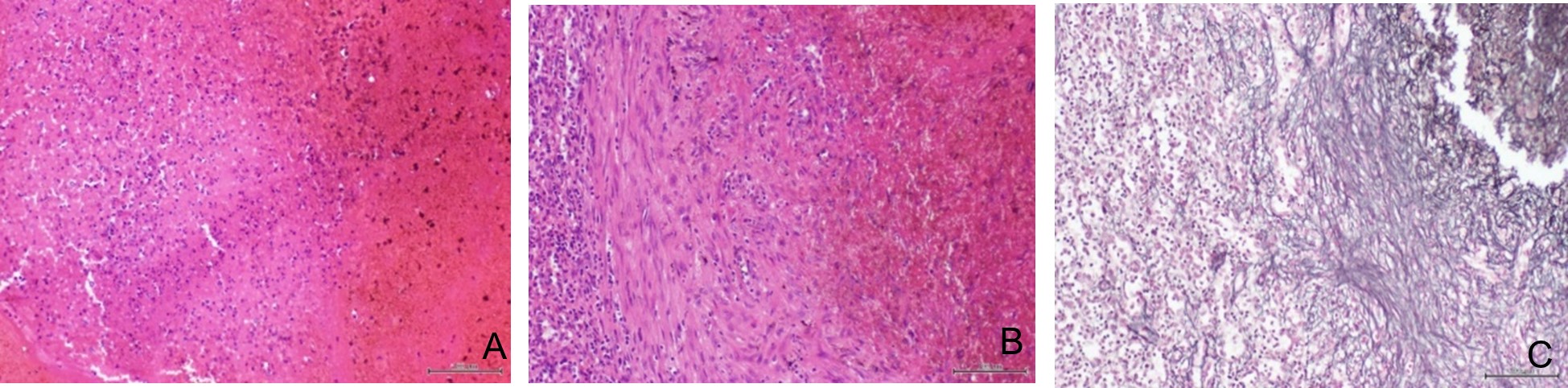
Figure 3: Optical microscopy imaging: (A) Spleen showing hemorrhagic necrosis lesions (hematoxylin and eosin, original magnification x100); (B) Fibrous reorganization with fibroblast deposition at the periphery of a perihilar hematoma (hematoxylin and eosin, original magnification x100); (C) Fibrous reorganization enhanced by thickening of the reticulin network (reticulin, original magnification x100).
Discussion
Splenic rupture most commonly results from a traumatic mechanism and leads to hemoperitoneum. The use of extended focused assessment with sonography in trauma (eFAST) examination on the trauma care primary survey can allow for an early detection and management of a hemoperitoneum. On the other hand, the absence of a traumatic incident may cause a delay in diagnosing and treating a splenic rupture, resulting in continuous blood loss and worsening of overall status.
Renzulli et al. proposed in 2009 the following division of the causes associated with atraumatic splenic rupture: neoplastic, inflammatory, infectious, mechanical, drug related and idiopathic.1 The described case is part of the drug related etiology that amounts to 9% of ASR.1
Given the scarcity of ASR events, there are no definitive guidelines regarding its management. The American Association for Surgery of Trauma (AAST) guidelines are often taken as a model for the therapeutic choices regarding the ASR. Treatment may include operative or non-operative therapy, depending upon the presence of hemodynamic instability, the amount of blood products used, the underlying pathology, the degree of hemoperitoneum and the extent of splenic injury.2
According to the World Society of Emergency Surgery (WSES) guidelines, non-operative management should be prioritized as the initial treatment approach, even in cases of splenic rupture classified as AAST grade V, provided that the patient is hemodynamically stable.5 Additionally, for AAST grades IV or V, angiography/angioembolization with coils is advisable, irrespective of the presence of a contrast blush on the CT scan.5 Regardless of the hemodynamic stability our patient presented at admission, since signs of peritonitis where identified, an operative management via a laparotomy approach became imperative.
Cocaine addiction remains a high-morbidity chronic-relapsing illness and it is associated with a wide range of medical complications explained by its effect on the vasculature. It causes a powerful adrenergic response by inhibiting norepinephrine reuptake at nerve terminal, as evidenced by increased heart rates and vasoconstriction.4 Within 10 minutes of entering the body, cocaine can reduce splenic volume by 20% causing end organ ischemia, tissue infarction and damage. The effect produced by cocaine is non-dose-related, as the spleen-volume changes are known to occur at plasma cocaine levels that are often encountered in intranasal cocaine users.3,6,7
The mechanism behind splenic bleeding seems to be initially triggered by the vasospasm induced by cocaine which leads to ischemia and infarction of the parenchyma of the spleen, eventually resulting in vascular rupture.8 Furthermore, increased abdominal venous pressure caused by coughing, for example, could be an instigating event for splenic hemorrhage.9
The first case report that details hemoperitoneum caused by ASR following cocaine use by a 42-year-old male was first described in 2013.10 Since then, searching the English-language literature using PubMed yields only three more cases.11,12,13 Our patient was the oldest ever registered at the time of his ASR diagnosis and only the second case that required surgical management, as the previous ones where stable enough to be either managed conservatively or by angiography with coil embolization.
Conclusion
Although uncommon, after ruling out neoplastic, infectious, and inflammatory processes, one should consider drug related ASR. A detailed social history may be very helpful raising the hypothesis of cocaine induced ASR.
Since early diagnosis and treatment can produce a positive outcome, emergency physicians should be made aware of this pathology.















