Introduction
MEC is a tumor usually seen in the major and minor salivary glands, also occurring in the breast, lacrimal glands, thyroid, thymus, esophagus, bronchial tree, pancreas and skin.1,2 MEC of the breast is an exceedingly rare entity, with little over 40 cases described in the literature, arising in adult women ranging from 29 to 80 years old.3 This neoplasm has distinctive histologic features with a particular genetic translocation.3 Despite this knowledge, characteristic radiological features of this entity are still lacking in the literature. In this paper, we present what we believe is the youngest patient diagnosed with MEC of the breast, among the cases reported to this date.4
Case-Report
A 15-year-old young woman presented with hematic left nipple discharge, mainly occurring at night, with no other remarkable findings. There was no family history of carcinoma of the breast. No axillary lymph node swelling was found.
Breast ultrasound (Fig. 1) showed slight retroareolar duct ectasia (2.5 mm) in the left breast, and a 9 mm solid hypoechoic nodule in the transition of the inner quadrants, classified as a BI-RADS 4A lesion.
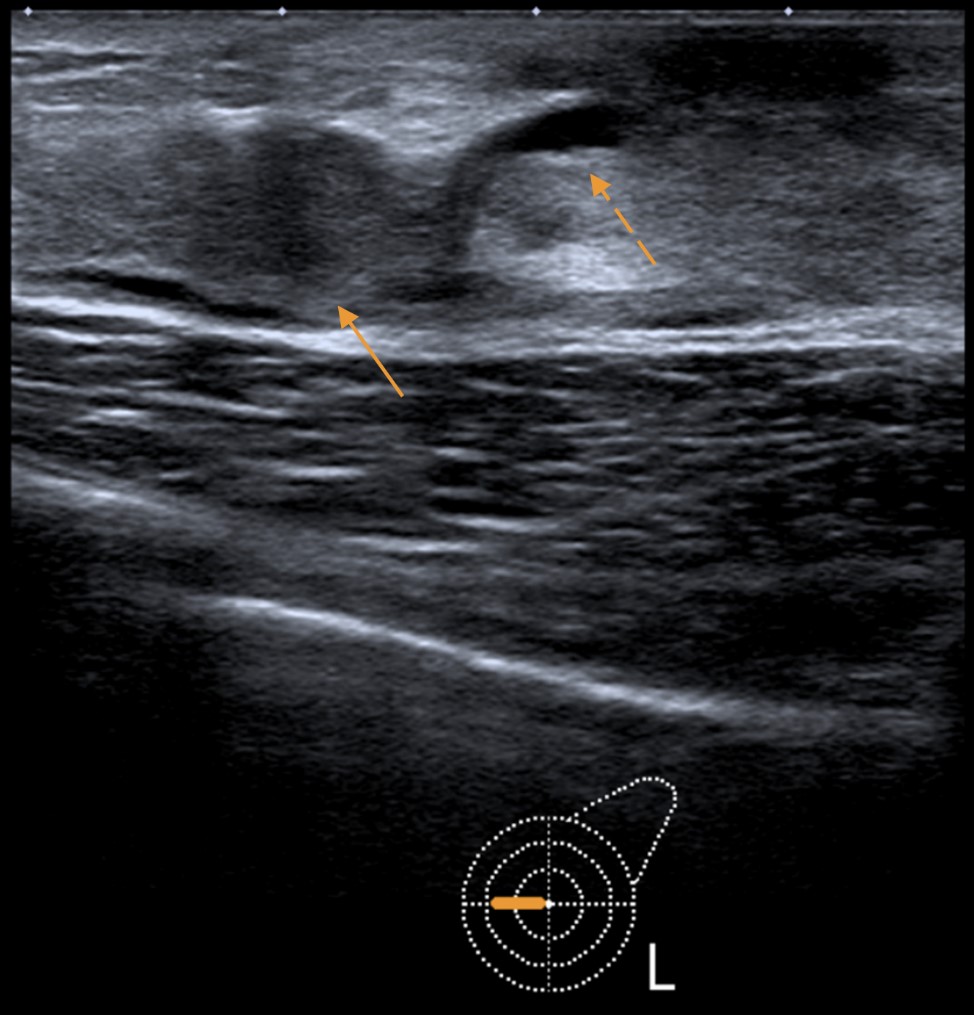
Figure 1: Breast ultrasound revealed a 9 mm hypoechoic, solid nodule (solid arrow), associated with slight duct ectasia (dashed arrow).
Core needle biopsy was performed and histopathological evaluation revealed morphologic and immunohistochemistry features compatible with invasive carcinoma, suggestive of secretory carcinoma of the breast. However, histopathological sample reassessment suggested MEC (which was later confirmed after lesion excision - see figure 5).
Contrast-enhanced breast MRI (3T) revealed the infracentimetric, enhancing lesion in the periareolar region at the transition of the left inner quadrants, initially detected on ultrasound. An additional 6 mm nodular lesion with similar enhancing pattern, located about 11 mm posteriorly and medially, in the same breast quadrant was found (Fig. 2).
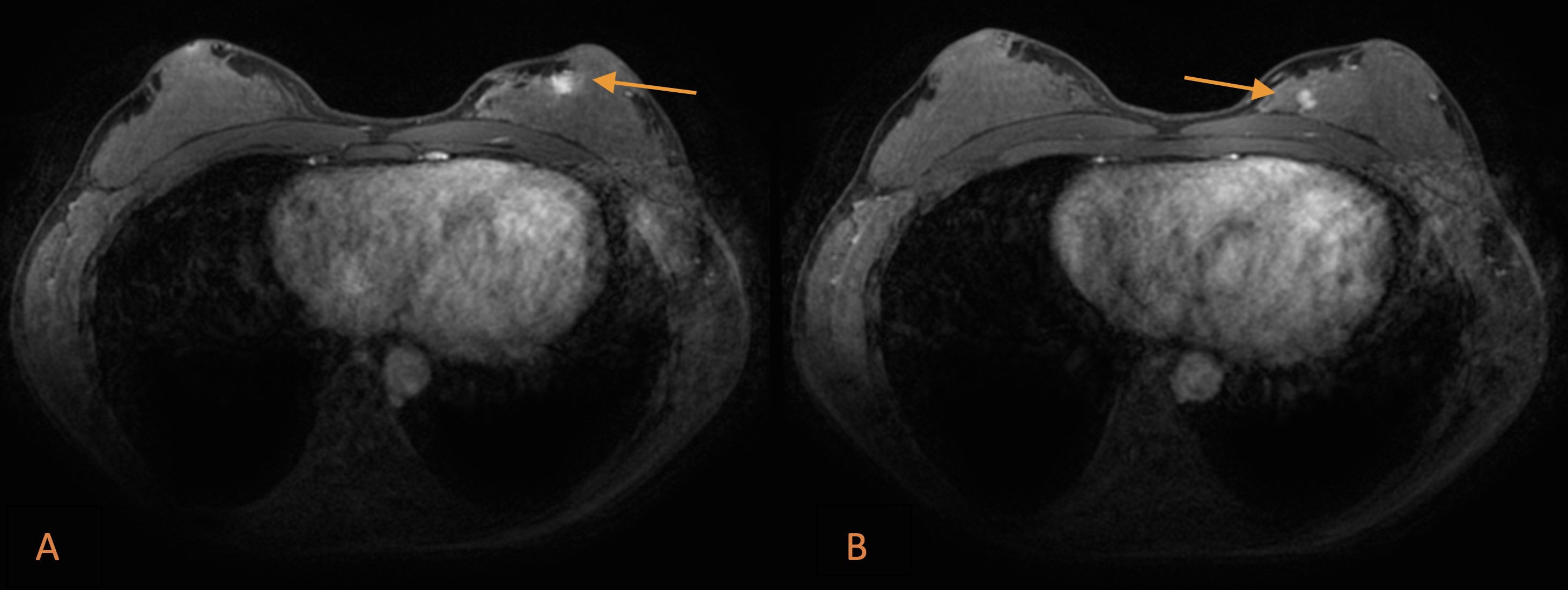
Figure 2: Breast MRI: T1-weighted fat-suppressed, contrast-enhanced sequences revealing the infracentimetric lesion initially detected by ultrasound, enhancing in the periareolar region (arrow in A). An additional 6 mm nodular lesion in the same breast quadrant was detected (arrow in B).
Second-look ultrasound (Fig. 3) showed this additional lesion as a round, apparently solid nodule, with slight posterior acoustic enhancement. Core needle biopsy also revealed MEC.
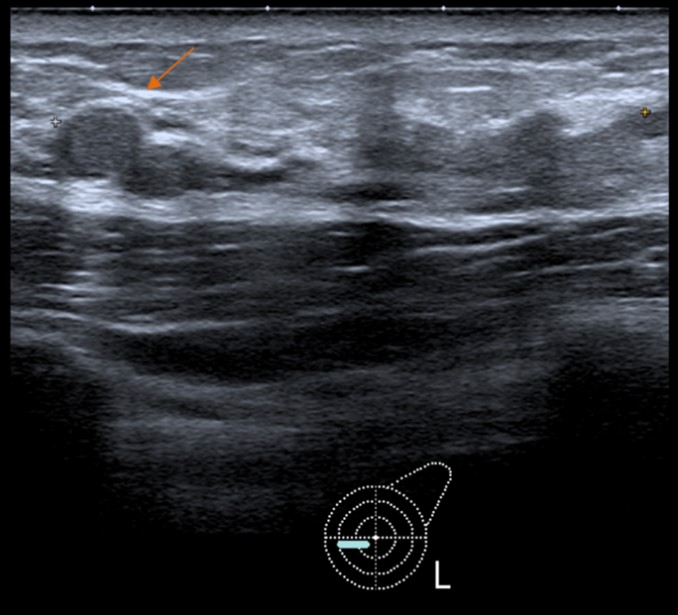
Figure 3: Second-look ultrasound depicting the additional lesion as a round nodule - core needle biopsy also revealed MEC of the breast.
These lesions were submitted to wire-guided localization and a control mammography was performed. Subsequently, the patient underwent partial mastectomy and sentinel lymph node biopsy.
The surgical specimen was sent for pathological evaluation. At gross section, a solid, poorly-delimitated mass of greyish appearance was found, measuring 1cm (Fig. 4).
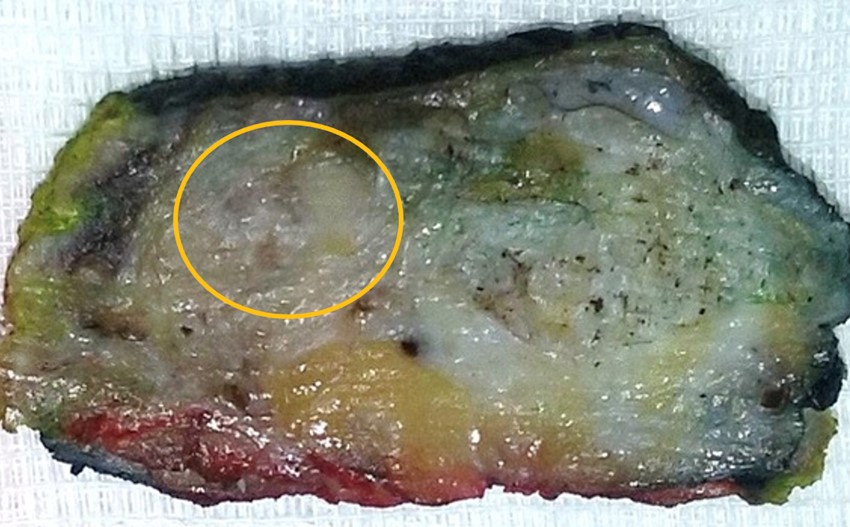
Figure 4: Surgical specimen: a poorly defined greyish nodule with 1cm (circle) was seen at gross section in a background of dense breast tissue.
Histopathological evaluation showed a tumor with cribriform and microacinar architecture embedded in a sclerotic stroma, with three different cells populations: mucinous, squamoid and intermediate cells (Fig. 5). No signs of true keratinization or high-grade features were found.

Figure 5: Microscopic sections showed a tumor with cribriform/microacinar architecture in a background of stromal sclerosis. The majority of cells showed round nuclei and abundant eosinophilic cytoplasm. Peripherally, cells with small uniform nuclei and dense cytoplasm were seen. Presence of extracellular and intracytoplasmic mucin was observed. (HE, x100).
Immunohistochemically, CK7 presented strong positivity in mucinous cells while p63 a CK14 stained both intermediate and squamoid cells. CD117, HER2 and hormonal receptors were negative. A MAML2 gene rearrangement was detected by FISH in 76% of the analyzed cells.
Considering all the aforementioned features, the diagnosis of grade 2 mucoepidermoid carcinoma of the breast was made.
Surgical margins were quite narrow in the lateral and inferior aspects of the specimen; therefore, widening of the margins was performed successfully, with additional foci detected.
Sentinel lymph node procedure revealed no extension of the disease.
Follow-up enhanced MRI revealed no relevant changes.
A multidisciplinary group decision (backed up by literature review) of surveillance and follow-up was made. The patient remains asymptomatic during a follow-up period of 66 months so far, with no signs of recurrence to this day.
Discussion
MEC is a malignant tumor mainly occurring in the salivary glands, but also described in other body parts.1,2 Primary MEC of the breast is a rare entity, first described in 1979 by Patchefsky et al,5 with distinctive morphological features and a few cases reported with molecular studies.3 In the literature, only 42 cases of MEC (including this one) have been reported in English literature.2,3,4 All cases referred to women aged 29-86 years1,2,4, which means this is the case report of the youngest patient diagnosed with MEC of the breast, to this day.
Breast glandular tissue and salivary glands are both exocrine glands, with elements derived from embryonic ectoderm4 - this common origin may explain morphological similarities shared by some of these tumors,6 however, the exact pathogenesis of MEC in the breast remains unclear. Histopathologically, MEC of the breast is similar to its salivary equivalent, which is composed of intermediate, epidermoid and mucinous cells.2,4,6
Immunohistochemistry of MEC of the breast usually shows a basal-like and triple-negative immunophenotype (negative estrogen, progesterone and HER-2 receptors),4 but with a better prognosis than other triple-negative breast cancers.4
Imaging characteristics are diverse and not extensively documented.1 MEC of the breast has been described as a mass with irregular margins, a nodule with well-circumscribed margins or mimicking a complex or simple cyst in ultrasound.1 Our case presented with a multifocal, nodular morphology, with relatively well-circumscribed margins.
MEC has been graded according to the same grading system applied for MEC of the salivary glands7 or by the Nottingham grading system used for invasive breast carcinomas.8
MEC with low/intermediate grade or grade 1/2 have usually a good prognosis and these patients may be potentially cured by complete resection.3 Additionally, axillary metastases are rarely observed, with no evidence of distant metastases in these cases.4,7
In contrast, high-grade MEC are a heterogeneous group of different complex lesions and usually show an aggressive behavior,4,7 with axillary lymph nodes and distant organs metastases.3
This young patient was treated with complete tumor excision and remains asymptomatic until this day, with a 5-year follow-up period and a good prognosis.
Conclusion
MEC of the breast is an extremely rare entity with distinctive histologic and genetic features, that has similarities with its salivary counterpart, but with no particular radiological characteristics. This paper documents the diagnosis of MEC of the breast in a 15-year-old woman who underwent partial mastectomy and remains asymptomatic - the youngest presentation of this entity in the literature up to date.















