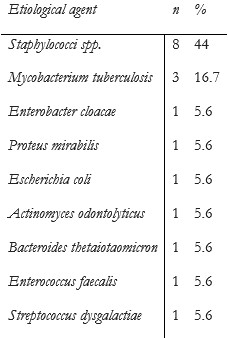
Introduction
The evolution of neuroimaging techniques has allowed better understanding and characterization of spine lesions. Yet, the low specificity of imaging examinations still requires histopathological confirmation of diagnosis. Open biopsy was not long ago considered to be the gold-standard for the diagnosis of bone lesions, but obvious procedural risks, as high as 17%, and the risk of missing small lesions, have led to the development of less invasive techniques.1
Percutaneous biopsy of musculoskeletal lesions has several advantages over open surgical biopsies including lower morbidity, higher cost effectiveness, and fewer complications. Contributing factors for the success rate of percutaneous biopsy procedures include location and type of lesion, needle system and use of different modalities of imaging as well as the physician’s expertise.2
We conducted a retrospective analysis to evaluate the diagnostic yield and safety of percutaneous vertebral biopsies performed in our center, between the years 2016 and 2019.
Materials and Methods
We performed a retrospective search using our prospective database of consecutive patients who underwent spinal biopsy between January of 2016 and December of 2019.
Electronic medical records were reviewed for the following information: demographic distribution, supporting imaging techniques (fluoroscopy and CT), vertebral segment (cervical, thoracic, lumbar, sacrococcygeal/iliac bones) and location of biopsy (vertebral body, pedicle, disc, spinous process, paravertebral), histopathological results (primary malignant tumor, metastasis, benign tumor, inflammatory/infectious, reactive bone changes, without pathological changes, insufficient sample), adjunct treatment (with or without vertebroplasty) and complications.
We used two different imaging modalities: fluoroscopy-guided biopsy and CT-guided biopsy.
The biopsies were performed under fluoroscopy GE Innova 2121IQ (Biplanar) and Siemens Artis Q (Biplanar), as well as GE LightSpeed CT (fig.1).
All procedures were performed by four experienced interventional neuroradiologists at our center.
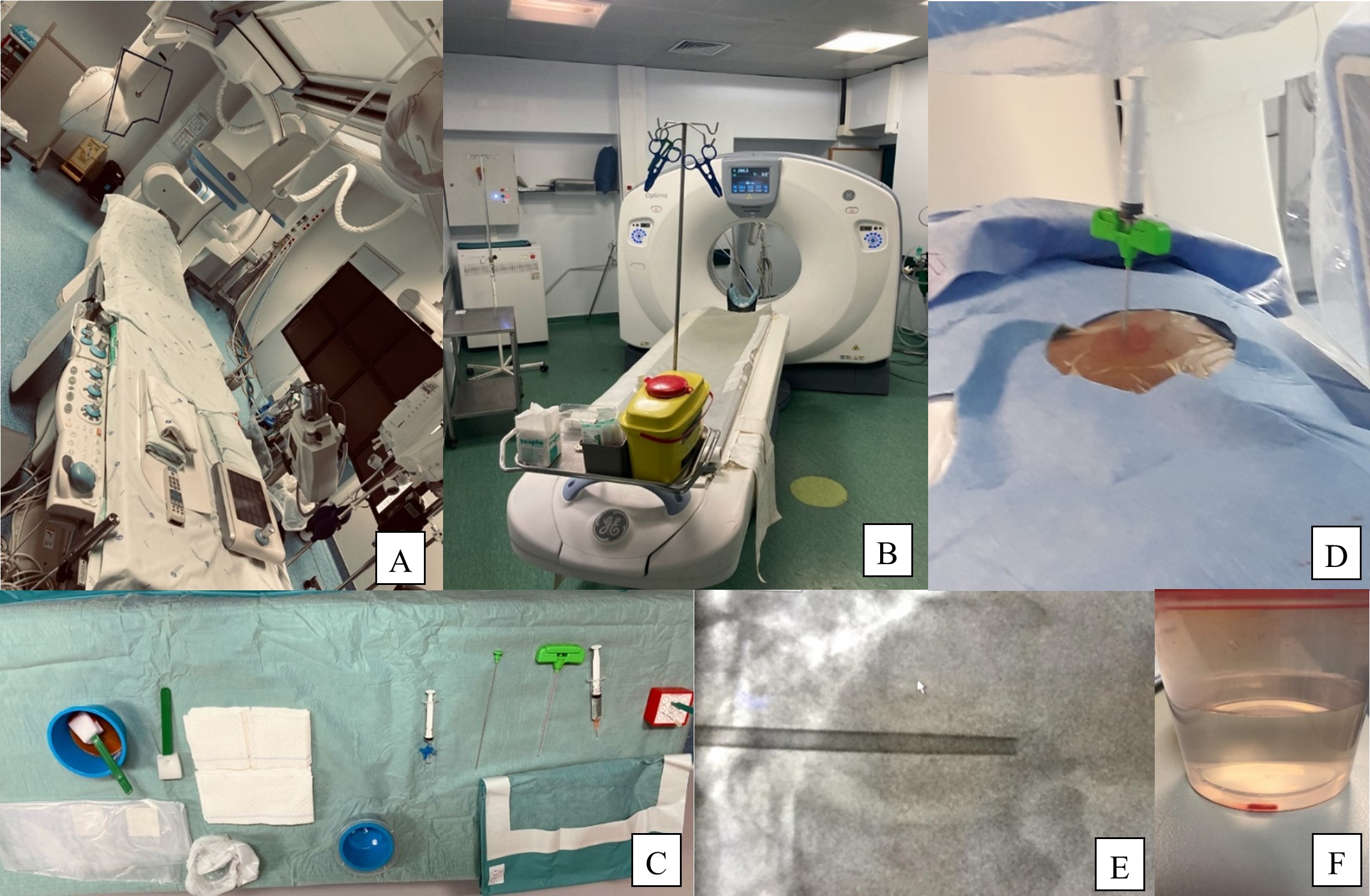
Figure.1: (A) and (B) Angio suite of our Department in Hospital de São José, CHULC. (C) Common table setup for our spinal biopsy procedures. (D) Positioning of the biopsy needle and the syringe for suction effect. (E) Lateral fluoroscopy projection depicting the depth of needle progression in the vertebral body. (F) Osteomedullary fragment collected in a formol container.
The study was designated a clinical audit, and no ethics committee review was required. The anonymized data that support the findings of this study are available from the corresponding author on request.
Results
From January 2016 to December 2019, 240 biopsies were included in our study. 102 were female and 138 were male, 42.5% and 57.5%, respectively. Fluoroscopy guided biopsy was used in 237 of procedures.
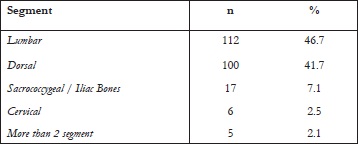
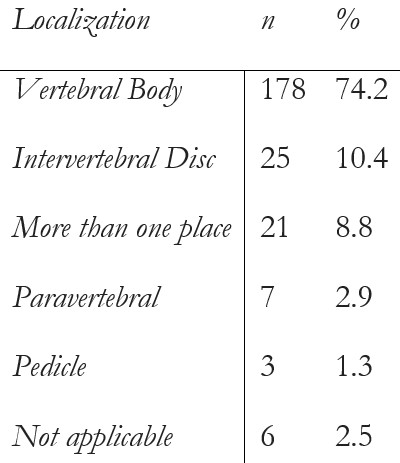
The lumbar spine was the most frequently biopsied segment (n=112), followed by the thoracic spine (n=100) (table 1). Most of the specimens were collected from the vertebral body (n=178) (table 2), followed by intervertebral disc and more than one site biopsies (e.g: disc and body, body and pedicle).
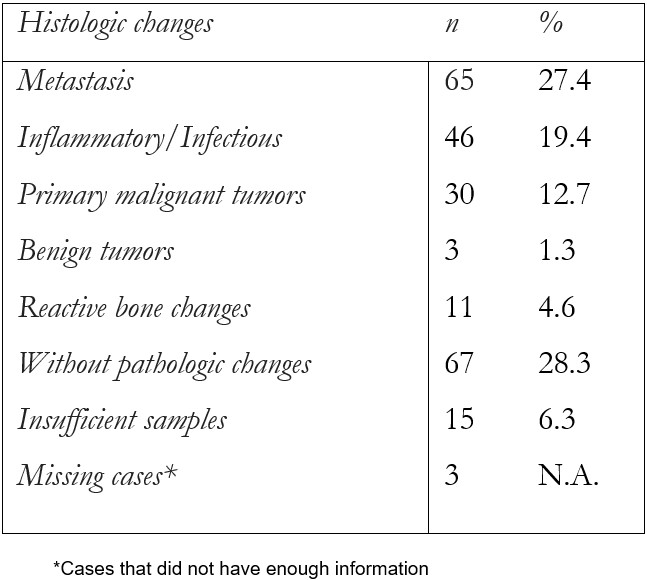
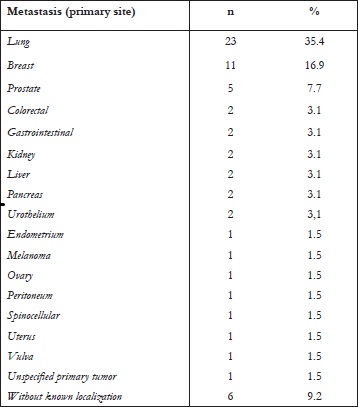
Out of the 240 specimens, the most frequent histological findings were bone metastasis (n=65) (table 3), and lung (n=23) was the most common primary tumor (table 4). After metastasis, inflammatory/infectious changes (n=46) were the second most frequent finding, and Staphylococci sp. was the most isolated species (n=8) (table 5). Of the 46 patients with infectious changes, we obtained positive cultural /microbiological results in only 18 (39%).
Considering the primary malignant tumors (n=30), bone marrow tumors represented almost all cases (n=29), including multiple myeloma, Ewing sarcoma and lymphoma; chondrosarcoma was found in one of the 30 cases. Few benign tumors were found (n=3) - one hemangioma, one nerve sheath tumor and one meningioma.
Less than a third of the samples (28%, n=67) had no pathological changes, and 4.6% (n=11) showed reactive bone changes. Fifteen samples (6.3%) did not have enough tissue for a conclusive histopathological result.
There was one complication (representing 0.4% of all cases), a dural laceration, which was managed medically, with no clinical sequelae.
As adjunct treatment, some patients were submitted to vertebroplasty in the same procedure (n=46). Pathological fractures of vertebrae presenting with acute/subacute pain, in conjunction with findings of bone edema in STIR (short-tau inversion recovery) MR imaging were treated with vertebroplasty.
Out of the 240 biopsies, 18 (7.5%) had to be repeated, 14 of which (78%) had diagnostic yield.
To collect larger amounts of tissue, whenever a biopsy was repeated, different access/side was used in the same vertebral body, or a different vertebral body was approached in cases of diffuse spine lesions. A three-way valve and aspiration were used for increased suction effect, and in some cases, CT- /flat-panel CT guided biopsy was performed for better anatomical depiction during biopsy. The diagnostic yield in this study was 92.5% (n=222).
Discussion
Our series describes a tertiary center experience in non-invasive spinal biopsies, with a diagnostic yield of 92.5% (n=222), and a very low rate of complications (0.4%), which confirms the efficacy and safety of this percutaneous biopsy as an alternative to open surgical biopsy.
The diagnostic yield of the biopsies performed at our center is in line with the literature. A study conducted by Wu et al. reported 151 percutaneous biopsies of bone and soft-tissue lesions under CT and ultrasound guidance and attained a diagnostic yield of 77%.3 Similar results were obtained by Yang et al. focusing on spinal tumorous lesions, showing a percutaneous image-guided biopsy diagnostic yield of 80%.4
However, in infectious spine disease, the diagnostic yield is comparably lower. Of the 46 patients with infectious changes, we obtained positive cultural /microbiological results in only 18 (39%). The same findings were described by Nam et al: false-negative results were explained by inadequate amount of specimen, inadequate extraction devices, sampling error, and empirical antibiotics at the time of the biopsy.5
According to reviewed literature, open biopsies can reach 87.5% of adequate sampling for histopathological analysis, although with much higher complication rates, up to 10-15%.6
There is little information in the literature about adjunct vertebroplasty or kyphoplasty post-biopsy procedures for vertebral lesions. Nevertheless, this is a viable option whenever patients fulfill criteria for treatment, namely vertebral compression fracture, persistent pain with a grade of >40% in Oswestry disability index (major disability) and ≥40% collapse of the vertebral body.7 We performed adjunct treatment with vertebroplasty in 19% of cases following biopsy, in order to stabilize pathological fractures and palliate pain.
Despite using a prospective database, this retrospective study might have some limitations such as data that was not available in clinical records. Selection bias may be present since biopsies performed at our center are generally referred to us by other clinicians. Another limitation is the variability in histopathologic results, from infectious diseases to cancer, rendering a wide range of pathology, that can alter the results, especially the diagnostic yield. Additionally, we considered the whole spine with all vertebral segments involved, each posing unique challenges and complicating result interpretation.