Background
Splenosis is an acquired benign condition that refers to the heterotopic autotransplantation of splenic tissue following splenic trauma or splenectomy, whose incidence is unknown. The most affected locations are the peritoneal and pelvic cavities by contiguous spread, but there are cases described in the brain and heart, via hematogenous dissemination. Most patients are asymptomatic, and it is often found incidentally. If symptomatic, clinical presentation varies according to the affected site. Splenosis can radiologically mimic other conditions requiring differentiated imaging methods for its definitive diagnosis.1,2 We present the case of peritoneal splenosis mimicking peritoneal carcinomatosis.
Case Report
A 56-year-old male with cardiomyopathy with left ventricular hypertrophy, precapillary pulmonary hypertension, atrial fibrillation, arterial hypertension, dyslipidemia, obesity, alcohol consumption and a history of splenectomy over 30 years before, following trauma, presented with increase in abdominal perimeter and unspecific abdominal discomfort lasting for several months. Upon physical examination, clinically evident ascites was noted.
Laboratory work-up revealed no abnormalities in the complete blood count and no evidence of coagulopathy. There was an elevated aspartate aminotransferase (40 U/L) and gamma-glutamyltransferase (328 U/L) (Reference Range: 10-34 and 10-66 U/L, respectively). Serologies for human immunodeficiency virus, hepatitis B and C viruses were negative. Autoimmune hepatitis, alpha-1-antitrypsine deficiency and hemochromatosis were excluded. Abdominal ultrasonography and contrast-enhanced computed tomography (CT) revealed hepatomegaly with signs of congestion, including massive ascites, and a heterogeneous aspect of the mesenteric fat with multiple unspecific isodense round/oval nodules, but no evidence of a primary tumor. A diagnostic hypothesis of peritoneal carcinomatosis was formulated.
Peritoneal histologic and cytologic assessment were negative for malignancy. Endoscopic studies, thoracic-abdominopelvic CT and [18F]F-FDG Positron Emission Tomography/CT (PET/CT) did not find suspicious neoplastic lesions.
After multidisciplinary discussion and given the patient’s history of splenectomy, a diagnosis of splenosis was considered. A 99mTc-heat-denatured red blood cells (99mTc-DRBC) Single Photon Emission (SPECT)/CT (Fig.1) enhanced multiple and scattered foci with increased radiotracer uptake within the peritoneal cavity, that were coincident with the known unspecific abdominal nodules on CT (Fig.2) with variable size, confirming the splenosis hypothesis.
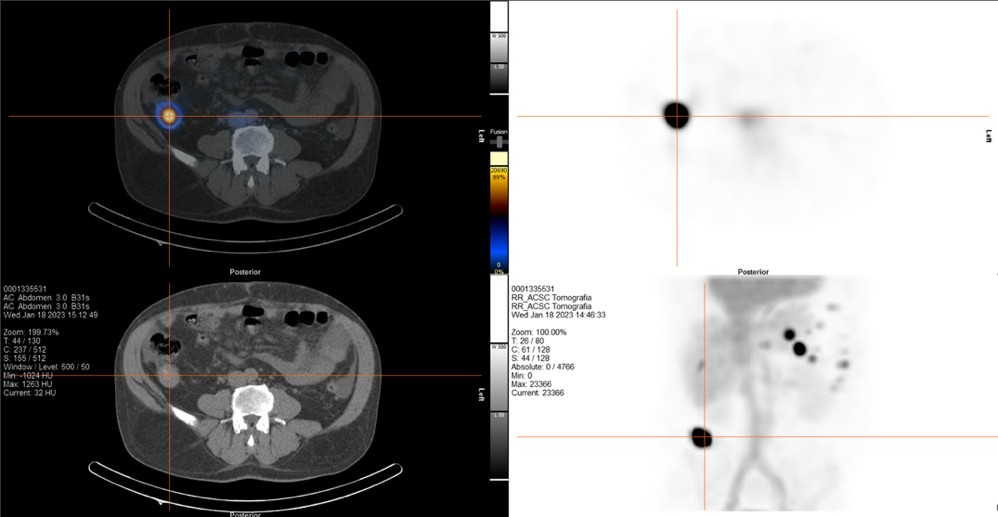
Figure 1: 99mTc-DRBC SPECT and MIP image (top right and bottom right) showing multiple and scattered abdominal foci with increased radiotracer uptake that can be fused with CT morphological image (bottom left), displaying hybrid SPECT/CT (top left), consistent with splenosis.
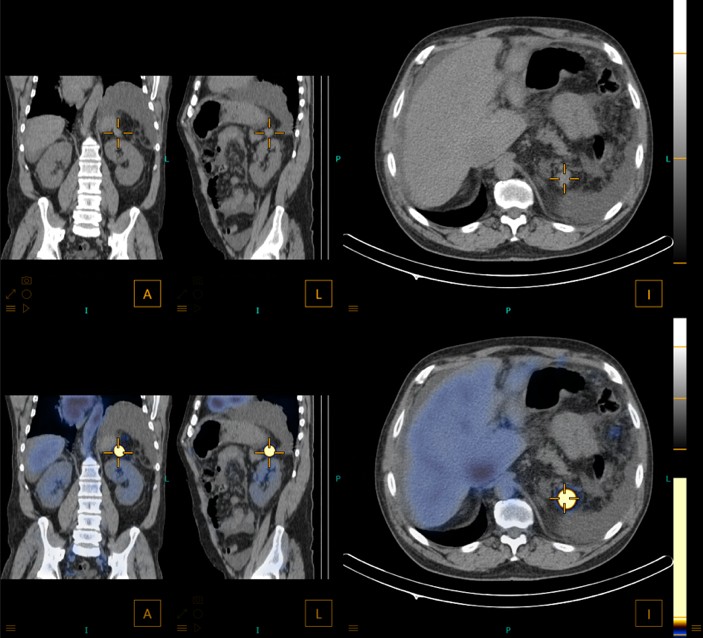
Figure 2: Nodule measuring 20x19mm posterior to the stomach on morphological images (non-contrast CT; top line) that is coincident with the foci with increased radiotracer uptake on 99mTc-DRBC SPECT/CT (bottom line).
After excluding malignancy, the patient started diuretic therapy on behalf of decompensated chronic liver disease, with resolution of ascites and abdominal discomfort.
Discussion
This case highlights the consideration of splenosis as a possible cause of unspecific abdominal nodules, as it may mimic poor prognostic conditions, such as peritoneal carcinomatosis, especially when there is no evidence of primary malignancy and there is a previous history of splenic rupture or surgery. The use of non-invasive functional imaging, such as 99mTc-DRBC SPECT/CT, may reveal its definitive diagnosis.3 This case further emphasizes the importance of a multidisciplinary approach involving medical, surgical and imaging teams.















