Introduction
Grisel syndrome (GS) is a rare entity that corresponds to a non-traumatic atlantoaxial rotatory subluxation (AARS), usually secondary either to an infection of the upper airway or a head and neck procedure.1,2 Although infective causes seem more predominant,1 and retropharyngeal abscesses are quoted as possible causes of GS, there are scarce reports in the literature of this syndrome as a consequence of a parapharyngeal abscess.3,4)
This syndrome has no apparent gender predominance and is seen almost exclusively in children and young adults, with more than 90% of cases presenting before 12 years of age.5 Although the pathophysiology is not yet completely understood, the most credited theory states that it may be secondary to hematogenic propa gation of inflammatory mediators from the pharynx to the stated ligaments, through venous plexus, causing abnormal relaxation and laxity.6 Risk factors for this en tity correlate with risk factors for greater atlantoaxial ligamental instability like younger age and syndromes like Down syndrome, osteogenesis imperfecta, or neurofibromatosis.6,7 Patients usually present with torticollis, and a high index of suspicion is needed for correct diagnosis.1
We report a case of a 6-year-old male patient presenting with odynophagia and torticollis to the emergency ward.
Case report
A previously healthy 6-year-old boy was referred to our emergency ward with a 2-day-duration odynophagia complaint, associated with painful torticollis and fever. There was no report of drooling, trauma, or other relevant symptoms. On physical examination, there were no observable alterations at oral and pharynx examination.
Multiple painful right cervical adenopathies were palpable, with approximately 3 cm diameter and the child had a preferential head position of head rotation to the right. Neurological examination revealed no findings on assessment of muscle power, cranial nerve functions, tendon reflexes, and sensory deficit.
Cervical echography confirmed multiple adenopathies, with a greater diameter of 3 cm, without necrosis or other findings. As this technique does not allow us to study the cervical spine, we proceeded to order a computed tomography (CT) scan with associated contrast. This revealed a parapharyngeal abscess of 1 cm of greater diameter, associated with an atlantoaxial subluxation, with right rotation, and an anterior displacement of 3 mm, configuring a type II of Fielding (Fig.s 1, 2 and 3). Blood samples were collected revealing leucocytosis with neutrophilia and CRP elevation.
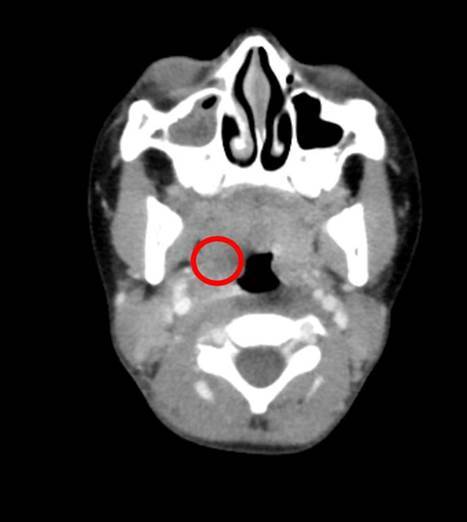
Figure 2: Axial view of CT scan. Parapharyngeal abscess associa ted with contiguous retropharyngeal edema.
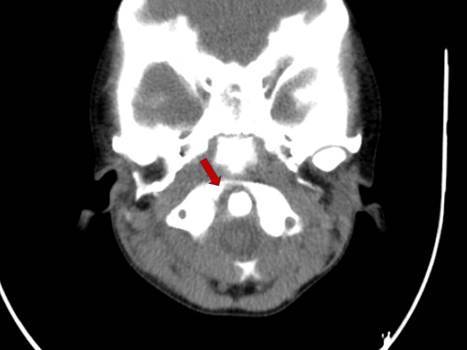
Figure 3: Axial view of CT scan. Atlanto-axial subluxation, sho wing right rotation, and an anterior displacement of 3 mm (type II of Fielding).
A conservative approach was adopted. The child was admitted to our hospital for completing an one-week antibiotherapy course of endovenous ceftriaxone and clindamycin adjusted to weight and age, associated with anti-inflammatory, with no need for surgical drainage, due to the abscess dimension. Measures of cervical im mobilization with cervical collar were also instituted. After one week, symptoms were frankly better, and so the child was discharged maintaining the cervical collar until the reevaluation consultation. This was performed at 6-weeks with a complete resolution of symptoms and of subluxation on dynamic x-ray. At one year follow-up, the child presents no limitation of movements, torticollis or other sequels.
Discussion
Grisel syndrome is a rare entity. In a systematic review of all the published cases, 48% were stated as infectious while 40% as post-surgical, going against the previous belief of surgery as the major causative factor. The most frequently stated infections are upper airway infections,1 being a parapharyngeal abcess a possible cause, yet rarely mentioned in published case reports. It usually affects children and patients with any syndrome that affects ligaments, such as Down’s syndrome.7,8 Our pa tient had no predisposing factor other than his age.
Pathophysiology is still up to much debate. The atlantoaxial joint is complex, and its most important characteristic is allowing rotation. The transverse ligament, the most important stabilizer, prevents anterior dislocation of the atlas on the axis, while the alar ligament prevents excessive rotation. When these ligaments are inflamed, they may become loose and cause excessive rotation and subluxation.2 Pharyngovertebral veins that drain to periodontal plexus were identified and might help in the hematogeneous progression of edema and inflammatory mediators, leading to this clinical picture.9 Battiata et al described a double-hit hypothesis, where a pre-existing risk factor for augmented ligamental luxation should exist before ligament inflammation.10
Symptoms and signs for GS include torticollis, dyspha gia, and most patients present with fever. Cock-Robin deformity may be present: the head is tilted ipsilaterally to the subluxation while the chin is rotated to the opposite side. Tenderness and deviation of the spinous process of C2 in the same direction as head rotation (Sudeck sign) may also be present.11 Torticollis in the context of a cervical infection might occur but is usually not as severe as in our case. The cervical spine should be studied, and trauma background assessed. Because all symptoms appeared on the same day, a causal relationship was established between the cervical infection and the observed AARS.
Imaging studies are key on establishing diagnosis. Plain X-ray may be difficult to interpret but in lateral plain, open-mouth radiographs, it might be visible an increased atlanto-odontoid distance (normal atlanto-od ontoid distance is ≤ 5 mm in children). CT scan is the most helpful in diagnosing atlantoaxial subluxation.2 For follow-up, dynamic X-ray can be the used exam.
For classifying its severity, we may use Fielding classification, ranging from type I or II (a luxation that can usually be treated with conservative measures) to III or IV, possibly needing surgical intervention. This classification is based on CT scan findings of subluxation dis tance.12
Treatment with conservative measures, when indicated, may offer complete resolution of the clinical picture within a few weeks. This includes bed rest, reduction and cervical immobilization with a stiff cervical collar, muscle relaxants, and non-steroid anti-inflammatory therapy. Broad spectrum antibiotics should be prescribed initially until the causative organism is identified. Uncomplicated, early treated AARS presents an excellent prognosis.13 Despite this fact, it may be initially overlooked, and a high index of suspicion is needed. In our case, these conservative measures were timely adopted during a course of a 1-week admission, with complete recovery.
There seems to exist a direct connection between diminished time to subluxation’s reduction and better outcomes. Untreated patients may acquire chronic functional and cosmetic deficits. This condition may also progress to neurological compromise (in about 15% of cases) such as paralysis, nerve damage, possibly leading to death. Therefore, early identification and establishment of treatment is of paramount importance.1,13
Our case represents a rarely mentioned etiology for atlanto-axial rotatory subluxation. In the group of head and neck infections, a parapharyngeal abscess is a less probable cause, as the distance from the cervical spine is greater. In Grisel syndrome, the inflammation spreads by contiguity, and this may explain why retropharyngeal abscesses are more mentioned in systematic reviews.1 Our first CT scan reveals a retropharyngeal hypodensity due to edema, being this the probable spreading route until the transversal ligament in our clinical picture.
Conclusion
Grisel syndrome may present in a child with torticollis and recent head and neck procedure or head and neck infection. Otorhinolaryngologists should remember the possible presentations and risk factors for this syndrome, as it follows infections or interventions in their area of expertise. Conservative treatment is often enough, and early identification and immobilization seem to lead to better outcomes.
















