Introduction
In anesthesiology, the team is composed of elements with different levels of training, experience, and skills that work together in an environment with high technological complexity.1,2 Simulation appears as the tool able to suppress the lacunae in traditional education, available for all the residents in anesthesiology.3 To build a simulation program, the needs and the goals of the participants should be defined, as well as the learning objectives.1,2
These facts, together with a difficult learning curve of the different procedures and a potentially high risk for the patients, lead to the development of a complementary education tool, oriented by the pedagogical goals defined by the Portuguese Specialty College.3,4
The implementation of the Portuguese National Pedagogical Plan at the Biomedical Simulation Centre from Centro Hospitalar e Universitário de Coimbra (BSC-CHUC), Portugal, had four main goals: to facilitate the acquisition of theoretical knowledge; to allow the acquisition of technical competencies, to allow the practice of critical situation and to facilitate the team training, communication, and leadership. Therefore, the residents' performance during this simulation course was self-evaluated in its two main components: technical and non-technical skills.5 Besides this self-evaluation of the competencies acquired during the simulation course, and since the National Pedagogical Plan should be implemented to complement the residency in anesthesiology, the program contents should suppress the lacunae that residents faced during their clinical practice. It is fundamental to analyze the importance and satisfaction of each topic included in the simulation course.
This study aimed to evaluate the importance attributed by the participants to each topic of the National Pedagogical Plan which revealed the satisfaction regarding the simulation courses to suppress the needs faced, by the residents, in the clinical practice.
Methods
Study Design
This prospective observational study was designed to evaluate the impact of the Anesthesiology Simulation Pedagogical Plan from BSC-CHUC, in the self-assessment of confidence, behavior, and training of the Portuguese Anesthesiology residents. Each simulation module was designed according to the program contents of each year of the Anesthesiology Residency Program (ARP), and the scripts/scenarios were previously published.4,5 A summary of the main contents of each simulation module is included in Table 1.
Questionnaires included questions about learning, behavior, and evaluation of the pedagogical content of each simulation course. In this paper are presented the results of the importance, attributed by the participants, of the pedagogical content of each simulation course performed after the simulation course (Table 2). The complete questionnaires included were published previously.
Table 1: Summary of the programmatic content of each simulation module.
| Year I | Year II | Year III | Year IV |
|---|---|---|---|
|
|
|
|
|
Table 2: Questionnaires applied in each module for each specific year of ARP. These questions were performed post-simulation courses to evaluate each topic's importance in a simulation context.
| Year I | |
| 21 | Basic Pharmacology in Anesthesiology: topic importance |
| 22 | Basic and advanced airway: topic importance |
| 23 | Ventilation: topic importance |
| 24 | Vascular cannulation in anesthesia: topic importance |
| 25 | Ultrasound in anesthesia: topic importance |
| 26 | Central and peripheral cannulation using ultrasound: topic importance |
| 27 | Neuraxial anesthesia and local anesthetics: topic importance |
| 28 | Simulation training on operation room - clinical cases |
| 28.1 | Topic importance |
| 28.2 | Training impact |
| 29 | Simulation training on post-anesthesia care unit - clinical cases |
| 29.1 | Topic importance |
| 29.2 | Formative impact |
| 30 | Etiology and prevention of cardiorespiratory arrest: topic importance |
| 31 | BLS algorithm: topic importance |
| 32 | ALS algorithm: topic importance |
| 33 | Recognition of rhythms: topic importance |
| 34 | Defibrillation: topic importance |
| 35 | Simulation training on ALS - clinical cases |
| 35.1 | Topic relevance |
| 35.2 | Formative impact |
| 36 | Global evaluation |
| Year II | |
| 37 | Leadership and health management: topic importance |
| 38 | Difficult Airway Algorithm: topic importance |
| 39 | Supraglottic and transcutaneous devices: topic importance |
| 40 | Fibroscopy principles: topic importance |
| 41 | Simulation training on difficult airway - clinical cases |
| 41.1 | Topic relevance |
| 41.2 | Formative impact |
| 42 | Ultrasound in anesthesiology: topic importance |
| 43 | Ultrasound-guided regional blocks: topic importance |
| 44 | Simulation training on ultrasound-guided regional blocks - clinical cases |
| 44.1 | Topic relevance |
| 44.2 | Formative impact |
| 45 | The anesthetic approach of the burnt patient |
| 46 | Simulation training on the anesthetic approach to the burned patient - clinical cases |
| 46.1 | Topic relevance |
| 46.2 | Formative impact |
| 47 | Global evaluation |
| Year III | |
| 48 | Assessment of a trauma patient, head and thoracic trauma: topic importance |
| 49 | Abdominal trauma: topic importance |
| 50 | Massive hemorrhage management: topic importance |
| 51 | Trauma in the pregnant: topic importance |
| 52 | Simulation training on trauma - clinical cases |
| 52.1 | Topic importance |
| 52.3 | Formative impact |
| 53 | Pathophysiology and management of ARDS topic importance |
| 54 | ARDS ventilation: topic importance |
| 55 | Pathophysiology of sepsis: topic importance |
| 56 | Management of a septic patient: topic importance |
| 57 | Simulation training on intensive care - clinical cases |
| 57.1 | Topic importance |
| 57.2 | Formative impact |
| 58 | Anatomy-physiological changes of pregnancy |
| 59 | Labour analgesia |
| 60 | Obstetric emergencies: topic importance |
| 61 | Simulation training on obstetric anesthesiology - clinical cases |
| 61.1 | Topic importance |
| 61.2 | Formative impact |
| 62 | Global evaluation |
| Year IV | |
| 63 | Effective communication: topic importance |
| 64 | ACRM: topic importance |
| 65 | ACRM principle |
| 66 | Simulation training on ACRM - clinical cases |
| 66.1 | Topic importance |
| 66.2 | Formative impact |
| 67 | Emergencies in the Operating room |
| 68 | Simulation training operating room emergencies - clinical cases |
| 68.1 | Topic importance |
| 68.2 | Formative impact |
| 69 | Global evolution |
ARP - Anesthesiology Residency Program; BLS - basic life support; ALS - advanced life support; ARDS - acute respiratory distress syndrome; ACRM - anesthesiology crisis resource management.
Questionnaire’s Development and Validation
The process of development and validation of questionnaires were previously described and published.
Setting and Participants
This study was an observational study conducted in Portugal, from 2011 to 2018, at BSC-CHUC. The same simulation courses of BSC-CHUC were offered since February 2011. The simulation environment included 3 simulation rooms: an operating room, a recovery room, and an emergency room. Four participants were included in each section with the roles of senior fellow (1st help), fellow, and 2 residents. The residents were active in “hot-seats”. The script of the scenarios5 is related to the content of each module, described in Table 1. Annually, approximately 15 residents of each year participate in the course. Simulation courses were performed during the first trimester of each specific year.
Participants were Anesthesiology residents enrolled in the simulation courses at BSC-CHUC.
Inclusion criteria: All anesthesiology residents enrolled in the anesthesiology simulation courses at BSC-CHUC. Exclusion criteria did not exist.
Ethical approval for this study (Ethical Committee Nº 171/ CES) was provided by the Ethical Committee from CHUC, Coimbra, Portugal (Chairperson Prof. Doutor João Pedroso de Lima) on 18 July 2019. Accordingly, written informed consent has been waived by the Ethical Committee.
Variables and Method of Assessment
All variables were collected on an anonymized database specifically designed for the study. The source of all the variables was the specific questionnaires applied after each simulation course. Answers were given on an eleven-point Likert scale (0-10, ranging from null to maximum).
Results
Three-hundred and forty-four validated questionnaires were included in the study: 76 from the year I, 89 from the year II, 82 from the year III, and 93 from the year IV. The mean age of the residents in the first year was 26.5 years of age with a minimum of 25 years and a maximum of 29 years.
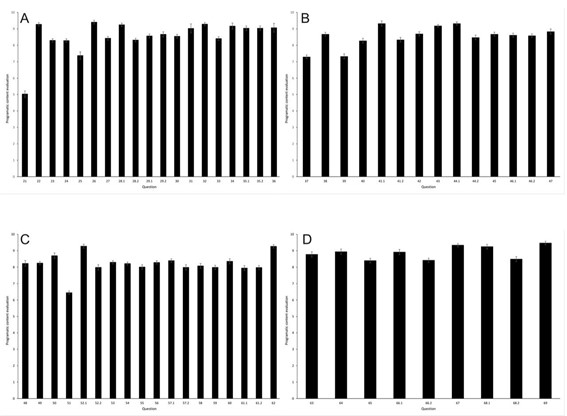
The mean of the resident assessment for each question of Table 1, regarding programmatic content importance, is represented in Fig. 1. Fig. 1 is grouped in four panels corresponding to each year of the simulation module: Panel A: the year I; Panel B- year II; Panel C- year III and Panel D- Year IV.
Discussion
Our study demonstrated that programmatic contents included in the simulation courses of the National Pedagogical Plan are important and satisfied the needs of residents in anesthesiology. This is of paramount importance since for a complete residency with high-quality standards, all these matters should be addressed, preferably in a safe environment, as simulation training permits.
The perceptions about the role of simulation in anesthesiology training are well documented. Simulation has a positive effect on the technical and non-technical skills of the students, namely in anesthesiology residents.5-8
Our results are part of a study that englobes technical and non-technical skills training in anesthesiology, in which the impact of a 4-year simulation course designed specifically on curricular goals defined for the Portuguese Anesthesiology Residency Program was evaluated. For that, the simulation modules were proposed to be performed in the first trimester of each year. This is an unique way, allowing to accomplish the main objective of simulation: to learn in a safe environment, without risk for the patient,7 since the first contact with each programmatic content occurs in a simulation environment. Simulation-based training is resource-intensive and there is a need to prioritize the contents and to adapt the courses to the immediate needs and lacunae of the participants,1,2 therefore, it is crucial to understand the perception and satisfaction of the students about the contents included in the simulation training. This is the reason why, in this paper, we presented the evaluation performed by the students of the importance of each pedagogical included in each simulation module. Thus, the questions were only answered after participation in the simulation course.
From the analysis of Fig. 1, we can conclude that is essential for the students to practice each of the programmatic content in a simulation context, including the clinical cases in which the students evaluated the formative impact beyond the topic importance.
The year I was the one in which more programmatic contents were addressed and consequently had more questions. Basic pharmacology in Anesthesiology is the topic to which was given less importance: with a mean of approximately 5 and a low dispersion, showing a high concordance between the students. Interestingly, this topic was not included in the final prioritized list of 30 procedures’ groups for simulation in anesthesiology, recently developed by a Consensus Panel.2 Nevertheless, the study of pharmacology in anesthesiology has been associated with more effective learning and long-lasting retention compared to lectures alone.9 The global evaluation of the course of the first year is very high.
In year II, different topics were approached. The global evaluation was very positive, and only questions 37 and 39 had a numerically low evaluation, approximately 7. Question 37 can be interpreted as a behavior question: leadership and health management are non-technical skills. Leadership and health management focus on interprofessional team training in healthcare education, together with communication and situation awareness.1 For good leadership and management, participants should interact with each other, with the environment, and with the manikin ("patient").1 The evaluation performed by the students could reveal some immaturity since they are at the beginning of their second year and are concerned with technical skills. Nevertheless, it is proven that simulation-based training has the advantage of improving self-confidence, situation awareness, communication, and leadership.5,9
Question 39 is related to supraglottic and transcutaneous devices. These devices are an essential second and third-line tool during difficult airway management after a failed tracheal intubation and require sufficient training. Moreover, they are related to a procedure included in the recommended final list of 30 prioritized procedures for the simulation-based training in anesthesiology.2 Although the indications for using these devices and their prominent role in managing the difficult airway, they are not widely used.10 A recent study showed that the feasibility of simulation for this training depends on the type of manikin.11 Therefore, the students' previous knowledge about the scarce use of these devices and a more appropriate manikin could impact the importance given to this theme.
As in year I and year II, the students' general evaluation of year III was very good. Trauma in pregnancy was the only topic with a mean of less than 7. It is estimated that trauma complicates approximately 1 in 12 pregnancies being vehicle crashes and falls due to instability, the predominant causes of reported trauma during pregnancy. The management of trauma in pregnant women should be done to minimize maternal injury, leading to maternal stabilization.12 However, in this situation, the medical doctors must deal with a higher stress situation, and simulation could be of extreme importance. The lower importance rating given by residents relate to the fact that, initially, a traumatically injured pregnant woman should be treated as their nongravid counterparts, and therefore the general management of trauma is more important to be included in simulation courses than the management of trauma in pregnancy.
Year IV is the last year of the residency. In the simulation modules of this year, ACRM - Anesthesia Crisis Resource Management, including communication and emergencies in the operating room, are the main explored concepts. All the questions were evaluated by the students with a high score (more than 8), meaning that in the last year of their residency, when exposed to the more challenging situations, they found the learning process based on simulation crucial.
Some limitations of this study have been noted. First, methodologically, and for a more concise analysis of the simulation courses' impact on the residents' learning process, a pre-course questionnaire should be applied to the students. Only with these pre- and post-course results we could analyze how the importance attributed to each programmatic content change due to the simulation course. To overcome this, questionnaires should be applied before and after the courses in future simulation courses.
Conclusion
This study showed that from the anesthesiology residents' point of view, most of the topics included in the simulation modules are of utmost importance and should be included in the simulation courses. This allows the residents to fulfill their educational needs, faced in the clinical practice, in a safe environment.